A child receives oral polio vaccine during a 2002 campaign to immunize children in India.
A public health effort to permanently eliminate all cases of poliomyelitis (polio) infection around the world began in 1988, led by the World Health Organization (WHO), the United Nations Children's Fund (UNICEF) and the Rotary Foundation. These organizations, along with the U.S. Centers for Disease Control and Prevention (CDC) and The Gates Foundation, have spearheaded the campaign through the Global Polio Eradication Initiative
(GPEI), which helps to coordinate vaccination campaigns, environmental
monitoring, evaluation of possible polio cases and logistics. Successful eradication of infectious diseases has been achieved twice before, with smallpox and bovine rinderpest.
Prevention of disease spread is accomplished by vaccination. There are two kinds of polio vaccine—oral polio vaccine (OPV), which uses weakened poliovirus, and inactivated
polio vaccine (IPV), which is injected. The OPV is less expensive and
easier to administer, and can spread immunity beyond the person
vaccinated, creating contact immunity.
It has been the predominant vaccine used. However, under conditions of
long-term vaccine virus circulation in under-vaccinated populations,
mutations can reactivate the virus to produce a polio-inducing strain,
while the OPV can also, in rare circumstances, induce polio or
persistent asymptomatic infection in vaccinated individuals,
particularly those that are immunodeficient. Being inactivated, the IPV
is free of these risks but does not induce contact immunity. IPV is more
costly and the logistics of delivery are more challenging.
The 33 diagnosed wild polio virus (WPV) cases worldwide in 2018 represented a 95% reduction from the 719 diagnosed cases in 2000 and a 99.99%
reduction from the estimated 350,000 cases when the eradication effort
began in 1988. Of the three strains of polio virus, the last recorded
wild case caused by type 2 (WPV2) was in 1999, and WPV2 was declared
eradicated in 2015. Type 3 (WPV3) is last known to have caused polio on
11 November 2012, with all wild-virus cases since that date being due to
type 1 (WPV1). All three types are represented among the periodic
cases arising from mutated oral vaccine strains, so-called circulating
vaccine-derived poliovirus (cVDPV). India is the latest country to have officially stopped endemic transmission of polio, with its last reported case in 2011. Three countries remain where the disease is endemic—Afghanistan, Pakistan and Nigeria.
Factors influencing eradication of polio
Eradication
of polio has been defined in various ways—as elimination of the
occurrence of poliomyelitis even in the absence of human intervention, as extinction of poliovirus, such that the infectious agent no longer exists in nature or in the laboratory, as control of an infection to the point at which transmission of the disease ceased within a specified area,
and as reduction of the worldwide incidence of poliomyelitis to zero as
a result of deliberate efforts, and requiring no further control
measures.
In theory, if the right tools were available, it would be
possible to eradicate all infectious diseases that reside only in a
human host. In reality there are distinct biological features of the
organisms and technical factors of dealing with them that make their
potential eradicability more or less likely. Three indicators, however,
are considered of primary importance in determining the likelihood of
successful eradication: that effective interventional tools are
available to interrupt transmission of the agent, such as a vaccine; that diagnostic tools, with sufficient sensitivity and specificity,
be available to detect infections that can lead to transmission of the
disease; and that humans are required for the life-cycle of the agent,
which has no other vertebrate reservoir and cannot amplify in the environment.
Strategy
The most important step in eradication of polio is interruption of endemic transmission of poliovirus. Stopping polio transmission has been pursued through a combination of routine immunization,
supplementary immunization campaigns and surveillance of possible
outbreaks. Several key strategies have been outlined for stopping polio
transmission:
- High infant immunization coverage with four doses of oral polio vaccine (OPV) in the first year of life in developing and endemic countries, and routine immunization with OPV and/or IPV elsewhere.
- Organization of "national immunization days" to provide supplementary doses of oral polio vaccine to all children less than five years old.
- Active surveillance for poliovirus through reporting and laboratory testing of all cases of acute flaccid paralysis. Acute flaccid paralysis (AFP) is a clinical manifestation of poliomyelitis characterized by weakness or paralysis and reduced muscle tone without other obvious cause (e.g., trauma) among children less than fifteen years old. AFP is also associated with a number of other pathogenic agents including enteroviruses, echoviruses, and adenoviruses, among others.
- Expanded environmental surveillance to detect the presence of poliovirus in communities. Sewage samples are collected at regular and random sites and tested in laboratories for the presence of WPV or cVDPV. Since most polio infections are asymptomatic, transmission can occur in spite of the absence of polio-related AFP cases, and such monitoring helps to evaluate the degree to which virus continues to circulate in an area.
- Targeted "mop-up" campaigns once poliovirus transmission is limited to a specific focal area.
Vaccination
There are two distinct polio vaccines. The oral polio vaccine (OPV, or Sabin vaccine) contains an attenuated poliovirus, 10,000 times less able to enter the circulation and cause polio, delivered as oral drops or infused into sugar cubes. It is highly effective and inexpensive (about US$0.12 per dose in 2016) and its availability has bolstered efforts to eradicate polio. A study carried out in an isolated Eskimo village showed that antibodies produced from subclinical wild virus infection persisted for at least 40 years. Because the immune response
to oral polio vaccine is very similar to natural polio infection, it is
expected that oral polio vaccination provides similar lifelong immunity to the virus.
