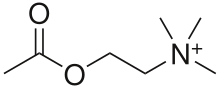
Acetylcholine - the natural agonist of muscarinic and nicotinic receptors.
Muscarine - an agonist used to distinguish between these two classes of receptors. Not normally found in the body.
Atropine - an antagonist.
Muscarinic acetylcholine receptors, or mAChRs, are acetylcholine receptors that form G protein-coupled receptor complexes in the cell membranes of certain neurons and other cells. They play several roles, including acting as the main end-receptor stimulated by acetylcholine released from postganglionic fibers in the parasympathetic nervous system.
Muscarinic receptors are so named because they are more sensitive to muscarine than to nicotine. Their counterparts are nicotinic acetylcholine receptors (nAChRs), receptor ion channels that are also important in the autonomic nervous system. Many drugs and other substances (for example pilocarpine and scopolamine) manipulate these two distinct receptors by acting as selective agonists or antagonists.
Function
Acetylcholine (ACh) is a neurotransmitter found in the brain, neuromuscular junctions and the autonomic ganglia.
Muscarinic receptors are used in the following roles:
Recovery receptors
The structure of Muscarinic acetylcholine receptor M2.
ACh is always used as the transmitter within the autonomic ganglion. Nicotinic receptors on the postganglionic neuron are responsible for the initial fast depolarization (Fast EPSP) of that neuron. As a consequence of this, nicotinic receptors are often cited as the receptor on the postganglionic neurons at the ganglion. However, the subsequent hyperpolarization (IPSP)
and slow depolarization (Slow EPSP) that represent the recovery of the
postganglionic neuron from stimulation are actually mediated by muscarinic receptors, types M2 and M1 respectively (discussed below).
Peripheral autonomic fibers (sympathetic and parasympathetic
fibers) are categorized anatomically as either preganglionic or
postganglionic fibers, then further generalized as either adrenergic
fibers, releasing noradrenaline, or cholinergic fibers, both releasing
acetylcholine and expressing acetylcholine receptors. Both preganglionic
sympathetic fibers and preganglionic parasympathetic fibers are
cholinergic. Most postganglionic sympathetic fibers are adrenergic:
their neurotransmitter is norepinephrine; postganglionic sympathetic
fibers to the sweat glands, piloerectile muscles of the body hairs, and
the skeletal muscle arterioles do not use adrenaline/noradrenaline.
The adrenal medulla
is considered a sympathetic ganglion and, like other sympathetic
ganglia, is supplied by cholinergic preganglionic sympathetic fibers:
acetylcholine is the neurotransmitter utilized at this synapse. The chromaffin cells
of the adrenal medulla act as "modified neurons", releasing adrenaline
and noradrenaline into the bloodstream as hormones instead of as
neurotransmitters. The other postganglionic fibers of the peripheral
autonomic system belong to the parasympathetic division; all are
cholinergic fibers, and use acetylcholine as the neurotransmitter.
Postganglionic neurons
Another
role for these receptors is at the junction of the innervated tissues
and the postganglionic neurons in the parasympathetic division of the
autonomic nervous system. Here acetylcholine is again used as a
neurotransmitter, and muscarinic receptors form the principal receptors on the innervated tissue.
Innervated tissue
Very few parts of the sympathetic system use cholinergic receptors. In sweat glands the receptors are of the muscarinic type. The sympathetic nervous system also has some preganglionic nerves terminating at the chromaffin cells in the adrenal medulla, which secrete epinephrine and norepinephrine
into the bloodstream. Some believe that chromaffin cells are modified
postganglionic CNS fibers. In the adrenal medulla, acetylcholine is used
as a neurotransmitter, and the receptor is of the nicotinic type.
The somatic nervous system uses a nicotinic receptor to acetylcholine at the neuromuscular junction.
Higher central nervous system
Muscarinic
acetylcholine receptors are also present and distributed throughout the
local nervous system, in post-synaptic and pre-synaptic positions.
There is also some evidence for postsynaptic receptors on sympathetic neurons allowing the parasympathetic nervous system to inhibit sympathetic effects.
Presynaptic membrane of the neuromuscular junction
It
is known that muscarinic acetylcholine receptors also appear on the
pre-synaptic membrane of somatic neurons in the neuro-muscular junction,
where they are involved in the regulation of acetylcholine release.
Form of muscarinic receptors
Muscarinic acetylcholine receptors belong to a class of metabotropic receptors that use G proteins as their signaling mechanism. In such receptors, the signaling molecule (the ligand) binds to a receptor that has seven transmembrane regions;
in this case, the ligand is ACh. This receptor is bound to
intracellular proteins, known as G proteins, which begin the information
cascade within the cell.
By contrast, nicotinic receptors use a ligand-gated ion channel mechanism for signaling. In this case, binding of the ligands with the receptor causes an ion channel to open, permitting either one or more specific type(s) of ion (e.g., K+, Na+, Ca2+) to diffuse into or out of the cell.
