Because Native American populations were not previously exposed
to most diseases introduced by European colonists, populations rarely
had built up individual or population immunities to those diseases. In
addition, Europe's position as a crossroads between many different
peoples, many of whom were separated by hundreds, if not thousands, of
miles (through things like constant war spreading localized afflictions
throughout the continent, and the silk road bringing diseases from the
East), resulted in Europeans being immune to a large variety of
diseases. Therefore, the diseases, which were brought by the Europeans
and had little effect on them, greatly affected, and often continue to
affect, Native Americans. This phenomenon is known as the virgin soil effect.
European contact
An ill Native American in the 19th century, being cared for by a medicine man.
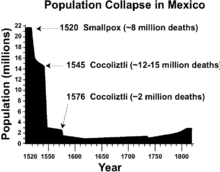
Graph of population decline in central Mexico caused by successive epidemics
The arrival of Europeans also brought on the Columbian Exchange.
During this period European settlers brought many different
technologies and lifestyles with them. Arguably, the most harmful effect
of this exchange was the arrival and spread of disease or biological
warfare; it was the genocide of entire civilizations.
Numerous diseases were brought to North America, including smallpox, bubonic plague, chickenpox, cholera, the common cold, diphtheria, influenza, malaria, measles, scarlet fever, sexually transmitted diseases, typhoid, typhus, tuberculosis, pertussis (whooping cough), etc. Each of these brought destruction through sweeping epidemics, involving disability, illness, and extensive deaths.
Native Americans, due to the lack of prior contact with Europeans, had
not previously been exposed to the diseases that were prevalent on the
distant continent. Therefore, they had not built up internal immunities
to the diseases or formed any medicines to combat them. Europeans came
into the New World bearing various diseases. Those infected with
diseases either possessed them in a dormant state or were not
quarantined in such a way that distanced them enough from Native
Americans not to spread the diseases, allowing them to spread into
epidemics.
The trade of Native American captives, and the use of commercial trade routes continued the spread of disease.
The diseases brought by Europeans are not easily tracked, since there
were numerous outbreaks and all were not equally recorded. Suzanne
Austin Alchon writes that “indirect evidence suggests that some serious
illness may have arrived with the 1500 colonists who accompanied
Columbus's second expedition in 1493. [...] And by the end of 1494,
disease and famine had claimed two-thirds of the Spanish settlers.” The most destructive disease brought by Europeans was smallpox. The first well-documented smallpox epidemic happened in 1518. The Lakota Indians called the disease the running face sickness. Smallpox was lethal to many Native Americans, bringing sweeping epidemics and affecting the same tribes repeatedly.
Between 1837 and 1870, at least four different epidemics struck the Plains tribes.
When the plains Indians began to learn of the "white man’s diseases",
they intentionally avoided contact with them and their trade goods. But
many tribes were enamored with things like metal pots, skillets, and
knives, and they traded with the white newcomers anyway, inadvertently
spreading diseases to their villages.
Certain cultural and biological traits made Native Americans more
susceptible to these diseases. Emphasis placed on visiting the sick led
to the spread of disease through consistent contact.
Native Americans first exposed to these diseases also had a unique
approach to illness, relating primarily to religious beliefs. There is
the belief that disease is caused by either a lack of charm use, an
intrusion of an object by means of sorcery, or the free soul's absence
from the body. Disease was understood to enter the body if one is not
protected by the spirits, as it is a natural occurrence. Religious
powers were believed to be related to curing diseases as well. Native American illness has been treated through the practice of shamanism in the past, though this decreased as the influence of Europeans increased.
Disease evolution and host pathogen interactions should be
considered in Native American disease history. Disease evolution is the
result of the interaction of the following parameters: hosts, parasites,
and setting. Such an example of disease evolution is the direct
biological effects of crowding that directly influences a host's
susceptibility to disease. Research by Power et al. (1998) demonstrated
that, at low doses of micro-bacterial pathogens, hosts were able to make
an appropriate immune response and avoid tuberculosis; higher doses
resulted in a less efficient form of a vaccination. The crowding that
was a result of widespread relocation and concentration of native groups
by the expanding America greatly impacted the susceptibility native
people initially had to the foreign diseases.
Impact on population numbers
Many
Native American tribes experienced great depopulation, averaging 25–50
percent of the tribes' members lost to disease. Additionally, smaller
tribes neared extinction after facing a severely destructive spread of
disease. The significant toll that this took is expounded upon in the article Population history of indigenous peoples of the Americas.
A specific example was Cortes' invasion of Mexico. Before his arrival,
the Mexican population is estimated to have been around 25 to 30
million. Fifty years later, the Mexican population was reduced to 3
million, mainly by infectious disease. This shows the main effect of the
arrival of Europeans in the new world. With no natural immunity against
these pathogens, Native Americans died in huge numbers. Yale historian David Brion Davis
describes this as "the greatest genocide in the history of man. Yet
it's increasingly clear that most of the carnage had nothing to do with
European barbarism. The worst of the suffering was caused not by swords
or guns but by germs." By 1700, less than five thousand Native Americans remained in the southeastern coastal region. In Florida alone, there were seven hundred thousand Native Americans in 1520, but by 1700 the number was around 2000.
