| Vitamin D | |
|---|---|

Cholecalciferol (D3)
| |
| Class identifiers | |
| Use | Rickets, osteoporosis, vitamin D deficiency |
| ATC code | A11CC |
| Biological target | vitamin D receptor |
| Clinical data | |
| Drugs.com | MedFacts Natural Products |
| External links | |
| MeSH | D014807 |
Vitamin D is a group of fat-soluble secosteroids responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, and multiple other biological effects. In humans, the most important compounds in this group are vitamin D3 (also known as cholecalciferol) and vitamin D2 (ergocalciferol). Cholecalciferol and ergocalciferol can be ingested from the diet and from supplements. Only a few foods contain vitamin D. The major natural source of the vitamin is synthesis of cholecalciferol in the skin from cholesterol through a chemical reaction that is dependent on sun exposure (specifically UVB radiation). Dietary recommendations typically assume that all of a person's vitamin D is taken by mouth, as sun exposure in the population is variable and recommendations about the amount of sun exposure that is safe are uncertain in view of the skin cancer risk.
Vitamin D from the diet, or from skin synthesis, is biologically inactive. A protein enzyme must hydroxylate it to convert it to the active form. This is done in the liver and in the kidneys. As vitamin D can be synthesized in adequate amounts by most mammals exposed to sufficient sunlight, it is not an essential dietary factor, and so not technically a vitamin. Instead it could be considered a hormone, with activation of the vitamin D pro-hormone resulting in the active form, calcitriol, which then produces effects via a nuclear receptor in multiple locations. Cholecalciferol is converted in the liver to calcifediol (25-hydroxycholecalciferol); ergocalciferol is converted to 25-hydroxyergocalciferol. These two vitamin D metabolites (called 25-hydroxyvitamin D or 25(OH)D) are measured in serum to determine a person's vitamin D status. Calcifediol is further hydroxylated by the kidneys to form calcitriol (also known as 1,25-dihydroxycholecalciferol), the biologically active form of vitamin D. Calcitriol circulates as a hormone in the blood, having a major role regulating the concentration of calcium and phosphate, and promoting the healthy growth and remodeling of bone. Calcitriol also has other effects, including some on cell growth, neuromuscular and immune functions, and reduction of inflammation.
Vitamin D has a significant role in calcium homeostasis and metabolism. Its discovery was due to effort to find the dietary substance lacking in children with rickets (the childhood form of osteomalacia). Vitamin D supplements are given to treat or to prevent osteomalacia and rickets, but the evidence for other health effects of vitamin D supplementation in the general population is inconsistent. The effect of vitamin D supplementation on mortality is not clear, with one meta-analysis finding a small decrease in mortality in elderly people, and another concluding no clear justification exists for recommending supplementation for preventing many diseases, and that further research of similar design is unneeded in these areas.
Types
| Name | Chemical composition | Structure |
|---|---|---|
| Vitamin D1 | Mixture of molecular compounds of ergocalciferol with lumisterol, 1:1 |
|
| Vitamin D2 | ergocalciferol (made from ergosterol) | 
|
| Vitamin D3 | cholecalciferol (made from 7-dehydrocholesterol in the skin). | 
|
| Vitamin D4 | 22-dihydroergocalciferol | 
|
| Vitamin D5 | sitocalciferol (made from 7-dehydrositosterol) | 
|
Several forms (vitamers) of vitamin D exist. The two major forms are vitamin D2 or ergocalciferol, and vitamin D3 or cholecalciferol; vitamin D without a subscript refers to either D2 or D3 or both. These are known collectively as calciferol. Vitamin D2 was chemically characterized in 1931. In 1935, the chemical structure of vitamin D3 was established and proven to result from the ultraviolet irradiation of 7-dehydrocholesterol.
Chemically, the various forms of vitamin D are secosteroids, i.e., steroids in which one of the bonds in the steroid rings is broken. The structural difference between vitamin D2 and vitamin D3 is the side chain of D2 contains a double bond between carbons 22 and 23, and a methyl group on carbon 24.
Biology
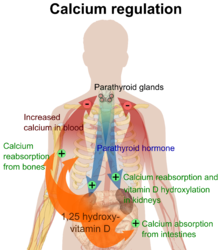
Calcium regulation in the human body. The role of active vitamin D (1,25-dihydroxyvitamin D, calcitriol) is shown in orange.
The active vitamin D metabolite calcitriol mediates its biological effects by binding to the vitamin D receptor (VDR), which is principally located in the nuclei of target cells. The binding of calcitriol to the VDR allows the VDR to act as a transcription factor that modulates the gene expression of transport proteins (such as TRPV6 and calbindin), which are involved in calcium absorption in the intestine. The vitamin D receptor belongs to the nuclear receptor superfamily of steroid/thyroid hormone receptors, and VDRs are expressed by cells in most organs, including the brain, heart, skin, gonads, prostate, and breast.
VDR activation in the intestine, bone, kidney, and parathyroid
gland cells leads to the maintenance of calcium and phosphorus levels in
the blood (with the assistance of parathyroid hormone and calcitonin) and to the maintenance of bone content.