Due to its route of administration, it induces an immunization of the
intestinal mucosa that protects against subsequent infection, though
multiple doses are necessary to achieve effective prophylaxis. It can also produce contact immunity. Attenuated
poliovirus derived from the oral polio vaccine is excreted, and infects
and indirectly induces immunity in unvaccinated individuals, thus
amplifying the effects of the doses delivered.
The oral administration does not require special medical equipment or
training. Taken together, these advantages have made it the preferred
vaccine of many countries, and it has long been preferred by the global
eradication initiative.
The primary disadvantage of the OPV derives from its inherent
nature as an attenuated but active virus. It can induce
vaccine-associated paralytic poliomyelitis (VAPP) in approximately 1
individual per every 2.4 million doses administered.
Likewise, mutation during the course of persistent circulation in
undervaccinated populations can lead to vaccine-derived poliovirus
strains (cVDPV) that can induce polio at much higher rates.
Until recently, a trivalent OPV containing all three virus strains was
used, but with the eradication of wild poliovirus type 2 this was
phased out in 2016 and replaced with bivalent vaccine containing just
types 1 and 3, while use of monovalent type 2 OPV is restricted to
regions with documented cVDPV2 circulation.
The inactivated polio vaccine (IPV, or Salk)
contains trivalent fully inactivated virus, administered by injection.
This vaccine cannot induce VAPP nor do cVDPV strains arise from it, but
it likewise cannot induce contact immunity and thus must be
administered to every individual. Added to this are greater logistical
challenges. Though a single dose is sufficient for protection,
administration requires medically trained vaccinators armed with
single-use needles and syringes. Taken together, these factors result
in substantially higher delivery costs. Original protocols involved intramuscular injection in the arm or leg, but recently subcutaneous injection
using a lower dose (so-called fractional-dose IPV, fIPV) has been found
to be effective, lowering costs and also allowing for more convenient
and cost-effective delivery systems.
The use of IPV results in serum immunity, but no intestinal immunity
arises. As a consequence, a vaccinated individual is protected from
contracting polio, but their intestinal mucosa can still be infected and
serve as a reservoir for the excretion of live virus. For this reason,
IPV is ineffective at halting ongoing outbreaks of WPV or cVDPV, but it
has become the vaccine for choice for industrialized, polio-free
countries.
While IPV does not itself induce mucosal immunity, it has been shown to boost the mucosal immunity from OPV,
and WHO now favors a combined protocol. It is recommended that
vulnerable children receive a dose of OPV at birth, then beginning at
the age of 6 weeks a 'primary series' consisting of three OPV doses at
least four weeks apart, along with one dose of IPV after 14 weeks. This combined IPV/OPV approach has also been used in outbreak suppression.
Herd immunity
Polio vaccination is also important in the development of herd immunity. For polio to occur in a population, there needs to be an infecting organism (poliovirus), a susceptible human population, and a cycle of transmission.
Poliovirus is transmitted only through person-to-person contact and the
transmission cycle of polio is from one infected person to another
person susceptible to the disease, and so on. If the vast majority of the population is immune to a particular agent, the ability of that pathogen
to infect another host is reduced; the cycle of transmission is
interrupted, and the pathogen cannot reproduce and dies out. This
concept, called community immunity or herd immunity, is important to
disease eradication, because it means that it is not necessary to
inoculate 100% of the population—a goal that is often logistically very
difficult—to achieve the desired result. If the number of susceptible
individuals can be reduced to a sufficiently small number through vaccination, then the pathogen will eventually die off.
When many hosts are vaccinated, especially simultaneously, the
transmission of wild virus is blocked, and the virus is unable to find
another susceptible individual to infect. Because poliovirus can only
survive for a short time in the environment (a few weeks at room
temperature, and a few months at 0–8 °C (32–46 °F)), without a human
host the virus dies out.
Herd immunity is an important supplement to vaccination. Among
those individuals who receive oral polio vaccine, only 95 percent will
develop immunity.
That means five of every 100 given the vaccine will not develop any
immunity and will be susceptible to developing polio. According to the
concepts of herd immunity this population whom the vaccine fails, are
still protected by the immunity of those around them. Herd immunity can
only be achieved when vaccination levels are high.
It is estimated that 80–86 percent of individuals in a population must
be immune to polio for the susceptible individuals to be protected by
herd immunity.
If routine immunization were stopped, the number of unvaccinated,
susceptible individuals would soon exceed the capability of herd
immunity to protect them.
Vaccine-derived poliovirus
While vaccination has played an instrumental role in the reduction of
polio cases worldwide, the use of attenuated virus in the oral vaccine
carries with it an inherent risk. The oral vaccine is a powerful tool
in fighting polio in part because of its person-to-person transmission
and resulting contact immunity. However, under conditions of long-term
circulation in under-vaccinated populations, the virus can accumulate
mutations that reverse the attenuation and result in vaccine virus
strains that themselves cause polio. As a result of such circulating
vaccine-derived poliovirus (cVDPV) strains, polio outbreaks have
periodically recurred in regions that have long been free of the wild
virus, but where vaccination rates have fallen. Oral vaccines can also
give rise to persistent infection in immunodeficient individuals, with
the virus eventually mutating into a more virulent
immunodeficiency-associated vaccine-derived poliovirus (iVDPV). In
particular the type 2 strain seems prone to reversions, so in 2016 the
eradication effort abandoned the trivalent oral vaccine containing
attenuated strains of all three virus types, and replaced it with a
bivalent oral vaccine lacking the type 2 virus. Eradication efforts
will eventually require all oral vaccination to be discontinued in favor
of the use of injectable vaccines. These vaccines are more expensive
and harder to deliver, and they lack the ability to induce contact
immunity because they contain only killed virus, but they likewise are
incapable of giving rise to vaccine-derived viral strains.