In summer 1639, a smallpox epidemic struck the Huron natives in the St. Lawrence and Great Lakes
regions. The disease had reached the Huron tribes through traders
returning from Québec and remained in the region throughout the winter.
When the epidemic was over, the Huron population had been reduced to
roughly 9000 people, about half of what it had been before 1634. The Iroquois people faced similar losses.
Disease did not only have a direct impact on death, but an
indirect impact as well. Losses from disease weakened communities, as
they had fewer people to contribute to their community. There were fewer
people to hunt, plant crops, and otherwise support their society
through other physical means.
Loss of cultural knowledge transfer also impacted the population. By
missing the right time to hunt or plant the crops, the food supply would
be affected, thus weakening the community from not having enough food,
and becoming more vulnerable for the next epidemic.
Communities were also impacted by disease if many of their population
who regularly did the physical tasks of providing food and water
suddenly could not. The communities under such crisis were often unable
to care for the disabled, elderly, or young.
The colonization of the Americas by Europeans killed so much of the indigenous population that it resulted in climate change and global cooling.
Disability
Epidemics killed a large portion of people with disabilities and also created a large number of people with disabilities.
Disabled people in native communities were not considered disabled in
Native American communities as long as they could fulfill their
responsibilities to the community.
The increase in disability due to diseases and epidemics began to
affect Native American communities, as well as displacement,
environmental decline, and war.
While disability affected European settlers, the material and societal
realities of disability for Native American communities was tangible.
Smallpox epidemics led to blindness and depigmented
scars. Smallpox specifically led indirectly to higher rates of suicide.
Many Native American tribes prided themselves in their appearance, and
the resulting skin disfigurement of smallpox deeply affected them
psychologically. Unable to cope with this psychological development,
tribe members were said to have committed suicide. Scarlet fever could result in blindness or deafness, and sometimes both.
Disease as a weapon against Native Americans
"You will do well to try to inoculate the Indians, by means of blankets, as well as to try every other method that can serve to extirpate this execrable race." — Jeffery Amherst
The spread of disease from European contact was not always
accidental. Europeans arriving in the Americas had long been exposed to
the diseases, attaining a measure of immunity, and thus were not as severely affected by them. Therefore, disease could be an effective biological weapon.
During the French and Indian War, Jeffery Amherst, 1st Baron Amherst,
Britain's commander in chief in North America authorized the use of
smallpox to wipe out their Native American enemy. In his writings to
Colonel Henry Bouquet about the situation in western Pennsylvania,
Amherst suggested that the spread of disease would be beneficial in
achieving their aims. Colonel Bouquet confirmed his intentions to do so.
Biological warfare during the Siege of Fort Pitt
"Out of our regard to them we gave them two Blankets and an Handkerchief out of the Small Pox Hospital. I hope it will have the desired effect." William Trent, William Trent's Journal at Fort Pitt
This event is well known for the documented instances of biological warfare.
British officers, including the top British commanding generals,
ordered, sanctioned, paid for and conducted the use of smallpox against
the Native Americans. As described by one historian, "there is no doubt
that British military authorities approved of attempts to spread
smallpox among the enemy", and "it was deliberate British policy to
infect the indians with smallpox".
In this instance, as recorded in his journal by sundries trader and militia Captain William Trent,
on June 24, 1763, allied lords from the Delaware tribe met with Fort
Pitt officials, warned them of "great numbers of Indians" coming to
attack the fort, and threatened them to leave the fort while there was
still time. But the commander of the fort refused to abandon the fort.
Instead, the British gave as gifts two blankets, one silk handkerchief
and one linen from the smallpox hospital,
to two Delaware delegates after the parley, a principal warrior named
Turtleheart, and Maumaultee, a Chief. The tainted gifts were, according
to their inventory accounts, given to the Indian dignitaries "to Convey
the Smallpox to the Indians".
INVOICE for 1763 June
Levy, Trent and Company: Account against the Crown, Aug. 13, 1763"To Sundries got to Replace in kind those which were taken from people in the Hospital to Convey the Smallpox to the Indians Vizt: 2 Blankets @ 20/ £299 099 0
1 Silk Handkerchef 10/
& 1 linnen do: 3/6 099 1399 6
Captain Ecuyer later certified that the items "were had for the uses
above mentioned", in the inventory reimbursement request, and General Thomas Gage would later approve that invoice for payment, endorsing it with a comment and his signature.
While Ecuyer, Trent and McKee were conducting their early form of
biological warfare upon the Indian lords at Fort Pitt, their superiors
were discussing similar plans. General Amherst, having learned that
smallpox had broken out among the garrison at Fort Pitt, and after
learning on July 7 of the loss of his forts at Venango, Le Boeuf and Presqu'Isle,
wrote to Colonel Bouquet, "Could it not be contrived to send the small
pox among the disaffected tribes of Indians? We must on this occasion
use every stratagem in our power to reduce them." In addition, Amherst
wrote, "Captain Ecuyer Seems to Act with great Prudence, & I approve
of everything he mentions to have done." Bouquet, who was already
marching to relieve Fort Pitt and Fort Detroit, responded on the 13th,
"I will try to inoculate the Indians with some blankets that may fall
into their hands, and take care not to get the disease myself. I wish we
could make use of the Spanish method to hunt them with English dogs,
supported by rangers and some light horse, who would, I think,
effectually extirpate or remove that vermin." On July 16, Amherst
replied, "You will do well to try to inoculate the Indians by means of
blankets, as well as to try every other method that can serve to
extirpate this execrable race. I should be very glad your scheme for
hunting them down by dogs could take effect, but England is at too great
a distance to think of that at present."