One of the most important roles of vitamin D is to maintain skeletal calcium balance by promoting calcium absorption in the intestines, promoting bone resorption by increasing osteoclast number, maintaining calcium and phosphate levels for bone formation, and allowing proper functioning of parathyroid hormone to maintain serum calcium levels. Vitamin D deficiency can result in lower bone mineral density and an increased risk of reduced bone density (osteoporosis) or bone fracture because a lack of vitamin D alters mineral metabolism in the body. Thus, vitamin D is also critical for bone remodeling through its role as a potent stimulator of bone resorption.
The VDR regulates cell proliferation and differentiation. Vitamin D also affects the immune system, and VDRs are expressed in several white blood cells, including monocytes and activated T and B cells. In vitro, vitamin D increases expression of the tyrosine hydroxylase gene in adrenal medullary cells, and affects the synthesis of neurotrophic factors, nitric oxide synthase, and glutathione.
Deficiency
A diet deficient in vitamin D in conjunction with inadequate sun
exposure causes osteomalacia (or rickets when it occurs in children),
which is a softening of the bones. In the developed world, this is a
rare disease. However, vitamin D deficiency has become a worldwide problem in the elderly and remains common in children and adults. Low blood calcifediol (25-hydroxy-vitamin D) can result from avoiding the sun. Deficiency results in impaired bone mineralization and bone damage which leads to bone-softening diseases, including rickets and osteomalacia. Being deficient in vitamin D can cause intestinal absorption of dietary calcium to fall to 15%. When not deficient, an individual usually absorbs between 60-80%.
Bone health
Rickets
Rickets, a childhood disease, is characterized by impeded growth and soft, weak, deformed long bones that bend and bow under their weight as children start to walk. This condition is characterized by bow legs,
which can be caused by calcium or phosphorus deficiency, as well as a
lack of vitamin D; today, it is largely found in low-income countries in
Africa, Asia, or the Middle East and in those with genetic disorders such as pseudovitamin D deficiency rickets.
Maternal vitamin D deficiency may cause overt bone disease from before birth and impairment of bone quality after birth.
Nutritional rickets exists in countries with intense year-round
sunlight such as Nigeria and can occur without vitamin D deficiency.
Although rickets and osteomalacia are now rare in the UK,
outbreaks have happened in some immigrant communities in which
osteomalacia sufferers included women with seemingly adequate daylight
outdoor exposure wearing Western clothing.
Having darker skin and reduced exposure to sunshine did not produce
rickets unless the diet deviated from a Western omnivore pattern
characterized by high intakes of meat, fish, and eggs, and low intakes
of high-extraction cereals. The dietary risk factors for rickets include abstaining from animal foods.
Vitamin D deficiency remains the main cause of rickets among
young infants in most countries, because breast milk is low in vitamin D
and social customs and climatic conditions can prevent adequate sun
exposure. In sunny countries such as Nigeria, South Africa, and
Bangladesh, where rickets occurs among older toddlers and children, it
has been attributed to low dietary calcium intakes, which are
characteristic of cereal-based diets with limited access to dairy
products.
Rickets was formerly a major public health problem among the US population; in Denver, where ultraviolet rays are about 20% stronger than at sea level on the same latitude, almost two-thirds of 500 children had mild rickets in the late 1920s. An increase in the proportion of animal protein in the 20th century American diet coupled with increased consumption of milk fortified with relatively small quantities of vitamin D coincided with a dramatic decline in the number of rickets cases.
Also, in the United States and Canada, vitamin D-fortified milk, infant
vitamin supplements, and vitamin supplements have helped to eradicate
the majority of cases of rickets for children with fat malabsorption
conditions.
Osteoporosis and osteomalacia
Osteomalacia
is a disease in adults that results from vitamin D deficiency.
Characteristics of this disease are softening of the bones, leading to
bending of the spine, bowing of the legs, proximal muscle weakness, bone fragility, and increased risk for fractures.
Osteomalacia reduces calcium absorption and increases calcium loss from
bone, which increases the risk for bone fractures. Osteomalacia is
usually present when 25-hydroxyvitamin D levels are less than about
10 ng/mL. Although the effects of osteomalacia are thought to contribute to chronic musculoskeletal pain, there is no persuasive evidence of lower vitamin D levels in chronic pain sufferers or that supplementation alleviates chronic nonspecific musculoskeletal pain.
Skin pigmentation
Dark-skinned
people living in temperate climates have been shown to have low vitamin
D levels but the significance of this is not certain. Dark-skinned people are less efficient at making vitamin D because melanin in the skin hinders vitamin D synthesis.
Use of supplements
The effects of vitamin D supplementation on health are uncertain.
A 2013 review did not find any effect from supplementation on the rates
of disease, other than a tentative decrease in mortality in the
elderly. Vitamin D supplements do not alter the outcomes for myocardial infarction, stroke or cerebrovascular disease, cancer, bone fractures or knee osteoarthritis. Low vitamin D levels may result from disease rather than cause disease.
A United States Institute of Medicine report states: "Outcomes related to cancer, cardiovascular disease and hypertension, and diabetes and metabolic syndrome, falls and physical performance, immune functioning and autoimmune disorders, infections, neuropsychological functioning, and preeclampsia could not be linked reliably with calcium or vitamin D intake and were often conflicting."
Some researchers claim the IOM was too definitive in its
recommendations and made a mathematical mistake when calculating the
blood level of vitamin D associated with bone health.
