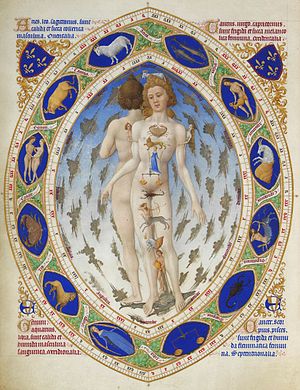
"Anatomical Man" (also "Zodiacal Man"), Très Riches Heures du Duc de Berry (Ms.65, f.14v, early 15th century)
Medieval medicine in Western Europe was composed of a mixture of existing ideas from antiquity, spiritual influences and what Claude Lévi-Strauss identifies as the "shamanistic complex" and "social consensus."
In the Early Middle Ages, following the fall of the Western Roman Empire, standard medical knowledge was based chiefly upon surviving Greek and Roman
texts, preserved in monasteries and elsewhere. Many simply placed their
hopes in the church and God to heal all their sicknesses. Ideas about
the origin and cure of disease were not purely secular, but were also based on a world view in which factors such as destiny, sin, and astral influences
played as great a part as any physical cause. The efficacy of cures was
similarly bound in the beliefs of patient and doctor rather than empirical evidence, so that remedia physicalia (physical remedies) were often subordinate to spiritual intervention.
Influences
Hippocratic medicine
The Western medical tradition often traces its roots directly to the early Greek civilization, much like the foundation of all of Western society. The Greeks certainly laid the foundation for Western medical practice but much more of Western medicine can be traced to the Middle East, Germanic, and Celtic cultures. The Greek medical foundation comes from a collection of writings known today as the Hippocratic Corpus. Remnants of the Hippocratic Corpus survive in modern medicine in forms like the “Hippocratic Oath” as in to “Do No Harm.”
The Hippocratic Corpus, popularly attributed to an ancient Greek medical practitioner known as Hippocrates,
lays out the basic approach to health care. Greek philosophers viewed
the human body as a system that reflects the workings of nature and
Hippocrates applied this belief to medicine. The body, as a reflection
of natural forces, contained four elemental properties expressed to the
Greeks as the four humors. The humors represented fire, air, earth and water through the properties of hot, cold, dry and moist, respectively. Health in the human body relied on keeping these humors in balance within each person.
Maintaining the balance of humors within a patient occurred in
several ways. An initial examination took place as standard for a
physician to properly evaluate the patient. The patient's home climate,
their normal diet, and astrological charts
were regarded during consultation. The heavens influenced each person
in different ways by influencing elements connected to certain humors,
important information in reaching a diagnosis. After the examination the
physician could determine which humor was unbalanced in the patient and
prescribe a new diet to restore that balance. Diet included not only food to eat or avoid but also an exercise regimen and medication.
Hippocratic medicine was written down within the Hippocratic
Corpus, therefore medical practitioners were required to be literate.
The written treatises within the Corpus are varied, incorporating
medical doctrine from any source the Greeks came into contact with. At Alexandria
in Egypt, the Greeks learned the art of surgery and dissection,; the
Egyptian skill in these arenas far surpassed those of Greeks and Romans due to social taboos regarding treatment of the dead. The early Hippocratic practitioner Herophilus engaged in dissection
and added new knowledge to human anatomy in the realms of the human
nervous system, the inner workings of the eye, differentiating arteries
from veins, and using pulses as a diagnostic tool in treatment.
Surgery and dissection yielded much knowledge of the human body that
Hippocratic physicians employed alongside their methods of balancing
humors in patients. The combination of knowledge in diet, surgery, and
medication formed the foundation of medical learning upon which Galen would later build upon with his own works.
Temple healing
The Greeks had been influenced by their Egyptian
neighbors, in terms of medical practice in surgery and medication.
However, the Greeks also absorbed many folk healing practices, including
incantations and dream healing. In Homer's Iliad and Odyssey
the gods are implicated as the cause of plagues or widespread disease
and that those maladies could be cured by praying to them. The religious
side of Greek medical practice is clearly manifested in the cult of Asclepius, whom Homer regarded as a great physician, and was deified in the third and fourth century BC.
Hundreds of temples devoted to Asclepius were founded throughout the
Greek and Roman empire to which untold numbers of people flocked for
cures. Healing visions and dreams formed the foundation for the curing
process as the person seeking treatment from Asclepius slept in a
special dormitory. The healing occurred either in the person's dream or
advice from the dream could be used to seek out the proper treatment for
their illness elsewhere. Afterwards the visitor to the temple bathed,
offered prayers and sacrifice, and received other forms of treatment
like medication, dietary restrictions, and an exercise regiment, keeping
with the Hippocratic tradition.
Pagan and folk medicine
Medicine in the Middle Ages had its roots in pagan
and folk practices. This influence was highlighted by the interplay
between Christian theologians who adopted aspects of pagan and folk
practices and chronicled them in their own works.
The practices adopted by Christian medical practitioners around the 2nd
century, and their attitudes toward pagan and folk traditions,
reflected an understanding of these practices, especially humoralism and
herbalism.
The practice of medicine in the early Middle Ages was empirical and pragmatic. It focused mainly on curing disease rather than discovering the cause of diseases.
Often it was believed the cause of disease was supernatural.
Nevertheless, secular approaches to curing diseases existed. People in
the Middle Ages understood medicine by adopting the ancient Greek
medical theory of humors. Since it was clear that the fertility of the
earth depended on the proper balance of the elements, it followed that
the same was true for the body, within which the various humors had to
be in balance. This approach greatly influenced medical theory throughout the Middle Ages.
Folk medicine of the Middle Ages dealt with the use of herbal remedies for ailments. The practice of keeping physic gardens teeming with various herbs with medicinal properties was influenced by the gardens of Roman antiquity.
Many early medieval manuscripts have been noted for containing
practical descriptions for the use of herbal remedies. These texts, such
as the Pseudo-Apuleius, included illustrations of various plants that would have been easily identifiable and familiar to Europeans at the time. Monasteries
later became centers of medical practice in the Middle Ages, and
carried on the tradition of maintaining medicinal gardens. These gardens
became specialized and capable of maintaining plants from Southern
Hemisphere as well as maintaining plants during winter.