Surveillance
A
global program of surveillance for the presence of polio and the
poliovirus plays a critical role in assessment of eradication and in
outbreak detection and response. Two distinct methods are used in
tandem: Acute Flaccid Paralysis (AFP) surveillance and environmental
surveillance.
Monitoring for AFP aims at identifying outbreaks of polio by
screening patients displaying symptoms consistent with but not exclusive
to severe poliovirus infection. Stool samples are collected from
children presenting with AFP and evaluated for the presence of
poliovirus by accredited laboratories in the Global Polio Laboratory
Network. Since rates of non-polio AFP are expected to be constant and
large compared to polio cases, the frequency of non-polio AFP reported
in a population is indicative of the effectiveness of surveillance, as
is the proportion of AFP patients from whom high-quality stool samples
are collected and tested, with a target of at least 80%.
Environmental surveillance is used to supplement AFP
surveillance. This entails the routine testing of sewage samples for the
presence of virus. This not only allows the effectiveness of
vaccination efforts to be evaluated in countries with active
transmission, but also allows the detection of new outbreaks in
countries without known transmission. The GPEI currently conducts
environmental surveillance in 44 countries, 24 of which are in Africa.
Obstacles
Among
the greatest obstacles to global polio eradication are the lack of
basic health infrastructure, which limits vaccine distribution and
delivery, the crippling effects of civil war and internal strife, and
the sometimes oppositional stance that marginalized communities take
against what is perceived as a potentially hostile intervention by
outsiders. Another challenge has been maintaining the potency
of live (attenuated) vaccines in extremely hot or remote areas. The
oral polio vaccine must be kept at 2 to 8 °C (36 to 46 °F) for
vaccination to be successful.
An independent evaluation of obstacles to polio eradication
requested by the WHO and conducted in 2009 considered the major
obstacles in detail by country. In Afghanistan and Pakistan, they
concluded that the most significant barrier was insecurity; but that
managing human resources, political pressures, the movement of large
populations between and within both countries, inadequately resourced
health facilities, also posed problems, as well as technical issues with
the vaccine. In India, the major challenge appeared to be the high efficiency of transmission within the populations of Bihar and Uttar Pradesh states, set against the low (~80% after three doses against type 1) seroconversion
response seen from the vaccine. In Nigeria, meanwhile, the most
critical barriers identified were management issues, in particular the
highly variable importance ascribed to polio by different authorities at
the local government level, although funding issues, community
perceptions of vaccine safety, inadequate mobilisation of community
groups, and issues with the cold chain also played a role. Finally, in
those countries where international spread from endemic countries had
resulted in transmission becoming re-established—namely Angola, Chad, and South Sudan,
the key issues identified were underdeveloped health systems and low
routine vaccine coverage, although low resources committed to Angola and
South Sudan for the purpose of curtailing the spread of polio and
climatic factors were also identified as playing a role.
Two additional challenges are found in unobserved polio
transmission and in vaccine-derived poliovirus. First, most polio
infections are asymptomatic or result in minor symptoms, with less than
1% of infections leading to paralysis and most infected people are unaware that they carry the disease, allowing polio to spread widely before cases are seen.
In 2000 using new screening techniques for the molecular
characterization of outbreak viral strains, it was discovered that some
of the outbreaks taking place were actually caused by circulating
vaccine-derived poliovirus, following mutations or recombinations in the
attenuated strain used for the oral polio vaccine. This altered the
strategy envisioned for the discontinuation of vaccination following
polio eradication,
necessitating an eventual switch to the more expensive and logistically
more problematic inactivated polio vaccine, since continued use of the
oral inactivated virus would continue to produce such revertant
infection-causing strains. The risk of vaccine-derived polio will persist long after the switch to inactivated vaccine, since a small number of chronic excretors continue to produce active virus for years (or even decades) after their initial exposure to the oral vaccine.
In a 2012 interview with Pakistani newspaper Dawn,
Dr. Hussain A. Gezari, WHO's special envoy on global polio eradication
and primary healthcare, gave his views on obstacles to eradication. He
said the biggest hurdle in making Pakistan polio-free was holding
district health officials properly accountable—in national eradication
campaigns officials had hired their own relatives, even young children.
"How do you expect a seven-year-old thumb-sucking kid to implement a
polio campaign of the government," said Dr Gezari. He added that, in
spite of this, "the first national campaign was initiated by your
government in 1994 and that year Pakistan reported 25,000 polio cases,
and the number was just 198 last year, which clearly shows that the
programme is working."
Opposition to vaccination efforts
One factor contributing to the continued circulation of polio immunization programs has been opposition in some countries.
In the context of the United States invasion of Afghanistan and the subsequent 2003 invasion of Iraq,
rumours arose in the Muslim world that immunization campaigns were
using intentionally-contaminated vaccines to sterilize local Muslim
populations or to infect them with HIV.
In Nigeria these rumours fit in with a longstanding suspicion of
modern biomedicine, which since its introduction during the era of colonialism
has been viewed as a projection of the power of western nations.