Members of the IOM panel maintain that they used a "standard procedure
for dietary recommendations" and that the report is solidly based on the
data. Research on vitamin D supplements, including large-scale clinical
trials, is continuing.
Mortality, all-cause
Vitamin D3 supplementation has been tentatively found to lead to a reduced risk of death in the elderly, but the effect has not been deemed pronounced or certain enough to make taking supplements recommendable. Other forms (vitamin D2, alfacalcidol, and calcitriol) do not appear to have any beneficial effects with regard to the risk of death.
High blood levels appear to be associated with a lower risk of death,
but it is unclear if supplementation can result in this benefit. Both an excess and a deficiency in vitamin D appear to cause abnormal functioning and premature aging. The relationship between serum calcifediol level and all-cause mortality is parabolic. Harm from vitamin D appears to occur at a lower vitamin D level in the black population than in the white population.
Bone health
In general, no good evidence supports the commonly held belief that vitamin D supplements can help prevent osteoporosis. Its general use for prevention of this disease in those without vitamin D deficiency is thus likely not needed.
For older people with osteoporosis, taking vitamin D with calcium may
help prevent hip fractures, but it also slightly increases the risk of
stomach and kidney problems. Supplementation with higher doses of vitamin D, in those older than 65 years, may decrease fracture risk. The effect is small or none for people living independently. Low serum vitamin D levels have been associated with falls, and low bone mineral density. Taking extra vitamin D, however, does not appear to change the risk. Athletes who are vitamin D deficient are at an increased risk of stress fractures
and/or major breaks, particularly those engaging in contact sports. The
greatest benefit with supplementation is seen in athletes who are
deficient (25(OH)D serum levels less than 30 ng/mL), or severely deficient
(25(OH)D serum levels less than 25 ng/mL). Incremental decreases in risks are
observed with rising serum 25(OH)D concentrations plateauing at
50 ng/mL with no additional benefits seen in levels beyond this point.
Because it found mounting evidence for a benefit to bone health,
though it had not found good evidence of other benefits, the US Food and Drug Administration has required manufacturers to declare the amount of vitamin D on nutrition facts labels,
as "nutrients of public health significance", since May 2016. By a
proposed deadline extension, small manufacturers with less than $10
million in annual food sales will have to comply by 1 Jan 2021, while
larger ones have to comply by 1 Jan 2020.
Cancer
Vitamin D supplements have been widely marketed for their claimed anticancer properties.
Associations have been shown in observational studies between low
vitamin D levels and the risk of development of certain cancers. It is unclear, however, if taking additional vitamin D in the diet or as supplements affects the risk of cancer.
Reviews have described the evidence as being "inconsistent,
inconclusive as to causality, and insufficient to inform nutritional
requirements" and "not sufficiently robust to draw conclusions". One 2014 review found that supplements had no significant effect on cancer risk. Another 2014 review concluded that vitamin D3
may decrease the risk of death from cancer (one fewer death in 150
people treated over 5 years), but concerns with the quality of the data
were noted. Insufficient evidence exists to recommend vitamin D supplements for people with cancer, although some evidence suggests that low vitamin D may be associated with a worse outcome for some cancers, and that higher 25-hydroxy vitamin D levels at the time of diagnosis are associated with better outcomes.
Cardiovascular disease
Taking vitamin D supplements does not meaningfully reduce the risk of stroke, cerebrovascular disease, cardial infarction, or ischaemic heart disease. Supplementation may have no effect on blood pressure.
Immune system
Infectious diseases
In general, vitamin D functions to activate the innate and dampen the adaptive immune systems. Deficiency has been linked to increased risk or severity of viral infections, including HIV. Low levels of vitamin D appear to be a risk factor for tuberculosis, and historically it was used as a treatment. Supplementation slightly decreases the risk of acute respiratory tract infections and the exacerbation of asthma. Evidence is lacking on whether it does so in children under five years of age. No clinical trials have been done to assess its effect on preventing other infections, such as malaria.
Autoimmune diseases
Although tentative data link low levels of vitamin D to asthma, evidence to support a beneficial effect on asthmatics from supplementation is inconclusive. Accordingly, supplementation is not currently recommended for treatment or prevention of asthma. Vitamin D and multiple sclerosis incidence have been linked, but it is not clear what the nature of any causal relationship might be.
Two systemic reviews concluded that the evidence for vitamin D
supplementation being helpful for treating people with multiple
sclerosis is inconclusive.
Inflammatory bowel disease
Low levels of vitamin D are associated with two major forms of human Inflammatory bowel disease (IBD): Crohn's disease and ulcerative colitis. However, further studies are required to determine its significance and the potential role of vitamin D axis in IBD.
Other conditions
Diabetes
-- A systematic review of 2014 concluded that the available studies
show no evidence of vitamin D3 supplementation having an effect on
glucose homeostasis or diabetes prevention.
A review article of 2016 reported that while there is increasing
evidence that vitamin D deficiency may be a risk factor for diabetes,
over-all evidence regarding vitamin D levels and diabetes mellitus is
contradictory, requiring further studies.
Depression -- Clinical trials of vitamin D
supplementation for depressive symptoms have generally been of low
quality and show no overall effect, although subgroup analysis showed
supplementation for participants with clinically significant depressive
symptoms or depressive disorder had a moderate effect.