General Amherst, July 8: "Could it not be contrived to Send the Small Pox among those Disaffected Tribes of Indians? We must, on this occasion, Use Every Stratagem in our power to Reduce them."
Colonel Bouquet, July 13: "I will try to inoculate the Indians by means of Blankets that may fall in their hands, taking care however not to get the disease myself."
Amherst, July 16: "You will Do well to try to Inoculate the Indians by means of Blankets, as well as to try Every other method that can serve to Extirpate this Execrable Race."
Bouquet, July 19: "all your Directions will be observed." Papers of Col. Henry Bouquet, ed. Stevens and Kent, ser. 21634, p. 161.
A
devastating smallpox epidemic plagued Native American tribes in the
Ohio Valley and Great Lakes area through 1763 and 1764, but the
effectiveness of individual instances of biological warfare remains
unknown. After extensive review of surviving documentary evidence,
historian Francis Jennings concluded the attempt at biological warfare was "unquestionably effective at Fort Pitt"; Barbara Mann deduced "it is important to note that the smallpox distribution worked"; Howard Peckham noted the resulting fatal epidemic "certainly affected their vigorous prosecution of the war".
Philip Ranlet notes that there is no evidence that the scheme worked:
there is no information about how fresh the blankets were or how they
were stored, Trent would have likely bragged in his journal if the
scheme had worked, but he is silent as to what happened, and the tribe
had just had a smallpox epidemic, so the blankets would have been fairly
pointless in any case.
Frequency and efficacy of biological weapon usage
There has been some dissent to the accepted history that certain
outbreaks of smallpox were caused by the intentional spreading of
disease, for example when smallpox-infested blankets were intentionally
given to Native Americans in 1763 at the Siege of Fort Pitt. Nineteenth century historian Francis Parkman, the first to research these events, described "the shameful plan of infecting the Indians" as "detestable".
There is persuasive scholarly support that such incidents likely have
occurred more frequently than scholars have acknowledged, but with such
actions considered beyond the pale of civilized behavior, incriminating
documentation would be scarce.
Efforts have since been made to justify the acts of biological
aggression, deny that they happened, minimize the injury or otherwise
reduce the stigma associated with being the perpetrators of such acts.
Captain Ecuyer's official report, written at the time of the incident
and in great detail, notably did not mention the tainted gifts.
According to biological warfare expert Mark Wheelis,
Ecuyer considered concealing the event and acknowledged the deed in his
ledgers only after learning that his superiors were ordering the same
course of action. The most widely cited expert on the subject, Elizabeth Fenn, has observed, "It is also possible that documents relating to such a plan were deliberately destroyed."
Peckham noted that, "oddly enough", the incriminating pages from
Amherst and Bouquet were missing from the Canadian Archives transcripts
as well as the collection published by the Pennsylvania Historical
Commission.
Likewise, Mann has described documents which have gone missing after
"later sanitation", and has documented efforts by "Amherst apologists"
and others who conjecture about, minimize and even dispute the instances
of European perfidy.
One historian says that though blankets containing smallpox were
distributed to Native Americans by the Europeans, they may have been
given with good will and intentions, instead of for the purpose of
disseminating disease, contrary to what was clearly recorded in the
trade ledgers and personal journals. Additionally,
scholars such as Gregory Dowd, are of the opinion that disease was also
spread by Native Americans returning from battling infected Europeans,
and therefore it may also have been spread by Native Americans to their
own people. Dixon has suggested that the attempt to infect the Indians near Fort Pitt "may well have been a failure",
and Ranlet has speculated that "either the smallpox virus was already
dead on the unpleasant gifts or that the presents simply failed to
fulfill Trent's ardent desire to infect the Indians".
Mann has called such assumptions "demonstrably false", and Wheelis has
concluded that while there may have been several simultaneous routes of
transmission for the epidemic, and the effect of each attempt is
impossible to determine, "the act of biological aggression at Fort Pitt
is indisputable".
Colonist accounts of smallpox effects on the native peoples
These
foreign diseases were a constant threat to the native peoples of the
Americas since the late fifteenth century. The attempt to "inoculate"
the native tribes in the area by giving tainted objects to their
dignitaries Turtle's Heart and Mamaltee, is documented in William Trent's journal. Thomas Hutchins, in his August 1762 Journal entry among the Natives at Ohio's Fort Miami, named for the Mineamie people, reports:
The 20th, The above Indians met, and the Ouiatanon Chief spoke in behalf of his and the Kickaupoo Nations as follows: '"Brother, We are very thankful to Sir William Johnson for sending you to enquire into the State of the Indians. We assure you we are Rendered very miserable at Present on Account of a Severe Sickness that has seiz'd almost all our People, many of which have died lately, and many more likely to Die. ... '"The 30th, Set out for the Lower Shawneese Town' and arriv'd 8th of September in the afternoon. I could not have a meeting with the Shawneese untill the 12th, as their People were Sick and Dying every day.