Hildegard of Bingen
was an example of a medieval medical practitioner while educated in
classical Greek medicine, also utilized folk medicine remedies.
Her understanding of the plant based medicines informed her commentary
on the humors of the body and the remedies she described in her medical
text Causae et curae were influenced by her familiarity with folk
treatments of disease. In the rural society of Hildegard's time, much
of the medical care was provided by women, along with their other
domestic duties. Kitchens were stocked with herbs and other substances required in folk remedies for many ailments. Causae et curae
illustrated a view of symbiosis of the body and nature, that the
understanding of nature could inform medical treatment of the body.
However, Hildegard maintained the belief that the root of disease was a
compromised relationship between a person and God. Many parallels between pagan and Christian ideas about disease existed during the early Middle Ages.[citation needed]
Christian views of disease differed from those held by pagans because
of a fundamental difference in belief: Christians' belief in a personal
relationship with God greatly influenced their views on medicine.
Evidence of pagan influence on emerging Christian medical
practice was provided by many prominent early Christian thinkers, such
as Origen, Clement of Alexandria, and Augustine, who studied natural philosophy
and held important aspects of secular Greek philosophy that were in
line with Christian thought. They believed faith supported by sound
philosophy was superior to simple faith.
The classical idea of the physician as a selfless servant who had to
endure unpleasant tasks and provide necessary, often painful treatment
was of great influence on early Christian practitioners. The metaphor
was not lost on Christians who viewed Christ as the ultimate physician.
Pagan philosophy had previously held that the pursuit of virtue should
not be secondary to bodily concerns. Similarly, Christians felt that,
while caring for the body was important, it was second to spiritual
pursuits.
The relationship between faith and the bodies ailments explains why
most medieval medical practice was performed by Christian monks.
Monasteries
Dominican doctor taking a pulse. Rare Book & Manuscript Library University of Pennsylvania LJS 24
Monasteries
developed not only as spiritual centers, but also centers of
intellectual learning and medical practice. Locations of the monasteries
were secluded and designed to be self-sufficient, which required the
monastic inhabitants to produce their own food and also care for their
sick. Prior to the development of hospitals, people from the surrounding
towns looked to the monasteries for help with their sick.
A combination of both spiritual and natural healing was used to treat the sick. Herbal remedies, known as Herbals,
along with prayer and other religious rituals were used in treatment by
the monks and nuns of the monasteries. Herbs were seen by the monks and
nuns as one of God’s creations for the natural aid that contributed to
the spiritual healing of the sick individual. An herbal textual
tradition also developed in the medieval monasteries.
Older herbal Latin texts were translated and also expanded in the
monasteries. The monks and nuns reorganized older texts so that they
could be utilized more efficiently, adding a table of contents
for example to help find information quickly. Not only did they
reorganize existing texts, but they also added or eliminated
information. New herbs that were discovered to be useful or specific
herbs that were known in a particular geographic area were added. Herbs
that proved to be ineffective were eliminated. Drawings were also added
or modified in order for the reader to effectively identify the herb.
The Herbals that were being translated and modified in the monasteries
were some of the first medical texts produced and used in medical
practice in the Middle Ages.
Not only were herbal texts being produced, but also other
medieval texts that discussed the importance of the humors. Monasteries
in Medieval Europe gained access to Greek medical works by the middle of
the 6th century.
Monks translated these works into Latin, after which they were
gradually disseminated across Europe. Monks such as Arnald of Villanova
also translated the works of Galen and other classical Greek scholars
from Arabic to Latin during the Medieval ages.
By producing these texts and translating them into Latin, Christian
monks both preserved classical Greek medical information and allowed for
its use by European medical practitioners. By the early 1300s these
translated works would become available at medieval universities and
form the foundation of the universities medical teaching programs.
Hildegard of Bingen,
a well known abbess, wrote about Hippocratic Medicine using humoral
theory and how balance and imbalance of the elements affected the health
of an individual, along with other known sicknesses of the time, and
ways in which to combine both prayer and herbs to help the individual
become well. She discusses different symptoms that were common to see
and the known remedies for them.
In exchanging the herbal texts among monasteries, monks became
aware of herbs that could be very useful but were not found in the
surrounding area. The monastic clergy traded with one another or used
commercial means to obtain the foreign herbs.
Inside most of the monastery grounds there had been a separate garden
designated for the plants that were needed for the treatment of the
sick. A serving plan of St. Gall depicts a separate garden to be developed for strictly medical herbals.
Monks and nuns also devoted a large amount of their time in the
cultivation of the herbs they felt were necessary in the care of the
sick. Some plants were not native to the local area and needed special
care to be kept alive. The monks used a form of science, what we would today consider botany,
to cultivate these plants. Foreign herbs and plants determined to be
highly valuable were grown in gardens within close proximity to the
monastery in order for the monastic clergy to hastily have access to the
natural remedies.
Medicine in the monasteries was concentrated on assisting the
individual to return to normal health. Being able to identify symptoms
and remedies was the primary focus. In some instances identifying the
symptoms led the monastic clergy to have to take into consideration the
cause of the illness in order to implement a solution. Research and experimental
processes were continuously being implemented in monasteries to be able
to successfully fulfill their duties to God to take care of all God's
people.
Christian charity
Christian practice and attitudes toward medicine drew on Middle Eastern (particularly from local Jews)
and Greek influences. The Jews took their duty to care for their fellow
Jews seriously. This duty extended to lodging and medical treatment of pilgrims to the temple at Jerusalem.
Temporary medical assistance had been provided in classical Greece for
visitors to festivals and the tradition extended through the Roman
Empire, especially after Christianity became the state religion
prior to the empire's decline. In the early Medieval period, hospitals,
poor houses, hostels, and orphanages began to spread from the Middle
East, each with the intention of helping those most in need.