Cognition and dementia -- A systematic review of clinical studies found an association between low vitamin D levels with cognitive impairment and a higher risk of developing Alzheimer's disease.
However, lower vitamin D concentrations are also associated with poor
nutrition and spending less time outdoors. Therefore, alternative
explanations for the increase in cognitive impairment exist and hence a
direct causal relationship between vitamin D levels and cognition could
not be established.
Pregnancy -- Low levels of vitamin D in pregnancy are associated with gestational diabetes, pre-eclampsia, and small (for gestational age) infants. Although taking vitamin D supplements during pregnancy raises blood levels of vitamin D in the mother at term, the extent of benefits for the mother or baby is unclear. Pregnant women who take an adequate amount of vitamin D during gestation may experience a lower risk of pre-eclampsia and positive immune effects. A 2018 review found that supplements may reduce the risk of undersized babies and of their poor rate of growth. Pregnant women often do not take the recommended amount of vitamin D.
Weight loss -- Though hypothesized that vitamin D supplementation may be an effective treatment for obesity apart from calorie restriction, one systematic review found no association of supplementation with body weight or fat mass. A 2016 meta-analysis
found that circulating vitamin D status was improved by weight loss,
indicating that fat mass may be inversely associated with blood levels
of vitamin D.
Allowable health claims
Governmental
regulatory agencies stipulate for the food and dietary supplement
industries certain health claims as allowable as statements on
packaging.
- normal function of the immune system
- normal inflammatory response
- normal muscle function
- reduced risk of falling in people over age 60
- "Adequate calcium and vitamin D, as part of a well balanced diet, along with physical activity, may reduce the risk of osteoporosis."
- Adequate calcium and regular exercise may help to achieve strong bones in children and adolescents and may reduce the risk of osteoporosis in older adults. An adequate intake of vitamin D is also necessary
Other possible agencies with claim guidance: Japan FOSHU and Australia-New Zealand.
Dietary intake
Recommended levels
Conversion: 1 µg = 40 IU.
Various institutions have proposed different recommendations for the amount of daily intake
of vitamin D. These vary according to precise definition, age,
pregnancy or lactation, and the extent assumptions are made regarding
skin synthesis of vitamin D.
United States
The dietary reference intake for vitamin D issued in 2010 by the Institute of Medicine (renamed National Academy of Medicine
in 2015), superseded previous recommendations which were expressed in
terms of Adequate Intake. The recommendations were formed assuming the
individual has no skin synthesis of vitamin D because of inadequate sun
exposure. The reference intake for vitamin D refers to total intake from
food, beverages and supplements, and assumes that calcium requirements
are being met. The tolerable upper intake level
(UL) is defined as "the highest average daily intake of a nutrient that
is likely to pose no risk of adverse health effects for nearly all
persons in the general population."
Although ULs are believed to be safe, information on the long-term
effects is incomplete and these levels of intake are not recommended for
long-term consumption.
For U.S food and dietary supplement labeling purposes, the amount
in a serving is expressed as a percent of Daily Value (%DV). For
vitamin D labeling purposes, 100% of the Daily Value was 400 IU (10 μg),
but on May 27, 2016 it was revised to 800 IU (20 μg) to bring it into
agreement with the RDA. The deadline to be in compliance was extended to January 1, 2020 for large companies and January 1, 2021 for small companies.
Canada
Health Canada published recommended dietary allowances (RDA) and tolerable upper intake levels for vitamin D in 2012 based on the Institute of Medicine report.
Australia and New Zealand
Australia and New Zealand published nutrient reference values including guidelines for dietary vitamin D intake in 2005. About a third of Australians have vitamin D deficiency.
European Union
The European Food Safety Authority (EFSA) in 2016
reviewed the current evidence, finding the relationship between serum
25(OH)D concentration and musculoskeletal health outcomes is widely
variable. They considered that average requirements and population
reference intakes values for vitamin D cannot be derived, and that a
serum 25(OH)D concentration of 50 nmol/L was a suitable target value.
For all people over the age of 1, including women who are pregnant or
lactating, they set an adequate intake of 15 μg/day (600 IU).
The EFSA reviewed safe levels of intake in 2012, setting the tolerable upper limit for adults at 100 μg/day (4000 IU), a similar conclusion as the IOM.
The UK National Health Service
recommends babies and young children aged six months to five years,
pregnant or breastfeeding women, and sun-deprived elderly people should
take daily vitamin supplements to ensure sufficient vitamin D intake. In July 2016, Public Health England
recommended that everyone consider taking a daily supplement containing
10 µg of vitamin D during autumn and winter because of inadequate
sunlight for vitamin D synthesis.
The Swedish Food Administration recommends a daily intake of 10
μg (400 IU) of vitamin D3 for children and adults up to 75 years, and 20
μg (800 IU) for adults 75 and older.
Non-government organisations in Europe have made their own recommendations. The German Society for Nutrition recommends 20 µg.
The European Menopause and Andropause Society recommends postmenopausal
women consume15 µg (600 IU) until age 70, and 20 µg (800 IU) from age
71. This dose should be increased to 100 µg (4,000 IU) in some patients
with very low vitamin D status or in case of co-morbid conditions.
Sources
Although vitamin D is not present naturally in most foods, it is commonly added as a fortification in manufactured foods. In some countries, staple foods are artificially fortified with vitamin D.