Gershom Hicks, held captive by the Shawnee and Delaware between May
1763 and April 1764, reported to the 42nd Regiment Captain William Grant
"that the Small pox has been very general & raging amongst the
Indians since last spring and that 30 or 40 Mingoes, as many Delawares
and some Shawneese Died all of the Small pox since that time, that it
still continues amongst them".
John McCullough, a Delaware captive since July, 1756, who was then 15 years old, wrote: "Soon after we got home to Mahoning,
instead of taking me to Pittsburgh, agreeable to their promise, they
set out on their Fall hunt, taking me along with them; we staid out till
some time in the Winter before we returned." He continues that, on June
2, 1763,
"Shortly after the commencement of the war, they plundered a tanyard
near to Pittsburgh, and carried away several horse-loads of leather" and recalled that, beginning on July 5, 1763. the Lenape people, under the leadership of Shamokin Daniel, "committed several depredations along the Juniata;
it happened to be at a time when the smallpox was in the settlement
where they were murdering, the consequence was, a number of them got
infected, and some died before they got home, others shortly after;
those who took it after their return, were immediately moved out of the
town, and put under the care of one who had the disease before."
Mary Jemison, a Seneca captive,
was taken in 1755 in what is now Adams County, Pennsylvania. She
married a Delaware, and later chose to remain with the Seneca. In James
E. Seaver's (Jemison's biographer) interview, she described her many
hardships, including travels to Fort Pitt. In 1762, her seventh year of
captivity, she reported the death of her first husband from "sickness".
Contemporary diseases
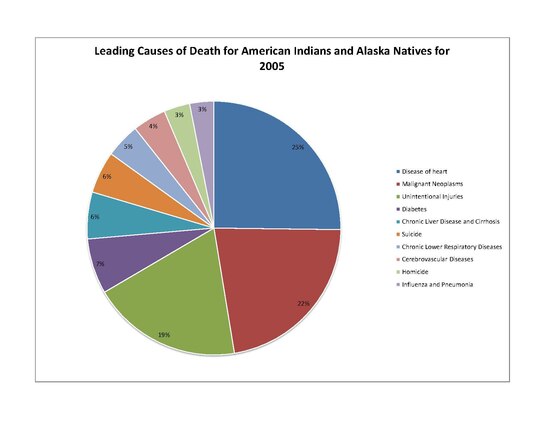
The
leading causes of death by percentage for Native Americans and Alaska
Natives for 2005. Heart disease accounted for 25% of deaths, cancer 22%,
accidents 19%, diabetes 7%, liver disease 6%, suicide 6%, respiratory
diseases 6%, stroke 4%, homicide 3%, and influenza and pneumonia 3%.
Native Americans share many of the same health concerns as their
non-Native American, United States citizen counterparts. For instance,
Native Americans leading causes of death include "heart disease, cancer, unintentional injuries (accidents), diabetes, and stroke". Other health concerns include "high prevalence and risk factors for mental health and suicide, obesity, substance abuse, sudden infant death syndrome (SIDS), teenage pregnancy, liver disease, and hepatitis." The leading causes of death for Native Americans include the following diseases: heart disease, cancer, diabetes, and chronic liver disease / cirrhosis. Overall, Native American life expectancy at birth (as of 2008) is 73.7 years, 4.4 years shorter than the United States average.
Though many of these appear to be concerns paralleling those of
non-Native Americans, some of these diseases present a much greater
threat to Native Americans' well-being.
American Indians and Alaska Natives die at greater rates from: chronic
liver disease and cirrhosis, diabetes mellitus, unintentional injuries,
assault/homicide, intentional self-harm/suicide, and chronic lower
respiratory diseases. These discrepancies in disease patterns vary significantly between diseases, but have a significant impact on the population.
The genetic composition of Native Americans and clans can have an influence on many diseases and their continuing presence.
The commonly lower socioeconomic status limits the ability of many to
receive adequate health care and make use of preventative measures.
Also, certain behaviors that take place commonly in the Native American
culture can increase risk of disease.
When the period of tribal termination in the 20th century occurred,
post termination many tribes could no longer afford to keep their
hospitals open.
Native Americans have higher rates of tobacco use than white,
Asian, or black communities. Native American men are about as likely to
be moderate to heavy drinkers as white men, but about 5–15% more likely
to be moderate to heavy drinkers than black or Asian men. Native
Americans are 10% less likely to be at a healthy weight than white
adults, and 30% less likely to be at a healthy weight than Asian adults.
On a similar note, they have far greater rates of obesity, and were
also less likely to engage in regular physical activity than white
adults.
Data collected by means of secondary sources such as the US
Census Bureau and the Centers for Disease Control and Prevention's
National Center for Health Statistics showed that from 1999 to 2009
Alaska Natives and Native Americans had high mortality rates to
infectious diseases when compared to the mortality rate of white
Americans. Alaska natives from the age groups 0–19 and 20–49 had death
rates 4 to 5 times higher than compared to whites. Native Americans from
the 20–49 age group in the Northern Plains were also 4 to 5 times more
likely to die to infectious diseases than whites. Also found was that
Native American and Alaska Natives were 13 times more likely to contract
tuberculosis than whites.