Refusal of vaccination came to be viewed as resistance to western
expansionism, and when the contamination rumours led the Nigerian
Supreme Council for Sharia to call for a region-wide boycott of polio
vaccination, polio cases in the country increased more than five-fold
between 2002 and 2006, with the uncontrolled virus then spreading across
Africa and globally. In Afghanistan and Pakistan, fears that the vaccine contained contraceptives were one reason given by the Taliban in issuing fatwas against polio vaccination. Skepticism in the Muslim world was exacerbated when it was learned in 2011 that the Central Intelligence Agency (CIA) had conducted a fake hepatitis B immunization campaign to collect blood samples from Osama bin Laden's Abbottabad compound
in order to confirm the genetic identity of the children living there,
and by implication his own presence, leading directly to his killing. In a letter written to CIA director Leon Panetta, the InterAction Alliance,
a union of about 200 U.S.-based non-government organizations, deplored
the actions of the CIA in using a vaccination campaign as a cover. Pakistan reported the world's highest number of polio cases (198) in 2011.
Religious boycotts based on contamination concerns have not been
limited to the Muslim world. In 2015, after claiming that a tetanus
vaccine contained a contraceptive, a group of Kenyan Catholic bishops
called on their followers to boycott a planned round of polio
vaccination. This did not have a major effect on vaccination rates, and
dialog along with vaccine testing forestalled further boycott calls.
Other religion-inspired refusals arise from concerns over whether the virus contains pig-derived products, and hence are haram (forbidden) in Islam, prohibitions against taking of animal life that may be required for vaccine production, or a resistance to interfering with divinely-directed disease processes.
Concerns were addressed through extensive outreach, directed both
toward the communities involved and respected clerical bodies, as well
as promoting local ownership of the eradication campaign in each region.
In early 2012, some parents refused to get their children vaccinated
in Khyber Pakhtunkhwa and in the Federally Administered Tribal Areas (FATA) but religious refusals in the rest of the country had "decreased manifold".
Even with the express support of political leaders, polio workers or
their accompanying security guards have been kidnapped, beaten, or
assassinated.
Polio vaccination efforts have also faced resistance in another
form. The priority placed on vaccination by national authorities has
turned it into a bargaining chip, with communities and interest groups
resisting vaccination, not due to direct opposition, but to leverage
other concessions from governmental authorities. In Nigeria this has
taken the form of 'block rejection' of vaccination that is only resolved
when state officials agree to repair or improve schools and health-care
facilities, pave roads or install electricity. There have been several instances of threatened boycotts by health workers in Pakistan over payment disputes.
Some governments have been accused of withholding vaccination or the
necessary accompanying infrastructure from regions where opposition to
their rule is high.
Polio eradication criteria
A country is regarded as polio free or non-endemic if no cases have been detected for a year.
However, it is still possible polio circulates under these
circumstances, as was the case for Nigeria, where a particular strain of
virus resurfaced after five years in 2016. This can be due to chance, limited surveillance and under-vaccinated populations.
Moreover, for the currently circulating virus WPV1, only 1 in 200
infection cases exhibit symptoms of polio paralysis in non-vaccinated
children, and possibly even fewer in vaccinated children. Therefore, even a single case is considered an epidemic.
According to modeling, it can take four to six months of no reported
cases to achieve only a 50% chance of eradication, and one to two years
for e.g. 95% chance.
Sensitivity of monitoring for circulation can be improved by sampling
sewage. In Pakistan in the last couple of years, the number of paralysis
cases has dropped relatively faster than the positive environmental
samples, which has shown no progress since 2015. The presence of
multiple infections with the same strain in the upstream area may not be
detectable, so there are some saturation effects when monitoring the
number of positive environmental samples.
Furthermore, virus may shed beyond the expected duration of several
weeks in certain individuals. Contagiousness can not be readily
excluded.
For a polio virus to be certified as eradicated worldwide, at least
three years of good surveillance without cases needs to be achieved,
though this period may need to be longer for a strain like WPV3, where a
lower proportion of those infected demonstrate symptoms, or if sewer
samples stay positive. Wild poliovirus type 2 was certified eradicated in 2015, the last case having been detected in 1999.
Wild poliovirus type 3 has not been detected since 2012, but its
eradication has yet to be certified, and the Global Commission for the
Certification of Poliomyelitis Eradication in 2017 recommended not
certifying its eradication independent of that of WPV1, and hence of
wild poliovirus as a whole.
This recommendation would mean that type WPV3 will not be removed from
the bivalent oral vaccine, as was considered necessary with WPV2 due to
its high risk of giving rise to cVDPV strains, but rather oral
vaccination for WPV3 will continue until total eradication of polio
allows all oral vaccination to cease.
Timeline
| International wild poliovirus cases by year | ||
| Year | Estimated | Recorded |
|---|---|---|
| 1975 | — | 49,293 |
| ... | ||
| 1980 | 400,000 | 52,552 |
| ... | ||
| 1985 | — | 38,637 |
| ... | ||
| 1988 | 350,000 | 35,251 |
| ... | ||
| 1990 | — | 23,484 |
| ... | ||
| 1993 | 100,000 | 10,487 |
| ... | ||
| 1995 | — | 7,035 |
| ... | ||
| 2000 | — | 719 |
| ... | ||
| 2005 | — | 1,979 |
| ... | ||
| 2010 | — | 1,352 |
| 2011 | — | 650 |
| 2012 | — | 223 |
| 2013 | — | 416 |
| 2014 | — | 359 |
| 2015 | — | 74 |
| 2016 | — | 37 |
| 2017 | — | 22 |
| 2018 | — | 33 |
Pre-1988
Kindergarten children receive an very early oral polio vaccine in 1960 in East Germany.