Natural sources
In general, vitamin D2 is found in fungi and vitamin D3 is found in animals. Vitamin D2 is produced by ultraviolet irradiation of ergosterol found in many fungi. The vitamin D2 content in mushrooms and Cladina arbuscula, a lichen, increase with exposure to ultraviolet light. This process is emulated by industrial ultraviolet lamps, concentrating vitamin D2 levels to higher levels.
The United States Department of Agriculture reports D2 and D3 content combined in one value.
- Fungal sources
- C. arbuscula (lichen), thalli, dry: vitamin D3 0.67 to 2.04 μg/g (27 to 82 IU/g); vitamin D2 0.22-0.55 μg/g (8.8 to 22 IU/g).
- Agaricus bisporus (common mushroom), D2 + D3, per 100 grams (3.5 oz):
- Raw portobello: 0.3 μg (10 IU); exposed to ultraviolet light: 11.2 µg (446 IU)
- Raw crimini: 0.1 μg (3 IU); exposed to ultraviolet light: 31.9 µg (1276 IU)
- Animal sources
- Fish liver oils, such as cod liver oil, 450 IU per teaspoon (4.5 g); (100 IU/g)
- Fatty fish species, such as:
- Salmon, pink, cooked, dry heat, 100 grams (3.5 oz): 522 IU (5.2 IU/g)
- Mackerel, Pacific and jack, mixed species, cooked, dry heat, 100 grams (3.5 oz): 457 IU (4.6 IU/g)
- Tuna, canned in oil, 100 grams (3.5 oz): 269 IU (2.7 IU/g)
- Sardines, canned in oil, drained, 100 grams (3.5 oz): 193 IU (1.9 IU/g)
- Cooked egg yolk: 44 IU for a 61 g egg (0.7 IU/g)
- Beef liver, cooked, braised, 100 grams (3.5 oz): 49 IU (0.5 IU/g)
Food fortification
Manufactured foods fortified with vitamin D include some fruit juices and fruit juice drinks, meal replacement energy bars, soy protein-based beverages, certain cheese and cheese products, flour products, infant formulas, many breakfast cereals, and milk.
In 2016 in the United States, the Food and Drug Administration (FDA) amended food additive regulations for milk fortification, stating that vitamin D3 levels not exceed 42 IU vitamin D per 100 g (400 IU per US quart) of dairy milk, 84 IU of vitamin D2 per 100 g (800 IU per quart) of plant milks, and 89 IU per 100 g (800 IU per quart) in plant-based yogurts.
Plant milks are defined as beverages made from soy, almond, rice, among
other plant sources intended as alternatives to dairy milk.
While some studies have found that vitamin D3 raises 25(OH)D blood levels faster and remains active in the body longer, others contend that vitamin D2 sources are equally bioavailable and effective as D3 for raising and sustaining 25(OH)D.
Food preparation
Vitamin
D content in typical foods is reduced variably by cooking. Boiled,
fried and baked foods retained 69–89% of original vitamin D.
Recommended serum levels
Recommendations on recommended 25(OH)D serum levels vary across authorities, and vary based on factors like age.
US labs generally report 25(OH)D levels in ng/mL. Other countries
often use nmol/L. One ng/mL is approximately equal to 2.5 nmol/L.
A 2014 review concluded that the most advantageous serum levels
for 25(OH)D for all outcomes appeared to be close to 30 ng/mL (75
nmol/L).
The optimal vitamin D levels are still controversial and another
review concluded that ranges from 30 to 40 ng/mL (75 to 100 nmol/L) were
to be recommended for athletes.
Part of the controversy is because numerous studies have found
differences in serum levels of 25(OH)D between ethnic groups; studies
point to genetic as well as environmental reasons behind these
variations. Supplementation to achieve these standard levels could cause harmful vascular calcification.
A 2012 meta-analysis showed that the risk of cardiovascular diseases
increases when blood levels of vitamin D are lowest in a range of 8 to
24 ng/mL (20 to 60 nmol/L), although results among the studies analyzed
were inconsistent.
In 2011 an IOM
committee concluded a serum 25(OH)D level of 20 ng/mL (50 nmol/L) is
needed for bone and overall health. The dietary reference intakes for
vitamin D are chosen with a margin of safety and 'overshoot' the
targeted serum value to ensure the specified levels of intake achieve
the desired serum 25(OH)D levels in almost all persons. No contributions
to serum 25(OH)D level are assumed from sun exposure and the
recommendations are fully applicable to people with dark skin
or negligible exposure to sunlight. The Institute found serum 25(OH)D
concentrations above 30 ng/mL (75 nmol/L) are "not consistently
associated with increased benefit". Serum 25(OH)D levels above 50 ng/mL
(125 nmol/L) may be cause for concern. However, some people with serum
25(OH)D between 30 and 50 ng/mL (75 nmol/L-125 nmol/L) will also have
inadequate vitamin D.
Excess
Vitamin D toxicity is rare.