Native Americans were at least twice as likely to have unmet
medical needs due to cost and were much less likely to have seen a
dentist within the last five years compared with white or Asian adults,
putting them at risk for gingivitis and other oral diseases. As it
stands, Native American/ Alaska Natives face high rates of health
disparity compared to other ethnic groups.
Heart disease
The leading cause of death of Native Americans is heart disease.
In 2005, it claimed 2,659 Native American lives. Heart disease occurs
in Native American populations at a rate 20 percent greater than all
other United States races. Additionally, the demographic of Native
Americans who die from heart disease is younger than other United States
races, with 36% dying of heart disease before age 65. The highest heart disease death rates are located primarily in South Dakota and North Dakota, Wisconsin, and Michigan.
Heart disease in Native Americans is not only due to diabetic complications; the increased risk is also due to higher rates of hypertension.
Native American populations have been documented as being more likely
to have high blood pressure than other groups, such as white Caucasians. Studies have also been conducted that associate the exposure to stress and trauma
to an increased rate of heart disease. It has been documented in Native
American populations that adverse childhood experiences, which are
significantly more common in the Native American demographic, have a
positively linear relationship with heart disease, as well an increasing
influence on symptoms of heart disease.
Cancer
Cancer
has a documented presence among Native Americans, and the rates of
certain types of cancer exceed that of the general population of the
United States. For instance, Native American males were twice as likely
to have liver cancer
than white males in 2001–05. Women are 2.4 times as likely to contract
and die from liver cancer as their white counterparts. Rates of
alcoholism of Native Americans are also greater than in the general
population.
Stomach cancer
was also 1.8 times more common in Native American males than white
males, in addition to being twice as likely to be fatal. Other cancers,
such as kidney cancer,
are more common among Native American populations. It is important to
note that overall cancer rates are lower among Native Americans compared
to the white population of the United States. For cancers that are more
prevalent in Native Americans than the white United States population,
death rates are higher.
Diabetes
The rates of death by diabetes for each race and ethnicity in the United States in 2005
Diabetes has posed a significant health risk to Native Americans. Type I diabetes is rare among Native Americans. Type II diabetes
is a much more significant problem and is the type of diabetes referred
to in the remainder of this section. The prevalence of diabetes began
primarily in the middle of the twentieth century and has grown into an
epidemic. This time frame coincides with the fact that Indians were now
living on reservations. With the uprooting of Indians and their
traditional way of life, and being put onto reservations, this removed
not only their main source of exercise with hunting and gathering, but
also the healthier food that they were used to eating. About 16.3% of Native American adults have been diagnosed with diabetes.
Type two diabetes and the complications that follow have gone from
being acute infectious diseases to chronic illnesses within Native
American and Alaska Native communities. Native Americans and Alaska
Natives experience high rates of end-stage renal disease, which is
mainly driven by, and directly correlates with, the increase in diabetes
within their communities.
Native Americans are about 2.8 times more likely to have Type II
diabetes than white individuals of comparable age. The rates of diabetes
among Native Americans also continue to rise. During the eight-year
span of 1990 to 1998, diabetes grew 65% among the Native American
population. This is very significant growth, and this growth continues
in the present day.
The highest rates of diabetes in the world are also found among a Native American tribe. The Pima
tribe of Arizona took part in a research study on diabetes which
documented diabetes rates within the tribe. This study found that the
Pimas had diabetes rates 13 times that of population of Rochester,
Minnesota, a primarily white populace. Diabetes was documented in over
one third of Pimas from ages 35–44, and in over sixty percent of those
over 45 years of age.
There are multiple causes for diabetes to cast such a presence on the Native American demographic:
- Genetic predisposition
- Native Americans with the "least genetic admixture with other groups" have been found to be at a higher risk of developing diabetes. the genetic makeup of the American Indian allowed their bodies to store energy for use in times of famine. When food was plentiful, their bodies would store excess carbs through an exaggerated secretion of insulin called hypersulinemia, and be able to use this stored energy when food was scarce. When feast or famine was no longer an issue, and food was always plentiful, with modern, high caloric foods, their bodies may not have been able to handle the excess fat and calories, resulting in type II diabetes.
- Obesity
- Native Americans have a significant health problem with obesity, as they are 1.6 times more likely to be obese than a white American.; Native Americans are as likely as black adults to be obese. Obesity is known as a general causative factor of diabetes, which is generally caused by Food Deserts, a lack of readily available nutritious foods, in reservations.
- Low birth weight
- The correlation between low birth weight and increased risk of diabetes has been documented in Native American populations
- Diet
- Changes in Native American diets have been associated with the increase in diabetes, as more high calorie and high fat foods are consumed, replacing the traditionally agriculturally driven diet. As time has gone there has been a push for Native Americans to return to their traditional ways; including growing and eating traditional foods. The Centers for Disease Control and Prevention (CDC) has been a huge proponent of Native Americans returning to traditional diets. Even going as far as too make a PSA in 2013, which involved Cherokee actors discussing diabetes, and the impact diet has on their increased risk. In the past several years agencies such as the IHS (part of the U.S. Public Health Svc.) & the Division of Diabetes Treatment and Prevention (DDTP) have offered up 19 diabetes programs, 12 control officers, and 399 grant programs such as SDPI (Special Diabetes program for Indians), aimed at educating and helping Native Americans to hopefully one day abolish diabetes for good.