Following the widespread use of poliovirus vaccine in the mid-1950s,
the incidence of poliomyelitis declined rapidly in many industrialized
countries. Czechoslovakia became the first country in the world to scientifically demonstrate nationwide eradication of poliomyelitis in 1960. In 1962—just one year after Sabin's oral polio vaccine (OPV) was licensed in most industrialized countries—Cuba
began using the oral vaccine in a series of nationwide polio campaigns.
The early success of these mass vaccination campaigns suggested that
polioviruses could be globally eradicated. The Pan American Health Organization (PAHO), under the leadership of Ciro de Quadros, launched an initiative to eradicate polio from the Americas in 1985.
Much of the work towards eradication was documented by Brazilian photographer Sebastião Salgado, as a UNICEF Goodwill Ambassador, in the book The End of Polio: Global Effort to End a Disease.
1988–2000
In 1988, the World Health Organization, together with Rotary International, UNICEF, and the U.S. Centers for Disease Control and Prevention passed the Global Polio Eradication Initiative, with the goal of eradicating polio by the year 2000. The initiative was inspired by Rotary International's 1985 pledge to raise $120 million toward immunising all of the world's children against the disease. The last case of wild poliovirus poliomyelitis in the Americas was reported in Peru, August 1991.
On 20 August 1994 the Americas were certified as polio-free. This achievement was a milestone in efforts to eradicate the disease.
In 1994 the Indian Government launched the Pulse Polio Campaign to eliminate polio. The current campaign involves annual vaccination of all children under age five.
In 1995 Operation MECACAR (Mediterranean, Caucasus, Central Asian Republics and Russia) were launched; National Immunization Days were coordinated in 19 European and Mediterranean countries. In 1998, Melik Minas of Turkey became the last case of polio reported in Europe. In 1997 Mum Chanty of Cambodia became the last person to contract polio in the Indo-West Pacific region. In 2000 the Western Pacific Region (including China) was certified polio-free.
In October 1999, the last isolation of type 2 poliovirus occurred in India. This type of poliovirus was declared eradicated.
Also in October 1999, The CORE Group—with funding from the United States Agency for International Development
(USAID)—launched its effort to support national eradication efforts at
the grassroots level. The CORE Group initiated this initiative in Bangladesh, India and Nepal in South Asia, and in Angola, Ethiopia and Uganda in Africa.
2001–2005
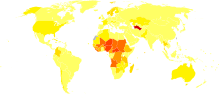
Disability-adjusted life year for poliomyelitis per 100,000 inhabitants in 2004
|
no data
<0 .3="" span="">
0.3–0.75
0.75–1.2
1.2–1.65
1.65–2.1
2.1–2.55
|
2.55–3
3–4
4–5
5–7.5
7.5–10
>10
|
By 2001, 575 million children (almost one-tenth the world's population) had received some 2 billion doses of oral polio vaccine. The World Health Organization announced that Europe was polio-free on 21 June 2002, in the Copenhagen Glyptotek.
In 2002, an outbreak of polio occurred in India. The number of
planned polio vaccination campaigns had recently been reduced, and
populations in northern India, particularly from the Islamic background,
engaged in mass resistance to immunization. At this time, the Indian
state Uttar Pradesh accounted for nearly two-thirds of total worldwide cases reported. However, by 2004, India had adopted strategies to increase ownership of
polio vaccinations in marginalized populations, and the immunity gap in
vulnerable groups rapidly closed.
In August 2003, rumors spread in some states in Nigeria, especially Kano,
that the vaccine caused sterility in girls. This resulted in the
suspension of immunization efforts in the state, causing a dramatic rise
in polio rates in the already endemic country.
On 30 June 2004, the WHO announced that after a 10-month ban on polio
vaccinations, Kano had pledged to restart the campaign in early July.
During the ban the virus spread across Nigeria and into 12 neighboring
countries that had previously been polio-free.
By 2006, this ban would be blamed for 1,500 children being paralyzed
and had cost $450 million for emergency activities. In addition to the
rumors of sterility and the ban by Nigeria's Kano state, civil war and
internal strife in the Sudan and Côte d'Ivoire
have complicated WHO's polio eradication goal. In 2004, almost
two-thirds of all the polio cases in the world occurred in Nigeria (760
out of 1,170 total).
Countries with polio cases in 2005
In May 2004 the first case of the polio outbreak in Sudan was
detected. The reemergence of polio led to stepped up vaccination
campaigns. In the city of Darfur, 78,654 children were immunized and 20,432 more in southern Sudan (Yirol and Chelkou).
In 2005 there were 1,979 cases of wild poliovirus (excludes vaccine-derived polio viruses). Most cases were located in two areas: the Indian subcontinent and Nigeria. Eradication efforts in the Indian sub-continent met with a large measure of success. Using the Pulse Polio campaign to increase polio immunization rates, India recorded just 66 cases in 2005, down from 135 cases reported in 2004, 225 in 2003, and 1,600 in 2002.
