| True hermaphroditism | |
|---|---|
| Other names | DiseasesDB = 29664 |
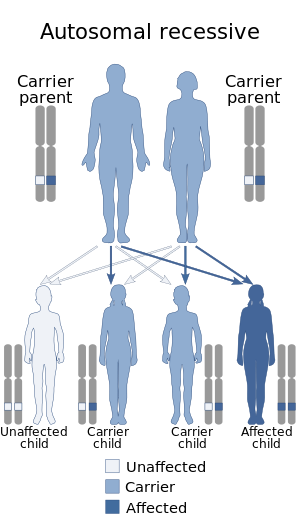 | |
| This condition is inherited in an autosomal recessive manner | |
| Specialty | Obstetrics and gynaecology, endocrinology |
True hermaphroditism, clinically known as ovotesticular disorder of sex development, is a medical term for an intersex condition in which an individual is born with ovarian and testicular tissue. More commonly one or both gonads is an ovotestis containing both types of tissue.
Although similar in some ways to mixed gonadal dysgenesis, the conditions can be distinguished histologically.
Presentation
External genitalia are often ambiguous, the degree depending mainly on the amount of testosterone produced by the testicular tissue between 8 and 16 weeks of gestation.
Causes
There are several ways in which this may occur.
- It can be caused by the division of one ovum, followed by fertilization of each haploid ovum and fusion of the two zygotes early in development.
- Alternately, an ovum can be fertilized by two sperm followed by trisomic rescue in one or more daughter cells.
- Two ova fertilized by two sperm cells will occasionally fuse to form a tetragametic chimera. If one male zygote and one female zygote fuse, a hermaphroditic individual may result.
- It can be associated with a mutation in the SRY gene.
Karyotypes
Encountered karyotypes include 46XX/46XY, or 46XX/47XXY or XX & XY with SRY mutations, mixed chromosomal anomalies or hormone deficiency/excess disorders, 47XXY, and various degrees of mosaicism of these and a variety of others.
The 3 primary karyotypes for true hermaphroditism are XX with genetic
anomalies (55-70% of cases), XX/XY (20-30% of cases) & XY (5-15% of
cases) with the remainder being a variety of other chromosomal anomalies
and mosaicisms.
Prevalence
Only 500 cases have been reported in medical literature.
Fertility
There are extremely rare cases of fertility in "truly hermaphroditic" humans. These individuals typically have functional ovarian tissue, but underdeveloped testes that are unable to engage in spermatogenesis. As a result, these individuals are fertile, but not auto-fertile.
There is evidence that 50% of individuals with ovotestes can go through ovulation but spermatogenesis is rare.
There is a hypothetical scenario, though, in which it could be
possible for a human to self fertilize. If a human chimera is formed
from a male and female zygote fusing into a single embryo, giving an
individual functional gonadal tissue of both types, such a
self-fertilization is feasible. Indeed, it is known to occur in non-human species where hermaphroditic animals are common, including some mammals. However, no such case of functional self-fertilization has ever been documented in humans.
As of 2010, there have been at least 11 reported cases of fertility in true hermaphrodite humans in the scientific literature, with one case of a person with XY-predominant (96%) mosaic giving birth. Estimated frequency of ovotestes is one in 83,000 births (0.0012%).
Etymology
The term derives from the Latin: hermaphroditus, from Ancient Greek: ἑρμαφρόδιτος, romanized: hermaphroditos, which derives from Hermaphroditos ( Ἑρμαϕρόδιτος), the son of Hermes and Aphrodite in Greek mythology. According to Ovid, he fused with the nymph Salmacis resulting in one individual possessing physical traits of both sexes; according to the earlier Diodorus Siculus, he was born with a physical body combining both sexes. The word hermaphrodite entered the English lexicon in the late fourteenth century.
Society and culture
Having ovotesticular disorder of sex development can make one inadmissible for service in the United States Armed Forces.
M.C. v. Aaronson
The U.S. legal case of M.C. v. Aaronson, advanced by intersex civil society organization interACT with the Southern Poverty Law Center was brought before the courts in 2013.
The child in the case was born in December 2004 with ovotestes,
initially determined as male, but subsequently assigned female and
placed in the care of South Carolina Department of Social Services in
February 2005.
Physicians responsible for M.C. initially concluded that surgery was
not urgent or necessary and M.C. had potential to identify as male or
female, but, in April 2006, M.C. was subjected to feminizing medical
interventions.
He was adopted in December 2006. Aged 8 at the time the case was taken,
he now identifies as male. The Southern Poverty Law Center state: "In
M.C.’s condition, there is no way to tell whether the child will
ultimately identify as a boy or a girl. Instead, the doctors decided to
assign M.C. female and change his body to fit their stereotype of how a
girl should look."
The defendant in the case, Dr Ian Aaronson, had written in 2001 that
"feminizing genitoplasty on an infant who might eventually identify
herself as a boy would be catastrophic".
The defendants sought to dismiss the case and seek a defense of
qualified immunity, but these were denied by the District Court for the
District of South Carolina. In January 2015, the Court of Appeals for
the Fourth Circuit reversed this decision and dismissed the complaint,
stating that, "it did not “mean to diminish the severe harm that M.C.
claims to have suffered” but that a reasonable official in 2006 did not
have fair warning from then-existing precedent that performing sex
assignment surgery on sixteen-month-old M.C. violated a clearly
established constitutional right." The Court did not rule on whether or not the surgery violated M.C.'s constitutional rights.
State suits were subsequently filed.
In July 2017, it was reported that the case had been settled out of
court by the Medical University of South Carolina for $440,000. The
University denied negligence, but agreed to a "compromise" settlement to
avoid "costs of litigation."