It is caused by supplementing with high doses of vitamin D rather than
sunlight. The threshold for vitamin D toxicity has not been established;
however, according to some research, the tolerable upper intake level
(UL) is 4,000 IU/day for ages 9–71
(100 µg/day), while other research concludes that, in healthy adults,
sustained intake of more than 1250 μg/day (50,000 IU) can produce overt toxicity after several months and can increase serum 25-hydroxyvitamin D levels to 150 ng/mL and greater. Those with certain medical conditions, such as primary hyperparathyroidism, are far more sensitive to vitamin D and develop hypercalcemia
in response to any increase in vitamin D nutrition, while maternal
hypercalcemia during pregnancy may increase fetal sensitivity to effects
of vitamin D and lead to a syndrome of mental retardation and facial
deformities.
A review published in 2015 noted that adverse effects have been reported only at 25(OH)D serum concentrations above 200 nmol/L.
Published cases of toxicity involving hypercalcemia in which the
vitamin D dose and the 25-hydroxy-vitamin D levels are known all involve
an intake of ≥40,000 IU (1,000 μg) per day.
Pregnant or breastfeeding women should consult a doctor before
taking a vitamin D supplement. The FDA advised manufacturers of liquid
vitamin D supplements that droppers accompanying these products should
be clearly and accurately marked for 400 international units
(1 IU is the biological equivalent of 25 ng
cholecalciferol/ergocalciferol). In addition, for products intended for
infants, the FDA recommends the dropper hold no more than 400 IU.
For infants (birth to 12 months), the tolerable upper limit (maximum
amount that can be tolerated without harm) is set at 25 μg/day
(1,000 IU). One thousand micrograms per day in infants has produced
toxicity within one month. After being commissioned by the Canadian and American governments, the Institute of Medicine (IOM) as of 30 November 2010,
has increased the tolerable upper limit (UL) to 2,500 IU per day for
ages 1–3 years, 3,000 IU per day for ages 4–8 years and 4,000 IU per day
for ages 9–71+ years (including pregnant or lactating women).
Calcitriol itself is auto-regulated in a negative feedback cycle, and is also affected by parathyroid hormone, fibroblast growth factor 23, cytokines, calcium, and phosphate.
Effect of excess
Vitamin
D overdose causes hypercalcemia, which is a strong indication of
vitamin D toxicity – this can be noted with an increase in urination and
thirst. If hypercalcemia is not treated, it results in excess deposits
of calcium in soft tissues and organs such as the kidneys, liver, and
heart, resulting in pain and organ damage.
The main symptoms of vitamin D overdose which are those of hypercalcemia including anorexia, nausea, and vomiting. These may be followed by polyuria, polydipsia, weakness, insomnia, nervousness, pruritus and ultimately renal failure. Furthermore, proteinuria, urinary casts, azotemia, and metastatic calcification (especially in the kidneys) may develop.
Other symptoms of vitamin D toxicity include mental retardation in
young children, abnormal bone growth and formation, diarrhea,
irritability, weight loss, and severe depression.
Vitamin D toxicity is treated by discontinuing vitamin D
supplementation and restricting calcium intake. Kidney damage may be
irreversible. Exposure to sunlight for extended periods of time does not
normally cause vitamin D toxicity. The concentrations of vitamin D
precursors produced in the skin reach an equilibrium, and any further vitamin D produced is degraded.
Biosynthesis
Synthesis
of vitamin D in nature is dependent on the presence of UV radiation and
subsequent activation in liver and in kidney. Many animals synthesize
vitamin D3 from 7-dehydrocholesterol, and many fungi synthesize vitamin D2 from ergosterol.
Photochemistry
The photochemistry of vitamin D biosynthesis in animal and fungi
Thermal isomerization of previtamin D3 to vitamin D3
The transformation that converts 7-dehydrocholesterol to vitamin D3 occurs in two steps. First, 7-dehydrocholesterol is photolyzed by ultraviolet light in a 6-electron conrotatory ring-opening electrocyclic reaction; the product is previtamin D3. Second, previtamin D3 spontaneously isomerizes to vitamin D3 (cholecalciferol) in an antarafacial sigmatropic [1,7] hydride shift. At room temperature, the transformation of previtamin D3 to vitamin D3 in an organic solvent takes about 12 days to complete. The conversion of previtamin D3 to vitamin D3 in the skin is about 10 times faster than in an organic solvent.
The conversion from ergosterol to vitamin D2 follows a similar procedure, forming previtamin D2 by photolysis, which isomerizes to vitamin D2. The transformation of previtamin D2 to vitamin D2 in methanol has a rate comparable to that of previtamin D3. The process is faster in white button mushrooms.
Synthesis in the skin
In
the epidermal strata of the skin, vitamin D production is greatest in
the stratum basale (colored red in the illustration) and stratum
spinosum (colored light brown).
Vitamin D3 is produced photochemically from 7-dehydrocholesterol in the skin of most vertebrate animals, including humans. The precursor of vitamin D3, 7-dehydrocholesterol is produced in relatively large quantities. 7-Dehydrocholesterol reacts with UVB light at wavelengths of 290–315 nm. These wavelengths are present in sunlight, as well as in the light emitted by the UV lamps in tanning beds (which produce ultraviolet primarily in the UVA
spectrum, but typically produce 4% to 10% of the total UV emissions as
UVB). Exposure to light through windows is insufficient because glass
almost completely blocks UVB light.
Adequate amounts of vitamin D can be produced with moderate sun
exposure to the face, arms and legs, averaging 5–30 minutes twice per
week, or approximately 25% of the time for minimal sunburn. The darker
the skin, and the weaker the sunlight, the more minutes of exposure are
needed. Vitamin D overdose is impossible from UV exposure; the skin
reaches an equilibrium where the vitamin degrades as fast as it is
created.