Mental health
Other
issues that Native Americans are facing are mental health and suicide.
Native Americans have the highest rate of suicide out of any ethnic
group in the United States, in 2009 suicide was the leading cause of
death among Native Americans and Native Alaskans between the ages of 10
and 34.
75% of deaths among Native Americans and Native Alaskans over the age
of 10 are due to unintentional injury, homicide, and suicide. Suicide rates among Native American youths is significantly higher than the suicide rates among white youths. The head of the IHS, Mary L. Smith, says
that there will be a new focus on mental health issues in Native
American communities, and that since there is a tremendous amount of
suicide among teens on the Pine Ridge reservation they are designating
it a Promise Zone and sending extra help.
Impact
The significant presence of diabetes also brings other health complications, such as end-stage renal disease. Each of these are more prevalent in the Native American population.
Diabetes has caused premature death of Native Americans by vascular
disease, especially in those diagnosed with diabetes later in life. It
has been reported among the Pima Tribe to cause elevated urinary albumin
excretion. Native Americans with diabetes have a significantly higher
rate of heart disease than those without diabetes, and cardiovascular
disease is the "leading underlying cause of death in diabetic adults" in
Native Americans.
Diabetes has caused nephropathy
among Native Americans, leading to renal function deterioration,
failure, and disease. Prior to the increase in cardiovascular disease
among diabetic Native Americans, renal disease was the leading cause of
death. Another complication documented in diabetic Native Americans, as
well as other diabetic populations, is retinopathy.
Lower extremity amputations are also higher among Native American
populations with diabetes. In studies of the Pima tribes, those with
diabetes were found to have much higher prevalence of periodontal
disease. Additionally, those with diabetes have higher instances of
bacterial and fungal infection. This is seen in statistics such as
"diabetic Sioux (Lakota people) Tribes were four times as likely to have tuberculosis as those without diabetes."
Prior to the 1940s diabetes was virtually unheard of, but ever
since the 1960s the prevalence has been on the rise. This rise is
thought to be in part due to their food history and culture. Native
Americans had a diverse food history prior to colonization, but after
colonization the natives were forced to live on non-traditional lands
and eat government hand-outs for food. Much of this food was of low
quality, meaning that here is not much nutritional content for the
caloric intake and led to many Natives being malnourished.
Native Americans with diabetes have a death rate three times
higher than those in the non-Native population. Diabetes can shorten a
person's life by approximately 15 years.
As of 2012, diabetes was not the leading cause of death for Native
Americans itself but contributed significantly to the top leading causes
of death.
The barriers for Native Americans and Alaskan Natives to receive
proper health care include the isolated locations of some tribes make
traveling to facilities far too difficult to travel the distance,
hazardous roads, high rates of poverty, and too few staff in hospitals
near reservations. Another contributing factor is that Native people
generally wait longer for organ transplants than white people. Diabetes
is primary cause of end-stage renal disease, and dialysis treatments and
kidney transplants remain the most effective methods of treatment
Alcoholism
Another significant concern in Native American health is alcoholism.
Alcoholism in the modern day is approached as a disease, and has been
strongly linked to genetics and social circumstances. The rate of death
from alcoholism in Native Americans is about five times that of all
races in the United States.
However, due to the nature of alcoholism and the behaviors involved,
the disease model is not always applicable. It is clearly a disorder
that has many factors, but the behavioral component distinguishes it
from many other diseases, such as those previously discussed. Alcoholism, along with drug use, is discussed in Modern social statistics of Native Americans.
However, In contrast to enduring and often racist stories about
extraordinarily high rates of alcohol abuse among Native Americans, University of Arizona researchers have found
that Native Americans’ binge and heavy drinking rates actually match
those of whites. The groups differed regarding abstinence: Native
Americans were more likely to abstain from alcohol use.
The “Drunken Indian” myth perpetuates a stereotype that affects
everything from the kind of jobs a native person gets, to the kind of
diagnosis that a doctor gives a native person.
From the National Survey on Drug Use and Health (spanning from
2009 to 2013 which included data from more than 4,000 Native Americans
and 170,000 whites), and The Behavioral Risk Factor Surveillance System
survey (conducted between 2011 and 2013, covered more than 21,000 Native
Americans and 1 million whites) about 17 percent of whites and Native
Americans were binge drinkers. When asked about the last time they had a
drink, 40% percent of Native Americans had a drink during the previous
month, compared to 43 percent of whites who did consume alcohol in the
previous month. Despite only drinking marginally less than white people,
Native Americans may be more vulnerable to the risks associated with
drinking because of other issues, such as a lack of access to health
care, safe housing and clean water
HIV/AIDS
HIV and AIDS
are growing concerns for the Native American population. The overall
percentage of Native Americans diagnosed with either HIV or AIDS within
the entire United States population is relatively small. Native American
AIDS cases make up approximately 0.5% of the nation's cases, while they
account for about 1.5% of the total population.