Charity, the driving principle behind these healing centers,
encouraged the early Christians to care for others. The cities of
Jerusalem, Constantinople, and Antioch contained some of the earliest and most complex hospitals, with many beds to house patients and staff physicians with emerging specialties. Some hospitals were large enough to provide education in medicine, surgery and patient care. St. Basil
(AD 330-79) argued that God put medicines on the Earth for human use,
while many early church fathers agreed that Hippocratic medicine could
be used to treat the sick and satisfy the charitable need to help
others.
Medicine
Medieval European medicine became more developed during the Renaissance of the 12th century, when many medical texts both on Ancient Greek medicine and on Islamic medicine were translated from Arabic during the 13th century. The most influential among these texts was Avicenna's The Canon of Medicine, a medical encyclopedia written in circa 1030 which summarized the medicine of Greek, Indian and Muslim physicians until that time. The Canon became an authoritative text in European medical education until the early modern period. Other influential texts from Jewish authors include the Liber pantegni by Isaac Israeli ben Solomon, while Arabic authors contributed De Gradibus by Alkindus and Al-Tasrif' by Abulcasis.
At Schola Medica Salernitana in Southern Italy, medical texts from Byzantium and the Arab world were readily available, translated from the Greek and Arabic at the nearby monastic centre of Monte Cassino. The Salernitan masters gradually established a canon of writings, known as the ars medicinae (art of medicine) or articella (little art), which became the basis of European medical education for several centuries.
During the Crusades the influence of Islamic medicine became stronger. The influence was mutual and Islamic scholars such as Usamah ibn Munqidh
also described their positive experience with European medicine - he
describes a European doctor successfully treating infected wounds with
vinegar and recommends a treatment for scrofula demonstrated to him by an unnamed "Frank".
Classical medicine
Anglo-Saxon translations of classical works like Dioscorides Herbal
survive from the 10th century, showing the persistence of elements of
classical medical knowledge. Other influential translated medical texts
at the time included the Hippocratic Corpus attributed to Hippocrates, and the writings of Galen.
Galen of Pergamon, a Greek, was one of the most influential ancient physicians. Galen described the four classic symptoms of inflammation (redness, pain, heat, and swelling) and added much to the knowledge of infectious disease and pharmacology.
His anatomic knowledge of humans was defective because it was based on
dissection of animals, mainly apes, sheep, goats and pigs. Some of Galen's teachings held back medical progress. His theory, for example, that the blood carried the pneuma,
or life spirit, which gave it its red colour, coupled with the
erroneous notion that the blood passed through a porous wall between the
ventricles
of the heart, delayed the understanding of circulation and did much to
discourage research in physiology. His most important work, however, was
in the field of the form and function of muscles and the function of
the areas of the spinal cord. He also excelled in diagnosis and prognosis.
Medieval surgery
Medieval surgery arose from a foundation created from Ancient Egyptian, Greek and Arabic medicine . An example of such influence would be Galen, the most influential practitioner of surgical or anatomical practices that he performed while attending to gladiators at Pergamon.
The accomplishments and the advancements in medicine made by the Arabic
world were translated and made available to the Latin world. This new
wealth of knowledge allowed for a greater interest in surgery.
In Paris,
in the late thirteenth century, it was deemed that surgical practices
were extremely disorganized, and so the Parisian provost decided to
enlist six of the most trustworthy and experienced surgeons and have
them assess the performance of other surgeons. The emergence of universities allowed for surgery to be a discipline that should be learned and be communicated to others as a uniform practice. The University of Padua
was one of the "leading Italian universities in teaching medicine,
identification and treating of diseases and ailments, specializing in
autopsies and workings of the body." The most prestigious and famous
part of the university is the oldest surviving anatomical theater, in which students studied anatomy by observing their teachers perform public dissections.
Surgery was formally taught in Italy even though it was initially
looked down upon as a lower form of medicine. The most important figure
of the formal learning of surgery was Guy de Chauliac.
He insisted that a proper surgeon should have a specific knowledge of
the human body such as anatomy, food and diet of the patient, and other
ailments that may have affected the patients. Not only should surgeons
have knowledge about the body but they should also be well versed in the
liberal arts. In this way, surgery was no longer regarded as a lower practice, but instead began to be respected and gain esteem and status.
During the Crusades,
one of the duties of surgeons was to travel around a battlefield,
assessing soldiers' wounds and declaring whether or not the soldier was
deceased. Because of this task, surgeons were deft at removing
arrowheads from their patients' bodies. Another class of surgeons that existed were barber surgeons.
They were expected not only to be able to perform formal surgery, but
also to be deft at cutting hair and trimming beards. Some of the
surgical procedures they would conduct were bloodletting and treating sword and arrow wounds.
In the mid-fourteenth century, there were restrictions placed on London
surgeons as to what types of injuries they were able to treat and the
types of medications that they could prescribe or use, because surgery
was still looked at as an incredibly dangerous procedure that should
only be used appropriately. Some of the wounds that were allowed to be
performed on were external injuries, such as skin lacerations caused by a
sharp edge, such as by a sword, dagger and axe or through household
tools such as knives. During this time, it was also expected that the
surgeons were extremely knowledgeable on human anatomy and would be held
accountable for any consequences as a result of the procedure.
Advances
A dentist with silver forceps and a necklace of large teeth, extracting the tooth of a well seated man. Omne Bonum (England - London; 1360–1375).
The Middle Ages contributed a great deal to medical knowledge. This
period contained progress in surgery, medical chemistry, dissection, and
practical medicine. The Middle Ages laid the ground work for later,
more significant discoveries. There was a slow but constant progression
in the way that medicine was studied and practiced. It went from apprenticeships to universities and from oral traditions
to documenting texts. The most well-known preservers of texts, not only
medical, would be the monasteries. The monks were able to copy and
revise any medical texts that they were able to obtain. Besides
documentation the Middle Ages also had one of the first well known
female physicians, Hildegard of Bingen.
Hildegard was born in 1098 and at the age of fourteen she entered the double monastery of Dissibodenberg.
She wrote the medical text Causae et curae, in which many medical
practices of the time were demonstrated. This book contained diagnosis,
treatment, and prognosis of many different diseases and illnesses. This
text sheds light on medieval medical practices of the time. It also
demonstrates the vast amount of knowledge and influences that she built
upon. In this time period medicine was taken very seriously, as is shown
with Hildegard's detailed descriptions on how to perform medical tasks.