Sunscreen absorbs or reflects ultraviolet light and prevents much of it from reaching the skin.
Sunscreen with a sun protection factor (SPF) of 8 based on the UVB
spectrum decreases vitamin D synthetic capacity by 95%, and SPF 15
decreases it by 98%.
The skin consists of two primary layers: the inner layer called the dermis, composed largely of connective tissue, and the outer, thinner epidermis. Thick epidermis in the soles and palms consists of five strata; from outer to inner, they are: the stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, and stratum basale. Vitamin D is produced in the keratinocytes of two innermost strata, the stratum basale and stratum spinosum.
Evolution
Vitamin D can be synthesized only by a photochemical process. Phytoplankton in the ocean (such as coccolithophore and Emiliania huxleyi)
have been photosynthesizing vitamin D for more than 500 million years.
Primitive vertebrates in the ocean could absorb calcium from the ocean
into their skeletons and eat plankton rich in vitamin D.
Land vertebrates required another source of vitamin D other than
plants for their calcified skeletons. They had to either ingest it or be
exposed to sunlight to photosynthesize it in their skin. Land vertebrates have been photosynthesizing vitamin D for more than 350 million years.
In birds and fur-bearing mammals, fur or feathers block UV rays
from reaching the skin. Instead, vitamin D is created from oily
secretions of the skin deposited onto the feathers or fur, and is
obtained orally during grooming. However, some animals, such as the naked mole-rat, are naturally cholecalciferol-deficient, as serum 25-OH vitamin D levels are undetectable.
Industrial synthesis
Vitamin D3 (cholecalciferol) is produced industrially by exposing 7-dehydrocholesterol to UVB light, followed by purification. The 7-dehydrocholesterol is a natural substance in fish organs, especially the liver, or in wool grease (lanolin) from sheep. Vitamin D2 (ergocalciferol) is produced in a similar way using ergosterol from yeast or mushrooms as a starting material.
Mechanism of action
Metabolic activation
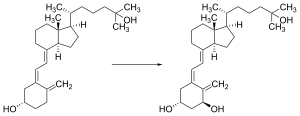
Liver hydroxylation of cholecalciferol to calcifediol
Kidney hydroxylation of calcifediol to calcitriol
Vitamin D is carried in the bloodstream to the liver, where it is converted into the prohormone calcifediol. Circulating calcifediol may then be converted into calcitriol, the biologically active form of vitamin D, in the kidneys.
Whether it is made in the skin or ingested, vitamin D is hydroxylated in the liver at position 25 (upper right of the molecule) to form 25-hydroxycholecalciferol (calcifediol or 25(OH)D). This reaction is catalyzed by the microsomal enzyme vitamin D 25-hydroxylase, the product of the CYP2R1 human gene, and expressed by hepatocytes. Once made, the product is released into the plasma, where it is bound to an α-globulin carrier protein named the vitamin D-binding protein.
Calcifediol is transported to the proximal tubules of the
kidneys, where it is hydroxylated at the 1-α position (lower right of
the molecule) to form calcitriol (1,25-dihydroxycholecalciferol,
1,25(OH)2D). The conversion of calcifediol to calcitriol is catalyzed by the enzyme 25-hydroxyvitamin D3 1-alpha-hydroxylase, which is the product of the CYP27B1 human gene. The activity of CYP27B1 is increased by parathyroid hormone, and also by low calcium or phosphate.
Following the final converting step in the kidney, calcitriol is
released into the circulation. By binding to vitamin D-binding protein,
calcitriol is transported throughout the body, including to the
classical target organs of intestine, kidney and bone. Calcitriol is the most potent natural ligand of the vitamin D receptor, which mediates most of the physiological actions of vitamin D.
In addition to the kidneys, calcitriol is also synthesized by certain other cells including monocyte-macrophages in the immune system. When synthesized by monocyte-macrophages, calcitriol acts locally as a cytokine, modulating body defenses against microbial invaders by stimulating the innate immune system.
Inactivation
The activity of calcifediol and calcitriol can be reduced by hydroxylation at position 24 by vitamin D3 24-hydroxylase, forming secalciferol and calcitetrol, respectively.
Difference between substrates
Vitamin D2 (ergocalciferol) and vitamin D3 (cholecaliferol) share a similar mechanism of action as outlined above. Metabolites produced by vitamin D2 are sometimes named with an er- or ergo prefix to differentiate them from the D3-based counterparts.
- Metabolites produced from vitamin D2 tend to bind less well to the vitamin D-binding protein.
- Vitamin D3 can alternatively be hydroxylated to calcifediol by sterol 27-hydroxylase (CYP27A1), but vitamin D2 cannot.
- Ergocalciferol can be directly hydroxylated at position 24. This hydroxylation also leads to a greater degree of inactivation: while calcitriol's activity decreases to 60% of original after 24-hydroxylation, ercalcitriol suffers a 10-fold decrease in activity on conversion to ercalcitetrol.
