| Liver transplantation | |
|---|---|

Human liver
| |
| Specialty | hepatology |
| ICD-9-CM | 50.5 |
| MeSH | D016031 |
| MedlinePlus | 003006 |
Liver transplantation or hepatic transplantation is the replacement of a diseased liver with the healthy liver from another person (allograft). Liver transplantation is a treatment option for end-stage liver disease and acute liver failure, although availability of donor organs is a major limitation. The most common technique is orthotopic transplantation, in which the native liver is removed and replaced by the donor organ in the same anatomic position as the original liver. The surgical procedure is complex, requiring careful harvest of the donor organ and meticulous implantation into the recipient. Liver transplantation is highly regulated, and only performed at designated transplant medical centers by highly trained transplant physicians and supporting medical team. The duration of the surgery ranges from 4 to 18 hours depending on outcome. Favorable outcomes require careful screening for eligible recipient, as well as a well-calibrated live or cadaveric donor match.
Medical uses
Liver
transplantation is a potential treatment for acute or chronic
conditions which cause irreversible and severe ("end-stage") liver
dysfunction.
Since the procedure carries relatively high risks, is
resource-intensive, and requires major life-modifications after surgery,
it is reserved for dire circumstances.
Judging the appropriateness/effectiveness of liver transplant on case-by-case basis is critically important, as outcomes are highly variable.
Contraindications
Although
liver transplantation is the most effective treatment for many forms of
end-stage liver disease, the tremendous limitation in allograft
availability and widely variable post-surgical outcomes make case
selection critically important. Assessment of a person's transplant
eligibility is made by a multi-disciplinary team that includes surgeons,
medical doctors, and other providers.
The first step in evaluation is to determine whether the patient
has irreversible liver-based disease which will be cured by getting a
new liver.
Thus, those with diseases which are primarily based outside the liver or
have spread beyond the liver are generally considered poor candidates.
Some examples include:
- someone with advanced liver cancer, with known/likely spread beyond the liver
- active alcohol/substance abuse
- severe heart/lung disease
- existing high cholesterol levels in the patient
- dyslipidemia
Importantly, many contraindications to liver transplantation are
considered reversible; a person initially deemed "transplant-ineligible"
may later become a favorable candidate if their situation changes. Some examples include:
- partial treatment of liver cancer, such that risk of spread beyond liver is decreased (for those with primary liver cancer or secondary spread to the liver, the medical team will likely rely heavily on the opinion of the patient's primary provider, the oncologist, and the radiologist)
- cessation of substance abuse (time period of abstinence is variable)
- improvement in heart function, e.g. by percutaneous coronary intervention or bypass surgery
- treated HIV infection (see Special populations)
- for those with high cholesterol or triglyceride levels or other dyslipidemias, using lifestyle changes (diet, portions, exercise) and drugs and counseling to lower one's levels, and to control any hyperglycemia or (pre-)diabetes or obesity
Risks/complications
Graft rejection
After a liver transplantation, immune-mediated rejection (also known as rejection)
of the allograft may happen at any time. Rejection may present with lab
findings: elevated AST, ALT, GGT; abnormal liver function values such
as prothrombin time, ammonia level, bilirubin level, albumin
concentration; and abnormal blood glucose. Physical findings may include
encephalopathy, jaundice, bruising and bleeding tendency. Other
nonspecific presentation may include malaise, anorexia, muscle ache, low
fever, slight increase in white blood count and graft-site tenderness.
Three types of graft rejection may occur: hyperacute rejection, acute rejection, and chronic rejection.
- Hyperacute rejection is caused by preformed anti-donor antibodies. It is characterized by the binding of these antibodies to antigens on vascular endothelial cells. Complement activation is involved and the effect is usually profound. Hyperacute rejection happens within minutes to hours after the transplant procedure.
- Acute rejection is mediated by T cells (versus B-cell-mediated hyperacute rejection). It involves direct cytotoxicity and cytokine mediated pathways. Acute rejection is the most common and the primary target of immunosuppressive agents. Acute rejection is usually seen within days or weeks of the transplant.
- Chronic rejection is the presence of any sign and symptom of rejection after one year. The cause of chronic rejection is still unknown, but an acute rejection is a strong predictor of chronic rejections.
Technique
Before transplantation, liver-support therapy might be indicated (bridging-to-transplantation). Artificial liver support like liver dialysis
or bioartificial liver support concepts are currently under preclinical
and clinical evaluation. Virtually all liver transplants are done in an
orthotopic fashion; that is, the native liver is removed and the new
liver is placed in the same anatomic location.
The transplant operation can be conceptualized as consisting of the
hepatectomy (liver removal) phase, the anhepatic (no liver) phase, and
the postimplantation phase. The operation is done through a large
incision in the upper abdomen. The hepatectomy involves division of all
ligamentous attachments to the liver, as well as the common bile duct,
hepatic artery, hepatic vein and portal vein. Usually, the retrohepatic
portion of the inferior vena cava is removed along with the liver,
although an alternative technique preserves the recipient's vena cava
("piggyback" technique).
The donor's blood in the liver will be replaced by an ice-cold organ storage solution, such as UW (Viaspan) or HTK
until the allograft liver is implanted. Implantation involves
anastomoses (connections) of the inferior vena cava, portal vein, and
hepatic artery. After blood flow is restored to the new liver, the
biliary (bile duct) anastomosis is constructed, either to the
recipient's own bile duct or to the small intestine. The surgery usually
takes between five and six hours, but may be longer or shorter due to
the difficulty of the operation and the experience of the surgeon.