Yemen, Indonesia and Sudan, countries that had been declared polio-free since before 2000, each reported hundreds of cases—probably imported from Nigeria. On 5 May 2005, news reports broke that a new case of polio was diagnosed in Java, Indonesia,
and the virus strain was suspected to be the same as the one that has
caused outbreaks in Nigeria. New public fears over vaccine safety, which
were unfounded, impeded vaccination efforts in Indonesia. In summer
2005 the WHO, UNICEF and the Indonesian government made new efforts to
lay the fears to rest, recruiting celebrities and religious leaders in a
publicity campaign to promote vaccination.
In the United States
on 29 September 2005, the Minnesota Department of Health identified the
first occurrence of vaccine derived polio virus (VDPV) transmission in
the United States since OPV was discontinued in 2000. The poliovirus
type 1 infection occurred in an unvaccinated, immunocompromised infant girl aged 7 months (the index patient) in an Amish community whose members predominantly were not vaccinated for polio.
2006–2010
In 2006 only four countries in the world (Nigeria, India, Pakistan and Afghanistan)
were reported to have endemic polio. Cases in other countries are
attributed to importation. A total of 1,997 cases worldwide were
reported in 2006; of these the majority (1,869 cases) occurred in
countries with endemic polio.
Nigeria accounted for the majority of cases (1,122 cases) but India
reported more than ten times more cases this year than in 2005 (676
cases, or 30% of worldwide cases). Pakistan and Afghanistan reported 40
and 31 cases respectively in 2006. Polio re-surfaced in Bangladesh
after nearly six years of absence with 18 new cases reported. "Our
country is not safe, as neighbours India and Pakistan are not polio
free", declared Health Minister ASM Matiur Rahman.
In 2007 there were 1,315 cases of poliomyelitis reported worldwide.
Over 60% of cases (874) occurred in India; while in Nigeria, the number
of polio cases fell dramatically, from 1,122 cases reported in 2006 to
285 cases in 2007. Officials credit the drop in new infections to
improved political control in the southern states and resumed
immunisation in the north, where Muslim clerics led a boycott of
vaccination in late 2003. Local governments and clerics allowed
vaccinations to resume on the condition that the vaccines be
manufactured in Indonesia, a majority Muslim country, and not in the
United States. Turai Yar'Adua, wife of recently elected Nigerian president Umaru Yar'Adua, made the eradication of polio one of her priorities. Attending the launch of immunization campaigns in Birnin Kebbi in July 2007, Turai Yar'Adua urged parents to vaccinate their children and stressed the safety of oral polio vaccine.
In July 2007, a student traveling from Pakistan imported the first polio case to Australia in over 20 years. Other countries with significant numbers of wild polio virus cases include the Democratic Republic of the Congo, which reported 41 cases, Chad with 22 cases, and Niger and Myanmar, each of which reported 11 cases.
In 2008, 19 countries reported cases and the total number of
cases was 1,652. Of these, 1,506 occurred in the four endemic countries
and 146 elsewhere. The largest number were in Nigeria (799 cases) and
India (559 cases): these two countries contributed 82.2 percent of all
cases. Outside endemic countries Chad reported the greatest number (37
cases).
In 2009, a total of 1,606 cases were reported in 23 countries.
Four endemic countries accounted for 1,256 of these, with the remaining
350 in 19 sub-Saharan countries with imported cases or re-established
transmission. Once again, the largest number were in India (741) and
Nigeria (388). All other countries had less than one hundred cases: Pakistan had 89 cases, Afghanistan 38, Chad 65, Sudan 45, Guinea 42, Angola 29, Côte d'Ivoire 26, Benin 20, Kenya 19, Niger 15, Central African Republic 14, Mauritania 13 and Sierra Leone and Liberia both had 11. The following countries had single digit numbers of cases: Burundi 2, Cameroon 3, the Democratic Republic of the Congo 3, Mali 2, Togo 6 and Uganda 8.
According to figures updated in April 2012, the WHO reported that
there were 1,352 cases of wild polio in 20 countries in 2010. Reported
cases of polio were down 95% in Nigeria (to a historic low of 21 cases)
and 94% in India (to a historic low of 42 cases) compared to the
previous year, with little change in Afghanistan (from 38 to 25 cases)
and an increase in cases in Pakistan (from 89 to 144 cases). An acute
outbreak in Tajikistan gave rise to 460 cases (34% of the global total), and was associated with a further 18 cases across Central Asia (Kazakhstan and Turkmenistan)
and the Russian Federation, with the most recent case from this region
being reported from Russia 25 September. These were the first cases in
the WHO European region since 2002. The Republic of Congo (Brazzaville)
saw an outbreak with 441 cases (30% of the global total). At least 179
deaths were associated with this outbreak, which is believed to have
been an importation from the ongoing type 1 outbreak in Angola (33 cases
in 2010) and the Democratic Republic of the Congo (100 cases).
2011–2015
In
2011, 650 WPV cases were reported in sixteen countries: the four
endemic countries—Pakistan, Afghanistan, Nigeria and India—as well as
twelve others. Polio transmission recurred in Angola, Chad and the
Democratic Republic of the Congo. Kenya reported its first case since 2009, while China reported 21 cases, mostly among the Uyghurs of Hotan prefecture, Xinjiang, the first cases since 1994.
The total number of wild-virus cases reported in 2012 was 223,
lower than any previous year. These were limited to five
countries—Nigeria, Pakistan, Afghanistan, Chad, and Niger—of which all
except Nigeria had fewer cases than in 2011.
Several additional countries, Chad, Democratic Republic of the Congo,
Somalia and Yemen, saw outbreaks of circulating vaccine-derived polio.