History
American researchers Elmer McCollum and Marguerite Davis in 1914 discovered a substance in cod liver oil which later was called "vitamin A". British doctor Edward Mellanby
noticed dogs that were fed cod liver oil did not develop rickets and
concluded vitamin A, or a closely associated factor, could prevent the
disease. In 1922, Elmer McCollum tested modified cod liver oil in which
the vitamin A had been destroyed.
The modified oil cured the sick dogs, so McCollum concluded the factor
in cod liver oil which cured rickets was distinct from vitamin A. He
called it vitamin D because it was the fourth vitamin to be named. It was not initially realized that, unlike other vitamins, vitamin D can be synthesised by humans through exposure to UV light.
In 1925, it was established that when 7-dehydrocholesterol is irradiated with light, a form of a fat-soluble vitamin is produced (now known as D3). Alfred Fabian Hess stated: "Light equals vitamin D." Adolf Windaus, at the University of Göttingen in Germany, received the Nobel Prize in Chemistry in 1928 for his work on the constitution of sterols and their connection with vitamins. In 1929, a group at NIMR
in Hampstead, London, were working on the structure of vitamin D, which
was still unknown, as well as the structure of steroids. A meeting took
place with J.B.S. Haldane, J.D. Bernal, and Dorothy Crowfoot
to discuss possible structures, which contributed to bringing a team
together. X-ray crystallography demonstrated the sterol molecules were
flat, not as proposed by the German team led by Windaus. In 1932, Otto
Rosenheim and Harold King published a paper putting forward structures
for sterols and bile acids which found immediate acceptance. The informal academic collaboration between the team members Robert Benedict Bourdillon, Otto Rosenheim, Harold King, and Kenneth Callow was very productive and led to the isolation and characterization of vitamin D. At this time, the policy of the Medical Research Council
was not to patent discoveries, believing the results of medical
research should be open to everybody. In the 1930s, Windaus clarified
further the chemical structure of vitamin D.
In 1923, American biochemist Harry Steenbock at the University of Wisconsin demonstrated that irradiation by ultraviolet light increased the vitamin D content of foods and other organic materials.
After irradiating rodent food, Steenbock discovered the rodents were
cured of rickets. A vitamin D deficiency is a known cause of rickets.
Using $300 of his own money, Steenbock patented his invention. His
irradiation technique was used for foodstuffs, most memorably for milk.
By the expiration of his patent in 1945, rickets had been all but
eliminated in the US.
In 1969, after studying nuclear fragments of intestinal cells, a specific binding protein for vitamin D called the vitamin D receptor was identified by Mark Haussler and Tony Norman.
In 1971–72, the further metabolism of vitamin D to active forms was
discovered. In the liver, vitamin D was found to be converted to
calcifediol. Calcifediol is then converted by the kidneys to calcitriol,
the biologically active form of vitamin D.
Calcitriol circulates as a hormone in the blood, regulating the
concentration of calcium and phosphate in the bloodstream and promoting
the healthy growth and remodeling of bone. The vitamin D metabolites,
calcifediol and calcitriol, were identified by competing teams led by Michael F. Holick in the laboratory of Hector DeLuca and by Tony Norman and colleagues.
Research
There
is considerable research activity looking at effects of vitamin D and
its metabolites in animal models, cell systems, gene expression studies,
epidemiology and clinical therapeutics. These different types of
studies can produce conflicting evidence as to the benefits of
interventions with vitamin D.
One school of thought contends the human physiology is fine-tuned to an
intake of 4,000–12,000 IU/day from sun exposure with concomitant serum
25-hydroxyvitamin D levels of 40 to 80 ng/mL
and this is required for optimal health. Proponents of this view, who
include some members of the panel that drafted a now-superseded 1997
report on vitamin D from the IOM, contend the IOM's warning about serum
concentrations above 50 ng/mL lacks biological plausibility. They
suggest, for some people, reducing the risk of preventable disease
requires a higher level of vitamin D than that recommended by the IOM.
The United States National Institutes of Health
Office of Dietary Supplements established a Vitamin D Initiative in
2014 to track current research and provide education to consumers.
In their 2016 review, they recognise that a growing body of research
suggests that vitamin D might play some role in the prevention and
treatment of types 1 and 2 diabetes, glucose intolerance, hypertension,
multiple sclerosis, and other medical conditions. They state further:
"however, most evidence for these roles comes from in vitro, animal, and
epidemiological studies, not the randomized clinical trials considered
to be more definitive. Until such trials are conducted, the implications
of the available evidence for public health and patient care will be
debated".
Some preliminary studies link low vitamin D levels with disease later in life. Evidence as of 2013 is insufficient to determine whether vitamin D affects the risk of cancer.
One meta-analysis found a decrease in mortality in elderly people.
Another meta-analysis covering over 350,000 people concluded that
vitamin D supplementation in unselected community-dwelling individuals
does not reduce skeletal (total fracture) or non-skeletal outcomes
(myocardial infarction, ischaemic heart disease, stroke, cerebrovascular
disease, cancer) by more than 15%, and that further research trials
with similar design are unlikely to change these conclusions.
Vitamin D deficiency is widespread in the European population.
European research is assessing vitamin D intake levels in association
with disease rates and policies of dietary recommendations, food
fortification, vitamin D supplementation, and small amounts of sun
exposure.
Apart from VDR activation, various alternative mechanisms of action are under study, such as inhibition of signal transduction by hedgehog, a hormone involved in morphogenesis.