Native Americans and Alaska Natives rank third in the United States in the rate of new HIV infections.
Native Americans, when counted with Alaskan Natives, have a 40% higher
rate of AIDS than white individuals. Also, Native American and Alaskan
Native women have double the rate of AIDS of white women.
These statistics have multiple suggested causes:
- Sexual behaviors
- Previous studies of high rates of sexually transmitted diseases among Native Americans lead to the conclusion that the sexual tendencies of Native Americans lead to greater transmission
- Illicit drug use
- The use of illicit drugs is documented to be very high among Native Americans, and not only does the involvement of individuals with illicit drugs correlate with greater rates of sexually transmitted disease, but it can facilitate the spread of diseases
- Socio-economic status
- Due to the poverty and lower rates of education, the risk of getting AIDS or any other sexually transmitted disease can be increased indirectly or directly
- Testing and data collection
- Native Americans may have limited access to testing for HIV/AIDS due to location away from certain health facilities; data collected on Native American sexually transmitted diseases may be limited for this same reason as well as for under-reporting and the Native American race being misclassified
- Culture and tradition
- Native American culture is not always welcoming of open discussion of sexually transmitted diseases
Stroke
Stroke
is the sixth-leading cause of death in the Native American population.
Native Americans are sixty percent more likely than white adults in the
United States to have a stroke. Native American women have double the
rate of stroke of white women. About 3.6% of Native American and Alaska
Native men and women over 18 have a stroke. The stroke death rate of Native Americans and Alaska Natives is 14 percent greater than among all races.
Combating disease and epidemics
Many
initiatives have been put in place to combat Native American disease
and improve the overall health of this demographic. One primary example
of such initiative by the government is the Indian Health Service
which works "to assure that comprehensive, culturally acceptable
personal and public health services are available and accessible to
Native American and Alaska Native people".
There are many other governmental divisions and funding for health care
programs relating to Native American diseases, as well as a multitude
of programs administered by tribes themselves.
Legislature
Healthcare for Native Americans were provided through the Department of War (throughout the 1800s) until it became a focus of the Office of Indian Affairs in the late 1800s. It again switched government agencies in the early 1950s, going under the supervision of the Department of Health, Education, and Welfare's Public Health Service (PHS). In 1955, the Indian Health Service division was created, which still enacts the majority of Native American specific healthcare.
The Snyder Act of 1921 (23 U.S.C. 13) was one of the first formal legislative pieces to allow healthcare to be provided to Native Americans.
In the 1970s, more legislature began passing to expand the healthcare access for Native Americans.
Diabetes programs
Eagle
books are a book series produced by the CDC to inform Native American
children about healthy lifestyles to prevent diabetes.
As diabetes is one of the utmost concerns of the Native American
population, many programs have been initiated to combat this disease.
Governmental programs
One such initiative has been developed by the Centers for Disease Control and Prevention
(CDC). Termed the "Native Diabetes Wellness Program", this program
began in 2004 with the vision of an "Indian Country free of the
devastation of diabetes".
To realize this vision, the program works with Native American
communities, governmental health institutions, other divisions of the
CDC, and additional outside partners. Together they develop health
programs and community efforts to combat health inequalities and in turn
prevent diabetes. The four main goals of the Native Diabetes Wellness
Program are to promote general health in Native communities (physical
activity, traditional foods), spread narratives of traditional health
and survival in all aspects of life, utilize and evaluate health
programs and education, and promote productive interaction with the
state and federal governments.
Funding for these efforts is provided by the Balanced Budget Act
of 1997, Public Law 105-33, and the Indian Health Service. One
successful aim of this program is the Eagle Books series, which are
books using animals as characters to depict a healthy lifestyle that
prevents diabetes, including embracing physical activity and healthy
food. These books were written by Georgia Perez, who worked with the
University of New Mexico's Native American Diabetes Project.
Other successful efforts include Diabetes Talking Circles to address
diabetes and share a healthy living message and education in schools.
The Native Diabetes Wellness Program also has worked with tribes to
establish food programs that support the "use of traditional foods and
sustainable ecological approaches" to prevent diabetes.
The Indian Health Service
has also worked to control the diabetes prevalence among Native
Americans. The IHS National Diabetes Program was created in 1979 to
combat the escalating diabetes epidemic.
The current head of the IHS, Mary L. Smith, Cherokee, took the position
in March 2016 and had pledged to improve the IHS and focus on
comprehensive health care for all the tribes and people covered by the
department.
A sector of the service is the Division of Diabetes Treatment and
Prevention, which "is responsible for developing, documenting, and
sustaining clinical and public health efforts to treat and prevent
diabetes in Native Americans and Alaska Natives".
This division contains the Special Diabetes Program for Indians,
as created by 1997 Congressional legislation. This program receives
$150 million a year in order to work on "Community-Directed Diabetes
Programs, Demonstration Projects, and strengthening the diabetes data
infrastructure".