The last reported type 3 case of polio worldwide had its onset 11
November 2012 in Nigeria; the last wild case outside Nigeria was in
April 2012 in Pakistan, and its absence from sewage monitoring in Pakistan suggests that active transmission of this strain has ceased there.
A total of 416 wild-virus cases were reported in 2013, almost double
the previous year. Of these, cases in endemic countries dropped from 197
to 160, while those in non-endemic countries jumped from 5 to 256 owing
to two outbreaks: one in the Horn of Africa, and one in Syria.
In April, a case of wild polio in Mogadishu was reported, the first in Somalia since 2007. By October, over 170 cases had been reported in the country, with more cases in neighboring Kenya and the Somali Region of Ethiopia.
Routine sewage monitoring in 2012 had detected a WPV1 strain of Pakistani origin in Cairo, sparking a major vaccination push there. The strain spread to Israel, where there was widespread environmental detection, but like Egypt, no paralysis cases.
It had more severe consequences when it spread to neighboring Syria,
with the total number of cases eventually reaching 35, the first
outbreak there since 1999.
In late April 2013, the WHO announced a new $5.5 billion, 6-year
cooperative plan (called the 2013–18 Polio Eradication and Endgame
Strategic Plan) to eradicate polio from its last reservoirs. The plan
called for mass immunization campaigns in the three remaining endemic
countries, and also dictated a switch to inactivated virus injections,
to avoid the risk of the vaccine-derived outbreaks that occasionally
occur from use of the live-virus oral vaccine.
In 2014, there were 359 reported cases of wild poliomyelitis,
spread over twelve countries. Pakistan had the most with 306, an
increase from 93 in 2013, which was blamed on Al Qaeda and Taliban
militants preventing aid workers from vaccinating children in rural
regions of the country.
On 27 March 2014, the WHO announced the eradication of poliomyelitis
in the South-East Asia Region, in which the WHO includes eleven
countries: Bangladesh, Bhutan, North Korea, India, Indonesia, Maldives, Myanmar, Nepal, Sri Lanka, Thailand and Timor-Leste. With the addition of this region, the proportion of world population living in polio-free regions reached 80%. The last case of wild polio in the South-East Asia Region was reported in India on 13 January 2011.
During 2015, 74 cases of wild poliomyelitis were reported
worldwide, 54 in Pakistan and 20 in Afghanistan. There were 32
circulating vaccine-derived poliovirus (cVDPV) cases in 2015.
On 25 September 2015, the WHO declared that Nigeria was no longer considered endemic for wild polio virus, with no reported case of wild polio virus having been reported since 24 July 2014. A WPV1 strain not seen in 5 years resurfaced in Nigeria the following year.
WPV2 was declared eradicated in September 2015 as it has not been
seen since 1999 and WPV3 may be eradicated as it has not been seen
since 2012. cVDPV type 2 was still causing paralysis in some countries
due to a years-long evolution in under-immunized populations.
Reported polio cases in 2013
Reported polio cases in 2014
Reported polio cases in 2015
2016
There were 37 reported WPV1 cases with an onset of paralysis in 2016,
half as many as in 2015. Twenty of these cases occurred in Pakistan,
thirteen in Afghanistan, and four in Nigeria.
The cases of WPV1 in Nigeria were viewed as a setback, there having
been no detected cases caused by the wild virus there in almost two
years, yet genetic analysis showed that the virus was of a strain
circulating undetected since 2011 in regions inaccessible due to the
activities of Boko Haram.
The 2015 cVDPV1 outbreak in Laos continued into 2016, with three cases in January.
Two separate strains of cVDPV2 were reported in Nigeria's Borno and
Sekoto states, the latter resulting in one case. In Pakistan a new
strain of cVDPV2 arose in the Quetta area, with one instance of
paralysis.
Environmental samples from Hyderabad, India from January 2015 to May 2016 showed the ongoing presence of a cVDPV2 strain in that city, without diagnosed cases.
Due to shortages in the global supply of injectable vaccine, an
emergency campaign was launched using vaccine at one fifth the normal
dose (fractional-Dose Inactivated Polio Vaccine, or fIPV), the first
mass vaccination using this dosage of injectable vaccine.
Attacks on polio vaccination campaigns continued. A suicide
bombing in Quetta in January and a pair of attacks by gunmen in Karachi
in April targeted Pakistani security personnel protecting vaccinators, while in January three Afghan vaccination workers disappeared and their bodies were found weeks later.
Because cVDPV2 strains continued to arise from trivalent oral
vaccine that included attenuated WPV2, in April and May 2016 this
vaccine was replaced with a bivalent version lacking WPV2 as well as
trivalent injected inactivated vaccine that cannot lead to cVDPV cases.
This is expected to prevent new strains of cVDPV2 from arising and allow
eventual cessation of WPV2 vaccination.
2017
There were 22 reported WPV1 polio cases with onset of paralysis in
2017, down from 37 in 2016. Eight of the cases were in Pakistan and 14
in Afghanistan, where genetic typing showed repeated introduction from Pakistan as well as local transmission.
In Pakistan, transmission of several genetic lineages of WPV1 seen in
2015 had been interrupted by September 2017, though at least two genetic
clusters remain. In spite of a significant drop in detected cases in
Pakistan, there was an increase in the percentage of environmental
samples that test positive for the polio virus, suggesting gaps in
identification of infected individuals.