Receptor isoforms
Classification
By
the use of selective radioactively labeled agonist and antagonist
substances, five subtypes of muscarinic receptors have been determined,
named M1-M5 (using an upper case M and subscript number). M1,M3,M5 receptors are coupled with Gq proteins, while M2 and M4 receptors are coupled with Gi/o proteins. There are other classification systems. For example, the drug pirenzepine is a muscarinic antagonist (decreases the effect of ACh), which is much more potent at M1
receptors than it is at other subtypes. The acceptance of the various
subtypes has proceeded in numerical order: therefore, sources that
recognize only the M1/M2 distinction exist. More recent studies tend to recognize M3 and the most recent M4.
Genetic differences
Meanwhile, geneticists and molecular biologists
have characterised five genes that appear to encode muscarinic
receptors, named m1-m5 (lowercase m; no subscript number). The first
four code for pharmacologic types M1-M4. The fifth, M5,
corresponds to a subtype of receptor that had until recently not been
detected pharmacologically. The receptors m1 and m2 were determined
based upon partial sequencing of M1 and M2 receptor proteins. The others were found by searching for homology, using bioinformatic techniques.
Difference in G proteins
G proteins contain an alpha-subunit that is critical to the
functioning of receptors. These subunits can take a number of forms.
There are four broad classes of form of G-protein: Gs, Gi, Gq, and G12/13.
Muscarinic receptors vary in the G protein to which they are bound,
with some correlation according to receptor type. G proteins are also
classified according to their susceptibility to cholera toxin (CTX) and pertussis toxin (PTX, whooping cough). Gs and some subtypes of Gi (Gαt and Gαg) are susceptible to CTX. Only Gi is susceptible to PTX, with the exception of one subtype of Gi (Gαz)
which is immune. Also, only when bound with an agonist, those G
proteins normally sensitive to PTX also become susceptible to CTX.
The various G-protein subunits act differently upon secondary
messengers, upregulating Phospholipases, downregulating cAMP, etc.
Because of the strong correlations to muscarinic receptor type,
CTX and PTX are useful experimental tools in investigating these
receptors.
M1 receptor
This receptor is found mediating slow EPSP at the ganglion in the postganglionic nerve[citation needed], is common in exocrine glands and in the CNS.
It is predominantly found bound to G proteins of class Gq, which use upregulation of phospholipase C and, therefore, inositol trisphosphate and intracellular calcium as a signaling pathway. A receptor so bound would not be susceptible to CTX or PTX. However, Gi (causing a downstream decrease in cAMP) and Gs
(causing an increase in cAMP) have also been shown to be involved in
interactions in certain tissues, and so would be susceptible to PTX and
CTX, respectively.
M2 receptor
The M2 muscarinic receptors are located in the heart, where they act to slow the heart rate down to normal sinus rhythm, by slowing the speed of depolarization.
In humans under resting conditions vagal activity dominates over
sympathetic activity. Hence inhibition of m2 receptors (e.g. by
atropine) will cause a raise in heart rate. They also moderately reduce
contractile forces of the atrial cardiac muscle, and reduce conduction velocity of the atrioventricular node (AV node). It also serves to slightly decrease the contractile forces of the ventricular muscle.
M2 muscarinic receptors act via a Gi type receptor, which causes a decrease in cAMP in the cell, inhibition of voltage-gated Ca2+ channels, and increasing efflux of K+, in general, leading to inhibitory-type effects.
M3 receptor
The M3 muscarinic receptors are located at many places in
the body. They are located in the smooth muscles of the blood vessels,
as well as in the lungs. Because the M3 receptor is Gq-coupled
and mediates an increase in intracellular calcium, it typically causes
contraction of smooth muscle, such as that observed during bronchoconstriction and bladder voiding. However, with respect to vasculature, activation of M3
on vascular endothelial cells causes increased synthesis of nitric
oxide, which diffuses to adjacent vascular smooth muscle cells and
causes their relaxation, thereby explaining the paradoxical effect of
parasympathomimetics on vascular tone and bronchiolar tone. Indeed,
direct stimulation of vascular smooth muscle, M3 mediates vasconstriction in pathologies wherein the vascular endothelium is disrupted.
The M3 receptors are also located in many glands, which help
to stimulate secretion in, for example, the salivary glands, as well as
other glands of the body.
Like the M1 muscarinic receptor, M3 receptors are G proteins of class Gq that upregulate phospholipase C and, therefore, inositol trisphosphate and intracellular calcium as a signaling pathway.
M4 receptor
M4 receptors are found in the CNS.
Receptors work via Gi receptors to decrease cAMP in the cell and, thus, produce generally inhibitory effects. Possible bronchospasm may result if stimulated by muscarinic agonists
M5 receptor
Location of M5 receptors is not well known.
Like the M1 and M3 muscarinic receptor, M5 receptors are coupled with G proteins of class Gq that upregulate phospholipase C and, therefore, inositol trisphosphate and intracellular calcium as a signaling pathway.
Pharmacological application
Ligands targeting the mAChR that are currently approved for clinical use include non-selective antagonists for the treatment of Parkinson's disease, atropine (to dilate the pupil), scopolamine (used to prevent motion sickness), and ipratropium (used in the treatment of COPD).