The descriptions are nothing without their practical counterpart, and
Hildegard was thought to have been an infirmarian in the monastery where
she lived. An infirmarian treated not only other monks but pilgrims,
workers, and the poor men, women, and children in the monastery's
hospice. Because monasteries were located in rural areas the infirmarian
was also responsible for the care of lacerations, fractures,
dislocations, and burns.
Along with typical medical practice the text also hints that the youth
(such as Hildegard) would have received hands-on training from the
previous infirmarian. Beyond routine nursing this also shows that
medical remedies from plants, either grown or gathered, had a
significant impact of the future of medicine. This was the beginnings of
the domestic pharmacy.
Although plants were the main source of medieval remedies, around the sixteenth century medical chemistry became more prominent. "Medical chemistry began with the adaptation of chemical processes to the preparation of medicine".
Previously medical chemistry was characterized by any use of inorganic
materials, but it was later refined to be more technical, like the
processes of distillation. John of Rupescissa's works in alchemy and the beginnings of medical chemistry is recognized for the bounds in chemistry. His works in making the philosopher's stone, also known as the fifth essence, were what made he became known for.
Distillation techniques were mostly used, and it was said that by
reaching a substance's purest form the person would find the fifth
essence, and this is where medicine comes in. Remedies were able to be
made more potent because there was now a way to remove nonessential
elements. This opened many doors for medieval physicians as new,
different remedies were made. Medical chemistry provided an "increasing
body of pharmacological literature dealing with the use of medicines
derived from mineral sources".
Medical chemistry also shows the use of alcohols in medicine. Though
these events were not huge bounds for the field, they were influential
in determining the course of science. It was the start of
differentiation between alchemy and chemistry.
The Middle Ages brought a new way of thinking and a lessening on
the taboo of dissection. Dissection for medical purposes became more
prominent around 1299. During this time the Italians were practicing anatomical dissection and the first record of an autopsy
dates from 1286. Dissection was first introduced in the educational
setting at the university of Bologna, to study and teach anatomy. The
fourteenth century saw a significant spread of dissection and autopsy in
Italy, and was not only taken up by medical faculties, but by colleges
for physicians and surgeons.
Roger Frugardi of Parma composed his treatise on Surgery around about 1180. Between 1350 and 1365 Theodoric Borgognoni produced a systematic four volume treatise on surgery, the Cyrurgia, which promoted important innovations as well as early forms of antiseptic practice in the treatment of injury, and surgical anaesthesia using a mixture of opiates and herbs.
Compendiums like Bald's Leechbook (circa 900), include citations from a variety of classical works alongside local folk remedies.
Theories of medicine
Although
each of these theories has distinct roots in different cultural and
religious traditions, they were all intertwined in the general
understanding and practice of medicine. For example, the Benedictine
abbess and healer, Hildegard of Bingen, claimed that black bile and other humor imbalances were directly caused by presence of the Devil and by sin. Another example of the fusion of different medicinal theories is the combination of Christian and pre-Christian ideas about elf-shot
(elf- or fairy-caused diseases) and their appropriate treatments. The
idea that elves caused disease was a pre-Christian belief that developed
into the Christian idea of disease-causing demons or devils.
Treatments for this and other types of illness reflected the
coexistence of Christian and pre-Christian or pagan ideas of medicine.
Humors
13th-century illustration showing the veins.
The underlying principle of medieval medicine was the theory of humors.
This was derived from the ancient medical works, and dominated all
western medicine until the 19th century. The theory stated that within
every individual there were four humors, or principal fluids -
black bile, yellow bile, phlegm, and blood, these were produced by
various organs in the body, and they had to be in balance for a person
to remain healthy. Too much phlegm in the body, for example, caused
lung problems; and the body tried to cough up the phlegm to restore a
balance. The balance of humours in humans could be achieved by diet,
medicines, and by blood-letting,
using leeches. The four humours were also associated with the four
seasons, black bile-autumn, yellow bile-summer, phlegm-winter and
blood-spring.
| HUMOR | TEMPER | ORGAN | NATURE | ELEMENT |
|---|---|---|---|---|
| Black bile | Melancholic | Spleen | Cold Dry | Earth |
| Phlegm | Phlegmatic | Lungs | Cold Wet | Water |
| Blood | Sanguine | Head | Warm Wet | Air |
| Yellow bile | Choleric | Gall Bladder | Warm Dry | Fire |
The astrological signs of the zodiac
were also thought to be associated with certain humours. Even now, some
still use words "choleric", "sanguine", "phlegmatic" and "melancholic"
to describe personalities.
Herbalism and botany
Herbs were commonly used in salves and drinks to treat a range of
maladies. The particular herbs used depended largely on the local
culture and often had roots in pre-Christian religion.
The success of herbal remedies was often ascribed to their action upon
the humours within the body. The use of herbs also drew upon the
medieval Christian doctrine of signatures
which stated that God had provided some form of alleviation for every
ill, and that these things, be they animal, vegetable or mineral,
carried a mark or a signature upon them that gave an indication of their usefulness. For example, skullcap seeds (used as a headache remedy) can appear to look like miniature skulls; and the white spotted leaves of lungwort
(used for tuberculosis) bear a similarity to the lungs of a diseased
patient. A large number of such resemblances were believed to exist.
Many monasteries developed herb gardens for use in the production of herbal cures,
and these remained a part of folk medicine, as well as being used by
some professional physicians. Books of herbal remedies were produced,
one of the most famous being the Welsh, Red Book of Hergest, dating from around 1400.
During the early Middle Ages, botany
had undergone drastic changes from that of its antiquity predecessor
(Greek practice). An early medieval treatise in the West on plants known
as the Ex herbis femininis was largely based on Dioscorides Greek text: De material medica.
The Ex herbis was a lot more popular during this time because it was
not only easier to read, but contained plants and their remedies that
related to the regions of southern Europe, where botany was being
studied. It also provided better medical direction on how to create
remedies, and how to properly use them. This book was also highly
illustrated, where its former was not, making the practice of botany
easier to comprehend.