In the third country where polio remains endemic, Nigeria, there were
no cases, though as few as 7% of infants were fully vaccinated in some
districts. An April 2017 spill at a vaccine production facility in the Netherlands resulted in one asymptomatic infection.
Laos was declared free of cVDPV1 in March,
but three distinct cVDPV2 outbreaks occurred in the Democratic Republic
of the Congo, one of them or recent origin, the other two having
circulated undetected for more than a year. Together they caused 20
cases by year's end. In Syria a large outbreak began at Mayadin, Deir ez-Zor Governorate, a center of fighting in the Syrian Civil War
and also spreading to neighboring districts saw 74 confirmed cases from
a viral strain that had circulated undetected for about two years.
Circulation of multiple genetic lines of cVDPV2 was also detected in
Banadir province, Somalia, but no infected individuals were identified.
WHO's Strategic Advisory Group of Experts on Immunization recommended
that cVDPV2 suppression be prioritized over targeting WPV1, and according to protocol OPV2 is restricted to this purpose.
The 2016 global switch in vaccination methods resulted in shortages of the injectable vaccine, and led the WHO in April 2017 to recommend general use of the fIPV vaccination protocol, involving subcutaneous injection of a lower dose than used in the standard intramuscular delivery.
2018
There were 33 reported WPV1 paralysis cases with an onset of paralysis in 2018 – 21 in Afghanistan and 12 in Pakistan. In Pakistan, three of the cases occurred in Kohlu District in Balochistan, with eight in Khyber Pakhtunkhwa, and one in the greater Karachi area, Sindh.
Viral circulation across much of the country, including several major
urban areas, led to wild poliovirus detection in 20% of the year's
environmental samples. The rates of parental refusal for vaccination are increasing. Cases in Afghanistan represented two transmission clusters, one in Kandahar, Urozgan and Helmand Provinces in the south, the other in the adjacent Nuristan, Kunar and Nangarhar Provinces in the northeast, on the Pakistani border.
Roughly half of recent Afghanistan isolates were genetically closer to
isolates from Pakistan than to other Afghani samples, suggesting
significant trans-border transmission. Recent cases in Afghanistan and Pakistan are due to three genetic clusters: R4B5C5B2 in the northern corridor in both countries, and the remaining cases are R4B5C4D in Pakistan, including five near the northern corridor, and R4B5C4C in Afghanistan. Though in 2017, nine of the detected viruses derived from long chains of undetected transmission, such long-chain transmission may have subsided in both Pakistan and Afghanistan in 2018, with the total number of circulating viral strains also dropping in both countries.
Nigeria, the third country classified as having endemic transmission,
passed two full years without a detected wild-virus case, but security
concerns continued to limit access to some areas of the country and
elimination of WPV transmission could not be confirmed.
Cases caused by vaccine-derived poliovirus were reported in seven
countries, with more than 100 total cases. Surveillance detected nine
strains of cVDPV in 2018 in seven countries.
In the Democratic Republic of Congo, one of the outbreaks of cVDPV2
first detected in 2017 caused no additional cases, but suppression of
the other two with OPV2 proved insufficient: not only did they continue,
but the vaccination efforts gave rise to a novel cVDPV2 outbreak. The country experienced a total of 20 cases in 2018. Two separate cVDPV2 outbreaks in northern Nigeria produced 34 cases,
as well as giving rise to 10 cases in the neighboring Niger. In
Somalia, cVDPV2 continued to circulate, causing several polio cases and
detected in environmental samples from as far as Nairobi,
Kenya. This virus, along with newly-detected cVDPV3, caused twelve
total cases in the country, including one patient infected by both
strains.
The large number of children residing in areas inaccessible to health
workers represent a particular risk for undetected cVDPV outbreaks. A cVDPV2 outbreak in Mozambique also resulted in a single case. Response to the Syrian cVDPV2 outbreak continued into 2018, and virus transmission was successfully interrupted. In Papua New Guinea, a cVDPV1 strain arose, causing twenty-six polio cases across 9 provinces, while a single diagnosed cVDPV1 case in neighboring Western New Guinea, Indonesia, resulted from a distinct outbreak.
2019
As of 12 June, twenty nine WPV1 paralysis cases had been detected in 2019, eight in Afghanistan and twenty one in Pakistan, with the latter already exceeding total the number of cases in the country in 2018. Trans-border migration continues to play a role in polio transmission in the two countries.
While problematic, this has fostered a dangerous false-narrative in
both nations, blaming the other for the presence and spread of polio in
their own country.
Environmental sampling in Pakistan has recently shown the virus'
presence in eight urban areas, a setback officials attribute primarily
to vaccine refusal.
Opponents to vaccination in Pakistan launched a series of attacks in
April that left a vaccinator and two security men dead, while false
rumors and hoax videos reporting vaccine toxicity have also disrupted
vaccination efforts there. Wild poliovirus of Pakistani origin has also been detected in environmental samples in Iran.
The cVDPV2 outbreaks in Nigeria, the Democratic Republic of
Congo, and Somalia continued into 2019. The Nigeria outbreaks have
caused eight reported paralysis cases, plus one in neighboring Niger,
while cVDPV2 virus has also been detected in environmental samples from
Cameroon. Somalia has seen two cases, while the DRC has had one case. A
new outbreak has caused one case in Angola, in a region bordering where
OPV2 vaccine had been used to fight the DRC outbreak.