Currently, bioprinting can be used to print tissues and organs to help research drugs and pills. However, emerging innovations span from bioprinting of cells or
extracellular matrix deposited into a 3D gel layer by layer to produce
the desired tissue or organ. In addition, 3D bioprinting has begun to
incorporate the printing of scaffolds. These scaffolds can be used to regenerate joints and ligaments.
Process

Bioprinting of 3D Convoluted Renal Proximal Tubules on Perfusable Chips
3D bioprinting generally follows three steps, pre-bioprinting, bioprinting, and post-bioprinting.
Pre-bioprinting
Pre-bioprinting
is the process of creating a model that the printer will later create
and choosing the materials that will be used. One of the first steps is
to obtain a biopsy of the organ. Common technologies used for
bioprinting are computed tomography (CT) and magnetic resonance imaging
(MRI). To print with a layer-by-layer approach, tomographic
reconstruction is done on the images. The now-2D images are then sent to
the printer to be made. Once the image is created, certain cells are
isolated and multiplied.
These cells are then mixed with a special liquefied material that
provides oxygen and other nutrients to keep them alive. In some
processes, the cells are encapsulated in cellular spheroids 500μm in
diameter. This aggregation of cells does not require a scaffold, and are
required for placing in the tubular-like tissue fusion for processes
such as extrusion.
Bioprinting
In the second step, the liquid mixture of cells, matrix, and nutrients known as bioinks are placed in a printer cartridge and deposited using the patients' medical scans. When a bioprinted pre-tissue is transferred to an incubator, this cell-based pre-tissue matures into a tissue.
3D bioprinting for fabricating biological constructs typically
involves dispensing cells onto a biocompatible scaffold using a
successive layer-by-layer approach to generate tissue-like
three-dimensional structures.
Artificial organs such as livers and kidneys made by 3D bioprinting
have been shown to lack crucial elements that affect the body such as
working blood vessels, tubules for collecting urine, and the growth of
billions of cells required for these organs. Without these components
the body has no way to get the essential nutrients and oxygen deep
within their interiors.
Given that every tissue in the body is naturally composed of different
cell types, many technologies for printing these cells vary in their
ability to ensure stability and viability of the cells during the
manufacturing process. Some of the methods that are used for 3D
bioprinting of cells are photolithography, magnetic bioprinting, stereolithography, and direct cell extrusion.
Post-bioprinting
The
post-bioprinting process is necessary to create a stable structure from
the biological material. If this process is not well-maintained, the
mechanical integrity and function of the 3D printed object is at risk.
To maintain the object, both mechanical and chemical stimulations are
needed. These stimulations send signals to the cells to control the
remodeling and growth of tissues. In addition, in recent development,
bioreactor technologies have allowed the rapid maturation of tissues, vascularization of tissues and the ability to survive transplants.
Bioreactors work in either providing convective nutrient
transport, creating microgravity environments, changing the pressure
causing solution to flow through the cells, or add compression for
dynamic or static loading. Each type of bioreactor is ideal for
different types of tissue, for example compression bioreactors are ideal
for cartilage tissue.
Bioprinting approach
Researchers
in the field have developed approaches to produce living organs that
are constructed with the appropriate biological and mechanical
properties. 3D bioprinting is based on three main approaches:
Biomimicry, autonomous self-assembly and mini-tissue building blocks.
Biomimicry
The
first approach of bioprinting is called biomimicry. The main goal of
this approach is to create fabricated structures that are identical to
the natural structure that are found in the tissues and organs in the
human body. Biomimicry requires duplication of the shape, framework, and
the microenvironment of the organs and tissues.
The application of biomimicry in bioprinting involves creating both
identical cellular and extracellular parts of organs. For this approach
to be successful, the tissues must be replicated on a micro scale.
Therefore, it is necessary to understand the microenvironment, the
nature of the biological forces in this microenvironment, the precise
organization of functional and supporting cell types, solubility
factors, and the composition of extracellular matrix.
Autonomous self-assembly
The
second approach of bioprinting is autonomous self-assembly. This
approach relies on the physical process of embryonic organ development
as a model to replicate the tissues of interest.
When cells are in their early development, they create their own
extracellular matrix building block, the proper cell signaling, and
independent arrangement and patterning to provide the required
biological functions and micro-architecture.
Autonomous self-assembly demands specific information about the
developmental techniques of the tissues and organs of the embryo.
There is a "scaffold-free" model that uses self-assembling spheroids
that subjects to fusion and cell arrangement to resemble evolving
tissues. Autonomous self-assembly depends on the cell as the fundamental
driver of histogenesis, guiding the building blocks, structural and
functional properties of these tissues. It demands a deeper
understanding of how embryonic tissues mechanisms develop as well as the
microenvironment surrounded to create the bioprinted tissues.
Mini-tissue
The
third approach of bioprinting is a combination of both the biomimicry
and self-assembly approaches, which is called mini tissues.
Organs and tissues are built from very small functional components.
Mini-tissue approach takes these small pieces and manufacture and
arrange them into larger framework.
Printers
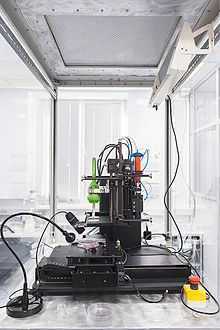
Printer from 3D Bioprinting Solutions
Akin to ordinary ink printers, bioprinters have three major
components to them. These are the hardware used, the type of bio-ink,
and the material it is printed on (biomaterials).
"Bio-ink is a material made from living cells that behaves much like a
liquid, allowing people to "print" it in order to create a desired
shape. To make bio-ink, scientists create a slurry of cells that can be
loaded into a cartridge and inserted into a specially designed printer,
along with another cartridge containing a gel known as bio-paper."
In bioprinting, there are three major types of printers that have
been used. These are inkjet, laser-assisted, and extrusion printers.
Inkjet printers are mainly used in bioprinting for fast and large-scale
products. One type of inkjet printer, called drop-on-demand inkjet
printer, prints materials in exact amounts, minimizing cost and waste.
Printers that utilize lasers provide high-resolution printing; however,
these printers are often expensive. Extrusion printers print cells
layer-by-layer, just like 3D printing to create 3D constructs. In addition to just cells, extrusion printers may also use hydrogels infused with cells.
Impact
3D bioprinting contributes to significant advances in the medical field of tissue engineering by allowing for research to be done on innovative materials called biomaterials.
Biomaterials are the materials adapted and used for printing
three-dimensional objects. Some of the most notable bioengineered
substances are usually stronger than the average bodily materials,
including soft tissue and bone. These constituents can act as future
substitutes, even improvements, for the original body materials. Alginate,
for example, is an anionic polymer with many biomedical implications
including feasibility, strong biocompatibility, low toxicity, and
stronger structural ability in comparison to some of the body's
structural material.
Synthetic hydrogels are also commonplace, including PV-based gels. The
combination of acid with a UV-initiated PV-based cross-linker has been
evaluated by the Wake Forest Institute of Medicine and determined to be a
suitable biomaterial.
Engineers are also exploring other options such as printing
micro-channels that can maximize the diffusion of nutrients and oxygen
from neighboring tissues In addition, the Defense Threat Reduction Agency
aims to print mini organs such as hearts, livers, and lungs as the
potential to test new drugs more accurately and perhaps eliminate the
need for testing in animals.