Dioscoridis: De materia medica
The re-emergence of Botany in the medieval world came about during
the sixteenth century. As part of the revival of classical medicine, one
of the biggest areas of interest was materia medica: the study of
remedial substances. “Italian humanists in the fifteenth century had
recovered and translated ancient Greek botanical texts which had been
unknown in the West in the Middle Ages or relatively ignored”.
Soon after the rise in interest in botany, universities such as Padua
and Bologna started to create programs and fields of study; some of
these practices including setting up gardens so that students were able
to collect and examine plants. “Botany was also a field in which
printing made a tremendous impact, through the development of
naturalistic illustrated herbals”.
During this time period, university practices were highly concerned
with the philosophical matters of study in sciences and the liberal
arts, “but by the sixteenth century both scholastic discussion of plants
and reliance upon intermediary compendia for plant names and
descriptions were increasingly abandoned in favor of direct study of the
original texts of classical authors and efforts to reconcile names,
descriptions, and plants in nature”.
Botanist expanded their knowledge of different plant remedies, seeds,
bulbs, uses of dried and living plants through continuous interchange
made possible by printing. In sixteenth century medicine, botany was
rapidly becoming a lively and fast-moving discipline that held wide
universal appeal in the world of doctors, philosophers, and pharmacists.
Mental disorders
Those with mental disorders
in medieval Europe were treated using a variety of different methods,
depending on the beliefs of the physician they would go to. Some doctors
at the time believed that supernatural forces such as witches, demons
or possession caused mental disorders. These physicians believed that
prayers and incantations, along with exorcisms, would cure the afflicted
and relieve them of their suffering. Another form of treatment existed to help expel evil spirits from the body of a patient, known as trephining. Trephining was a means of treating epilepsy
by opening a hole in the skull through drilling or cutting. It was
believed that any evil spirit or evil air would flow out of the body
through the hole and leave the patient in peace.
Contrary to the common belief that most physicians in Medieval Europe
believed that mental illness was caused by supernatural factors, it is
believed that these were only the minority of cases related to the
diagnosis and treatment of those suffering from mental disorders. Most
physicians believed that these disorders were caused by physical
factors, such as the malfunction of organs or an imbalance of the
humors. One of the most well-known and reported examples was the belief
that an excess amount of black bile was the cause of melancholia, which
would now be classified as schizophrenia or depression.
Medieval physicians used various forms of treatment to try to fix any
physical problems that were causing mental disorders in their patients.
When the cause of the disorder being examined was believed to be caused
by an imbalance of the four humors, doctors attempted to rebalance the
body. They did so through a combination of emetics, laxatives and different methods of bloodletting, in order to remove excess amounts of bodily fluids.
Christian interpretation
Medicine in the Middle Ages was rooted in Christianity
through not only the spread of medical texts through monastic tradition
but also through the beliefs of sickness in conjunction with medical
treatment and theory. Christianity, throughout the medieval period, did
not set medical knowledge back or forwards.
The church taught that God sometimes sent illness as a punishment, and
that in these cases, repentance could lead to a recovery. This led to
the practice of penance and pilgrimage as a means of curing illness. In
the Middle Ages,
some people did not consider medicine a profession suitable for
Christians, as disease was often considered God-sent. God was considered
to be the "divine physician" who sent illness or healing depending on
his will. From a Christian perspective, disease could be seen either as a
punishment from God or as an affliction of demons (or elves, see first
paragraph under Theories of Medicine). The ultimate healer in this
interpretation is of course God, but medical practitioners cited both
the bible and Christian history as evidence that humans could and should
attempt to cure diseases. For example, the Lorsch Book of Remedies or the Lorsch Leechbook
contains a lengthy defense of medical practice from a Christian
perspective. Christian treatments focused on the power of prayer and
holy words, as well as liturgical practice.
However, many monastic orders, particularly the Benedictines, were very involved in healing and caring for the sick and dying. In many cases, the Greek philosophy that early Medieval medicine was based upon was compatible with Christianity.
Though the widespread Christian tradition of sickness being a divine
intervention in reaction to sin was popularly believed throughout the
Middle Ages, it did not rule out natural causes. For example, the Black Death was thought to have been caused by both divine and natural origins.
The plague was thought to have been a punishment from God for sinning,
however because it was believed that God was the reason for all natural
phenomena, the physical cause of the plague could be scientifically
explained as well. One of the more widely accepted scientific
explanations of the plague was the corruption of air in which pollutants such as rotting matter or anything that gave the air an unpleasant scent caused the spread of the plague.
Hildegard of Bingen
(1098–1179) played an important role in how illness was interpreted
through both God and natural causes through her medical texts as well.
As a nun, she believed in the power of God and prayer to heal, however
she also recognized that there were natural forms of healing through the
humors as well. Though there were cures for illness outside of prayer,
ultimately the patient was in the hands of God. One specific example of this comes from her text Causae et Curae in which she explains the practice of bleeding:
Bleeding, says Hildegard, should be done when the moon is waning, because then the "blood is low" (77:23-25). Men should be bled from the age of twelve (120:32) to eighty (121:9), but women, because they have more of the detrimental humors, up to the age of one hundred (121:24). For therapeutic bleeding, use the veins nearest the diseased part (122:19); for preventive bleeding, use the large veins in the arms (121:35-122:11), because they are like great rivers whose tributaries irrigate the body (123:6-9, 17-20). 24 From a strong man, take "the amount that a thirsty person can swallow in one gulp" (119:20); from a weak one, "the amount that an egg of moderate size can hold" (119:22-23). Afterward, let the patient rest for three days and give him undiluted wine (125:30), because "wine is the blood of the earth" (141:26). This blood can be used for prognosis; for instance, "if the blood comes out turbid like a man's breath, and if there are black spots in it, and if there is a waxy layer around it, then the patient will die, unless God restore him to life" (124:20-24).
Monasteries were also important in the development of hospitals
throughout the Middle Ages, where the care of sick members of the
community was an important obligation. These monastic hospitals were not
only for the monks who lived at the monasteries but also the pilgrims,
visitors and surrounding population.