The Community-Directed Diabetes Programs are programs designed
specifically for Native American community needs to intervene in order
to prevent and treat diabetes. Demonstration Projects "use the latest
scientific findings and demonstrate new approaches to address diabetes
prevention and cardiovascular risk reduction".
Strengthening the diabetes data infrastructure is an effort to attain a
greater base of health information, specifically for the IHS electronic health record.
In addition to the Special Diabetes Program for Native Americans,
the IHS combats diabetes with Model Diabetes Programs and the
Integrated Diabetes Education Recognition Program. There are 19 Model
Diabetes Programs which work to "develop effective approaches to
diabetes care, provide diabetes education, and translate and develop new
approaches to diabetes control".
The Integrated Diabetes Education Recognition Program is an IHS program
that works towards high-quality diabetes education programs by
utilizing a three-staged accreditation scale. Native American programs
in healthcare facilities can receive accreditation and guidance to
effectively educate the community concerning diabetes self-management.
Tribal programs
Many
tribes themselves have begun programs to address the diabetes epidemic,
which can be specifically designed to address the concerns of the
specific tribe. The Te-Moak Tribe of Western Shoshone
have created their diabetes program. With this program, they hope to
promote healthy lifestyles with exercise and modified eating and
behavior. The means of achieving these ends including "a Walking Club, 5
a Day Fruits and Vegetable, Nutrition teaching, Exercise focusing, 28
day to Diabetes Control, and Children's Cookbook".
Additionally, the Te-Moak tribe has constructed facilities to promote
healthy lifestyles, such as a center to house the diabetes program and a
park with a playground to promote active living.
The Meskwaki
Tribe of the Mississippi has also formed diabetes program to provide
for the tribe's people. The Meskwaki Tribe facilitates their program to
eliminate diabetes as a health concern through prevention and control of
complications. The program has a team mentality, as community,
education and clinical services are all involved as well as community
organizations and members.
There are many facets of this diabetes program, which include the
distribution of diabetes information. This is achieved through
bi-weekly articles in the Meskwaki Times educating the population about
diabetes prevention and happenings in the program and additional
educational materials available about diabetes topics. Other educational
is spread through nutrition and diabetes classes, such as the Diabetes
Prevention Intensive Lifestyle Curriculum Classes, and events like
health fairs and walks. Medical care is also available. This includes
bi-weekly diabetes clinics, screenings for diabetes and related health
concerns and basic supplied.
HIV-AIDS programs
Official seal of the National Native HIV/AIDS Awareness Day
Multiple programs exist to address the HIV and AIDS concerns for
Native Americans. Within the Indian Health Service, an HIV/AIDS
Principal Consultant heads an HIV/AIDS program. This program involves
many different areas to address "treatment, prevention, policy,
advocacy, monitoring, evaluation, and research".
They work through many social outputs to prevent the masses from the
epidemic and enlist the help of many facilities to spread this message.
The Indian Health Service also works with Minority AIDS
Initiative to use funding to establish AIDS projects. This funding has
been used to create testing, chronic care, and quality care initiatives
as well as training and camps.
The Minority AIDS Initiative operates through the Ryan White HIV/AIDS
Program, under the Public Health Service Act. This is in recognition of
the disproportionate impact of HIV/AIDS on racial and ethnic minorities.
There has also been a National Native HIV/AIDS Awareness Day held
on March 20 for Native Americans, Alaska Natives, and Native Hawaiians,
with 2009 marking its third year. This day is held to:
- encourage Native people to get educated and to learn more about HIV/AIDS and its impact in their community;
- work together to encourage testing options and HIV counseling in Native communities; and
- help decrease the stigma associated with HIV/AIDS.
This day takes place across the United States with many groups
working in coordination, groups like the CDC and the National Native
Capacity Building Assistance Network. By putting out press releases,
displaying posters, and holding community events, these groups hope to
raise awareness of the HIV/AIDS epidemic.
Heart disease and stroke programs
The
United States CDC contains a Division for Heart Disease and Stroke
Prevention, and collects data and specifically releases information to
form policy for Native Americans. They have identified many areas in
which lifestyles of Native Americans need to be changed in order to
greatly decrease the prevalence of heart disease and stroke.
One major concern to prevent is diabetes, which directly relates to the
presence of heart disease. Many general health concerns also need to be
addressed, according to the CDC's observations, including moderating
alcohol use, eliminating tobacco use, maintaining health body weight,
regularizing physical activity, diet, and nutrition, preventing and
controlling high blood cholesterol, and preventing and controlling high
blood pressure.
The Indian Health Service works in collaboration with the
University of Arizona College of Medicine to maintain the Native
American Cardiology Program. This is a program that acknowledges the
changes in lifestyle and economics in the recent past which have
ultimately increased the prevalence of heart attacks, coronary disease,
and cardiac deaths. The Native American Cardiology Program prides itself
in its cultural understanding, which allows it to tailor health care
for its patients.
The program has many bases but has placed an emphasis on
providing care to remote, rural areas in order for more people to be
cared for. The Native American Cardiology Program's telemedicine
component allows for health care to be made more accessible to Native
Americans. This includes interpreting medical tests, offering specialist
input and providing triage over the phone. The Native American
Cardiology Program also has educational programs, such as lectures on
cardiovascular disease and its impact, and outreach programs.