The monastic tradition of herbals and botany influenced Medieval
medicine as well, not only in their actual medicinal uses but in their
textual traditions. Texts on herbal medicine were often copied in
monasteries by monks, but there is substantial evidence that these monks
were also practicing the texts that they were copying. These texts were
progressively modified from one copy to the next, with notes and
drawings added into the margins as the monks learned new things and
experimented with the remedies and plants that the books supplied.
Monastic translations of texts continued to influence medicine as many
Greek medical works were translated into Arabic. Once these Arabic texts
were available, monasteries in western Europe were able to translate
them, which in turn would help shape and redirect Western medicine in
the later Middle Ages.
The ability for these texts to spread from one monastery or school in
adjoining regions created a rapid diffusion of medical texts throughout
western Europe.
The influence of Christianity continued into the later periods of
the Middle Ages as medical training and practice moved out of the
monasteries and into cathedral schools,
though more for the purpose of general knowledge rather than training
professional physicians. The study of medicine was eventually
institutionalized into the medieval universities.
Even within the university setting, religion dictated a lot of the
medical practice being taught. For instance, the debate of when the
spirit left the body influenced the practice of dissection within the
university setting. The universities in the south believed that the soul
only animated the body and left immediately upon death. Because of
this, the body while still important, went from being a subject to an
object. However, in the north they believed that it took longer for the
soul to leave as it was an integral part of the body.
Though medical practice had become a professional and institutionalized
field, the argument of the soul in the case of dissection shows that
the foundation of religion was still an important part of medical
thought in the late Middle Ages.
Medical universities in medieval Europe
Medicine
was not a formal area of study in early medieval medicine, but it grew
in response to the proliferation of translated Greek and Arabic medical
texts in the 11th century.
Western Europe also experienced economic, population and urban growth
in the 12th and 13th centuries leading to the ascent of medieval medical
universities. The University of Salerno
was considered to be a renowned provenance of medical practitioners in
the 9th and 10th centuries, but was not recognized as an official
medical university until 1231. The founding of the Universities of Paris (1150), Bologna (1158), Oxford, (1167), Montpelier (1181) and Padua
(1222), extended the initial work of Salerno across Europe, and by the
13th century, medical leadership had passed to these newer institutions.
Despite Salerno’s important contributions to the foundation of the
medical curriculum, scholars do not consider Salerno to be one of the
medieval medical universities. This is because the formal establishment
of a medical curriculum occurred after the decline of Salerno’s grandeur
of being a center for academic medicine.
The medieval medical universities' central concept concentrated
on the balance between the humors and “in the substances used for
therapeutic purposes”.
The curriculum’s secondary concept focused on medical astrology, where
celestial events were thought to influence health and disease. The medical curriculum was designed to train practitioners.
Teachers of medical students were often successful physicians,
practicing in conjunction with teaching. The curriculum of academic
medicine was fundamentally based on translated texts and treatises
attributed to Hippocrates and Galen as well as Arabic medical texts. At Montpellier's Faculty of Medicine professors were required in 1309 to possess Galen's books which described humors, De complexionibus, De virtutibus naturalibus, De criticis diebu so that they could teach students about Galen's medical theory.
The translated works of Hippocrates and Galen were often incomplete,
and were mediated with Arabic medical texts for their “independent
contributions to treatment and to herbal pharmacology”. Although anatomy was taught in academic medicine through the dissection of cadavers, surgery was largely independent from medical universities.
The University of Bologna was the only university to grant degrees in
surgery. Academic medicine also focused on actual medical practice where
students would study individual cases and observe the professor
visiting patients.
The required number of years to become a licensed physician
varied among universities. Montpellier required students without their
masters of arts to complete three and a half years of formal study and
six months of outside medical practice.
In 1309, the curriculum of Montpellier was changed to six years of
study and eight months of outside medical practice for those without a
masters of arts, whereas those with a masters of arts were only
subjected to five years of study with eight months of outside medical
practice.
The university of Bologna required three years of philosophy, three
years of astrology, and four years of attending medical lectures.
Medical practitioners
Members of religious orders
were major sources of medical knowledge and cures. There appears to
have been some controversy regarding the appropriateness of medical
practice for members of religious orders. The Decree of the Second Lateran Council of 1139 advised the religious to avoid medicine because it was a well-paying job with higher social status
than was appropriate for the clergy. However, this official policy was
not often enforced in practice and many religious continued to practice
medicine.
There were many other medical practitioners besides clergy.
Academically trained doctors were particularly important in cities with
universities. Medical faculty at universities figured prominently in
defining medical guilds and accepted practices as well as the required qualifications for physicians. Beneath these university-educated physicians there existed a whole hierarchy of practitioners. Wallis
suggests a social hierarchy with these university educated physicians
on top, followed by “learned surgeons; craft-trained surgeons; barber
surgeons, who combined bloodletting with the removal of “superfluities”
from the skin and head; itinerant specialists such as dentists and
oculists; empirics; midwives; clergy who dispensed charitable advice and
help; and, finally, ordinary family and neighbors”. Each of these groups practiced medicine in their own capacity and contributed to the overall culture of medicine.
Hospital system
In the Medieval period the term hospital encompassed hostels for travellers, dispensaries for poor relief,
clinics and surgeries for the injured, and homes for the blind, lame,
elderly, and mentally ill. Monastic hospitals developed many treatments,
both therapeutic and spiritual.
During the thirteenth century an immense number of hospitals were built. The Italian cities were the leaders of the movement. Milan had no fewer than a dozen hospitals and Florence before the end of the fourteenth century had some thirty hospitals. Some of these were very beautiful buildings. At Milan a portion of the general hospital was designed by Bramante and another part of it by Michelangelo. The Hospital of Sienna, built in honor of St. Catherine, has been famous ever since. Everywhere throughout Europe this hospital movement spread. Virchow, the great German pathologist, in an article on hospitals, showed that every city of Germany of five thousand inhabitants had its hospital. He traced all of this hospital movement to Pope Innocent III, and though he was least papistically inclined, Virchow did not hesitate to give extremely high praise to this pontiff for all that he had accomplished for the benefit of children and suffering mankind.
Hospitals began to appear in great numbers in France and England. Following the French Norman invasion into England,
the explosion of French ideals led most Medieval monasteries to develop
a hospitium or hospice for pilgrims. This hospitium eventually
developed into what we now understand as a hospital, with various monks
and lay helpers providing the medical care for sick pilgrims and victims
of the numerous plagues and chronic diseases that afflicted Medieval
Western Europe. Benjamin Gordon
supports the theory that the hospital – as we know it - is a French
invention, but that it was originally developed for isolating lepers and plague victims, and only later undergoing modification to serve the pilgrim.
Owing to a well-preserved 12th-century account of the monk Eadmer of the Canterbury cathedral, there is an excellent account of Bishop Lanfranc's aim to establish and maintain examples of these early hospitals:
But I must not conclude my work by omitting what he did for the poor outside the walls of the city Canterbury. In brief, he constructed a decent and ample house of stone…for different needs and conveniences. He divided the main building into two, appointing one part for men oppressed by various kinds of infirmities and the other for women in a bad state of health. He also made arrangements for their clothing and daily food, appointing ministers and guardians to take all measures so that nothing should be lacking for them.
Later developments
Anathomia, 1541
Corpus physicum, from Liber de arte Distillandi de Compositis, 1512
High medieval surgeons like Mondino de Liuzzi
pioneered anatomy in European universities and conducted systematic
human dissections. Unlike pagan Rome, high medieval Europe did not have a
complete ban on human dissection. However, Galenic influence was still
so prevalent that Mondino and his contemporaries attempted to fit their
human findings into Galenic anatomy.
During the period of the Renaissance from the mid 1450s onward, there were many advances in medical practice. The Italian Girolamo Fracastoro(1478–1553) was the first to propose that epidemic diseases might be caused by objects outside the body that could be transmitted by direct or indirect contact. He also proposed new treatments for diseases such as syphilis.
In 1543 the Flemish Scholar Andreas Vesalius wrote the first complete textbook on human anatomy: "De Humani Corporis Fabrica", meaning "On the Fabric of the Human Body". Much later, in 1628, William Harvey explained the circulation of blood
through the body in veins and arteries. It was previously thought that
blood was the product of food and was absorbed by muscle tissue.
During the 16th century, Paracelsus, like Girolamo, discovered that illness was caused by agents outside the body such as bacteria, not by imbalances within the body.
The French army doctor Ambroise Paré,
born in 1510, revived the ancient Greek method of tying off blood
vessels. After amputation the common procedure was to cauterize the open
end of the amputated appendage to stop the hemorrhaging. This was done
by heating oil,
water, or metal and touching it to the wound to seal off the blood
vessels. Pare also believed in dressing wounds with clean bandages and
ointments, including one he made himself composed of eggs, oil of roses, and turpentine. He was the first to design artificial hands and limbs
for amputation patients. On one of the artificial hands, the two pairs
of fingers could be moved for simple grabbing and releasing tasks and
the hand look perfectly natural underneath a glove.
Medical catastrophes were more common in the late Middle Ages and the Renaissance than they are today. During the Renaissance, trade routes were the perfect means of transportation for disease. Eight hundred years after the Plague of Justinian, the bubonic plague returned to Europe. Starting in Asia, the Black Death reached Mediterranean and western Europe in 1348 (possibly from Italian merchants fleeing fighting in Crimea),
and killed 25 million Europeans in six years, approximately 1/3 of the
total population and up to a 2/3 in the worst-affected urban areas.
Before Mongols left besieged Crimean Kaffa
the dead or dying bodies of the infected soldiers were loaded onto
catapults and launched over Kaffa's walls to infect those inside. This
incident was among the earliest known examples of biological warfare and is credited as being the source of the spread of the Black Death into Europe.
The plague repeatedly returned to haunt Europe and the
Mediterranean from 14th through 17th centuries. Notable later outbreaks
include the Italian Plague of 1629–1631, the Great Plague of Seville (1647–1652), the Great Plague of London (1665–1666), the Great Plague of Vienna (1679), the Great Plague of Marseille in 1720–1722 and the 1771 plague in Moscow.
Before the Spanish discovered the New World (continental America), the deadly infections of smallpox, measles, and influenza were unheard of. The Native Americans did not have the immunities the Europeans developed through long contact with the diseases. Christopher Columbus ended the Americas' isolation in 1492 while sailing under the flag of Castile, Spain. Deadly epidemics swept across the Caribbean. Smallpox wiped out villages in a matter of months. The island of Hispaniola
had a population of 250,000 Native Americans. 20 years later, the
population had dramatically dropped to 6,000. 50 years later, it was
estimated that approximately 500 Native Americans were left. Smallpox
then spread to the area which is now Mexico where it then helped destroy
the Aztec Empire.
In the 1st century of Spanish rule in what is now Mexico, 1500–1600,
Central and South Americans died by the millions. By 1650, the majority
of New Spain (now Mexico) population had perished.
Contrary to popular belief bathing and sanitation were not lost in Europe with the collapse of the Roman Empire. Bathing in fact did not fall out of fashion in Europe until shortly after the Renaissance, replaced by the heavy use of sweat-bathing and perfume,
as it was thought in Europe that water could carry disease into the
body through the skin. Medieval church authorities believed that public bathing created an environment open to immorality and disease. Roman Catholic Church officials even banned public bathing in an unsuccessful effort to halt syphilis epidemics from sweeping Europe.
Battlefield medicine
Camp and movement
In
order for an army to be in good fighting condition, it must maintain
the health of its soldiers. One way of doing this is knowing the proper
location to set up camp. Military camps were not to be set up in any sort of marshy region. Marsh lands tend to have standing water, which can draw in mosquitos. Mosquitos in turn can carry deadly disease, such as malaria.
As the camp and troops were needed to be moved, the troops would be
wearing heavy soled shoes in order to prevent wear on soldiers’ feet.
Waterborne illness has also remained an issue throughout the
centuries. When soldiers would look for water they would be searching
for some sort of natural spring, or other form of flowing water. When
water sources were found, any type of rotting wood, or plant material,
would be removed before the water was used for drinking. If these
features could not be removed, then water would be drawn from a
different part of the source. By doing this the soldiers were more likely to be drinking from a safe source of water. Thus, water borne bacteria
had a less chance of making soldiers ill. One process used to check
for dirty water, was to moisten a fine white linen cloth with the water
and leave it out to dry. If the cloth had any type of stain, it would
be considered to be diseased. If the cloth was clean, the water was
healthy and drinkable. Fresh water also assists with sewage
disposal, as well as wound care. Thus, a source of fresh water was a
preemptive measure taken to defeat disease and keep men healthy once
they were wounded.
Physicians
Surgeons
In Medieval Europe the surgeons social status improved greatly as their expertise was needed on the battlefield.
Owing to the number of patients, warfare created a unique learning
environment for these surgeons. The dead bodies also provided an
opportunity for learning. The corpses provided a means to learn through
hands on experience. As war declined, the need for surgeons declined
as well. This would follow a pattern, where the status of the surgeon
would flux in regards to whether or not there was actively a war going
on.
First medical schools
Medical
school also first appeared in the Medieval period. This created a
divide between physicians trained in the classroom and physicians who
learned their trade through practice. The divide created a shift
leading to physicians trained in the classroom to be of higher esteem
and more knowledgeable. Despite this, there was still a lack of
knowledge by physicians in the military.
The knowledge of the militaries’ physicians was greatly acquired
through first hand experience. In the Medical schools, physicians such
as Galen
were referenced as the ultimate source of knowledge. Thus, the
education in the schools was aimed at proving these ancient physicians
were correct. This created issues as Medieval knowledge surpassed the
knowledge of these ancient physicians. In the scholastic
setting it still became practice to reference ancient physicians or the
other information being presented was not taken seriously.
Level of care
The
soldiers that received medical attention was most likely from a
physician who was not well trained. To add to this, a soldier did not
have a good chance of surviving a wound that needed specific,
specialized, or knowledgeable treatment.
Surgery was oftentimes performed by a surgeon who knew it as a craft.
There were a handful of surgeons such as Henry de Mondeville, who were
very proficient and were employed by Kings such as King Phillip. However; this was not always enough to save kings’ lives, as King Richard I of England died of wounds at the siege of Chalus in AD 1199 due to an unskilled arrow extraction.
Wound treatment
Arrow extraction
Treating
a wound was and remains the most crucial part of any battlefield
medicine, as this is what keeps soldiers alive. As remains true on the
modern battlefield, hemorrhaging
and shock were the number one killers. Thus, the initial control of
these two things were of the utmost importance in medieval medicine. Items such as the long bow were used widely throughout the medieval period, thus making arrow
extracting a common practice among the armies of Medieval Europe. When
extracting an arrow, there were three guidelines that were to be
followed. The physicians should first examine the position of the arrow
and the degree to which its parts are visible, the possibility of it
being poisoned, the location of the wound, and the possibility of
contamination with dirt and other debris. The second rule was to
extract it delicately and swiftly. The third rule was to stop the flow
of blood from the wound.
The arrowheads that were used against troops were typically not barbed
or hooked, but were slim and designed to penetrate armor such as chain mail.
Although this design may be useful as wounds were smaller, these
arrows were more likely to embed in bone making them harder to extract.
If the arrow happened to be barbed or hooked it made the removal more
challenging. Physicians would then let the wound putrify, thus making
the tissue softer and easier for arrow extraction.
After a soldier was wounded he was taken to a field hospital where
the wound was assessed and cleaned, then if time permitted the soldier
was sent to a camp hospital where his wound was closed for good and
allowed to heal.
Blade and knife wounds
Another
common injury faced was those caused by blades. If the wound was too
advanced for simple stitch and bandage, it would often result in amputation
of the limb. Surgeons of the Medieval battlefield had the practice of
amputation down to an art. Typically it would have taken less than a
minute for a surgeon to remove the damaged limb, and another three to
four minutes to stop the bleeding.
The surgeon would first place the limb on a block of wood and tie
ligatures above and below the site of surgery. Then the soft tissue
would be cut through, thus exposing the bone, which was then sawed
through. The stump was then bandaged and left to heal. The rates of
mortality among amputation patients was around 39%, that number grew to
roughly 62% for those patients with a high leg amputation.
Ideas of medieval surgery are often construed in our modern mind as
barbaric, as our view is diluted with our own medical knowledge. Surgery
and medical practice in general was at its height of advancement for
its time. All procedures were done with the intent to save lives, not
to cause extra pain and suffering. The speed of the procedure by the
surgeon was an important factor, as the limit of pain and blood loss
lead to higher survival rates among these procedures. Injuries to major arteries that caused mass blood loss were not usually treatable as shown in the evidence of archeological remains.
We know this as wounds severe enough to sever major arteries left
incisions on the bone which is excavated by archaeologists. Wounds were
also taught to be covered to improve healing. Forms of antiseptics
were also used in order to stave off infection. To dress wounds all
sorts of dressing were used such as grease, absorbent dressings, spider
webs, honey, ground shellfish, clay and turpentine. Some of these
methods date back to Roman battlefield medicine.
Bone breakage
Sieges were a dangerous place to be, as broken bones became an issue, with soldiers falling while they scaled the wall among other methods of breakage. Typically, it was long bones that were fractured. These fractures were manipulated to get the bones back into their correct location.
Once they were in their correct location, the wound was immobilized by
either a splint or a plaster mold. The plaster mold (an early cast)
was made of flour and egg whites and was applied to the injured area.
Both of these methods left the bone immobilized and gave it a chance to
heal.
Burn treatment
Burn
treatment also required a specific approach by physicians of the time.
This was due to burning oil and arrows or boiling water, which were
used in combat. In the early stages of treatment there was an attempt
to stop the formation of blisters.
The burn was prevented from becoming dry by using anointments placed
on the burn. These anointments typically consisted of vinegar, egg,
rose oil, opium, and a multitude of different herbs. The ointment was applied to affected area, and then reapplied as needed.