The large majority of liver transplants use the entire liver from
a non-living donor for the transplant, particularly for adult
recipients. A major advance in pediatric liver transplantation was the
development of reduced size liver transplantation, in which a portion of
an adult liver is used for an infant or small child. Further
developments in this area included split liver transplantation, in which
one liver is used for transplants for two recipients, and living donor
liver transplantation, in which a portion of a healthy person's liver is
removed and used as the allograft. Living donor liver transplantation
for pediatric recipients involves removal of approximately 20% of the
liver (Couinaud segments 2 and 3).
Further advance in liver transplant involves only resection of
the lobe of the liver involved in tumors and the tumor-free lobe remains
within the recipient. This speeds up the recovery and the patient stay
in the hospital quickly shortens to within 5–7 days.
Many major medical centers are now using radiofrequency ablation
of the liver tumor as a bridge while awaiting for liver transplantation.
This technique has not been used universally and further investigation
is warranted.
Cooling
Between
removal from donor and transplantation into the recipient, the
allograft liver is stored in a temperature-cooled preservation solution.
The reduced temperature slows down the process of deterioration from
normal metabolic processes, and the storage solution itself is designed
to counteract the unwanted effects of cold ischemia. Although this
"static" cold storage method has long been standard technique, various
dynamic preservation methods are under investigation. For example,
systems which use a machine to pump blood through the explanted liver
(after it is harvested from the body) during a transfer have met some
success.
Living donor transplantation
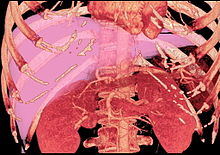
Volume rendering image created with computed tomography, which can be used to evaluate the volume of the liver of a potential donor.
Living donor liver transplantation (LDLT) has emerged in recent decades as a critical surgical option for patients with end stage liver disease, such as cirrhosis and/or hepatocellular carcinoma often attributable to one or more of the following: long-term alcohol abuse, long-term untreated hepatitis C infection, long-term untreated hepatitis B
infection. The concept of LDLT is based on (1) the remarkable
regenerative capacities of the human liver and (2) the widespread
shortage of cadaveric livers for patients awaiting transplant.
In LDLT, a piece of healthy liver is surgically removed from a living
person and transplanted into a recipient, immediately after the
recipient’s diseased liver has been entirely removed.
Historically, LDLT began with terminal pediatric patients, whose
parents were motivated to risk donating a portion of their compatible
healthy livers to replace their children's failing ones. The first
report of successful LDLT was by Christoph Broelsch at the University of Chicago Medical Center in November 1989, when two-year-old Alyssa Smith received a portion of her mother's liver.
Surgeons eventually realized that adult-to-adult LDLT was also
possible, and now the practice is common in a few reputable medical
institutes. It is considered more technically demanding than even
standard, cadaveric donor liver transplantation, and also poses the
ethical problems underlying the indication of a major surgical operation
(hemihepatectomy
or related procedure) on a healthy human being. In various case series,
the risk of complications in the donor is around 10%, and very
occasionally a second operation is needed. Common problems are biliary fistula, gastric stasis and infections;
they are more common after removal of the right lobe of the liver.
Death after LDLT has been reported at 0% (Japan), 0.3% (USA) and <1 2006="" 2012.="" altruistic="" as="" britain="" changed="" december="" decrease="" donation="" donations="" experience="" first="" further="" gain="" in="" law="" likely="" liver="" living="" more="" non-directed="" organ="" p="" permit="" place="" procedure.="" risks="" since="" surgeons="" the="" this="" to="" took="" uk="" urope="" was="" with="">
In a typical adult recipient LDLT, 55 to 70% of the liver (the
right lobe) is removed from a healthy living donor. The donor's liver
will regenerate approaching 100% function within 4–6 weeks, and will
almost reach full volumetric size with recapitulation of the normal
structure soon thereafter. It may be possible to remove up to 70% of the
liver from a healthy living donor without harm in most cases. The
transplanted portion will reach full function and the appropriate size
in the recipient as well, although it will take longer than for the
donor.
Living donors are faced with risks and/or complications after the
surgery. Blood clots and biliary problems have the possibility of
arising in the donor post-op, but these issues are remedied fairly
easily. Although death is a risk that a living donor must be willing to
accept prior to the surgery, the mortality rate of living donors in the
United States is low. The LDLT donor's immune system does diminish as a
result of the liver regenerating, so certain foods which would normally
cause an upset stomach could cause serious illness.
Donor requirements
CT scan
performed for evaluation of a potential donor. The image shows an
unusual variation of hepatic artery. The left hepatic artery supplies
not only left lobe but also segment 8. The anatomy makes right lobe
donation impossible. Even used as left lobe or lateral segment donation,
it would be very technically challenging in anastomosing the small
arteries.
Any member of the family, parent, sibling, child, spouse or a volunteer can donate their liver. The criteria
for a liver donation include:
- Being in good health
- Having a blood type that matches or is compatible with the recipient's, although some centres now perform blood group incompatible transplants with special immunosuppression protocols
- Having a charitable desire of donation without financial motivation
- Being between 20 and 60 years old
- Have an important personal relationship with the recipient
- Being of similar or larger size than the recipient
- Before one becomes a living donor, the donor must undergo testing to ensure that the individual is physically fit, in excellent health, and not having uncontrolled high blood pressure, liver disease, diabetes or heart disease. Sometimes CT scans or MRIs are done to image the liver. In most cases, the work up is done in 2–3 weeks.
Complications
Living donor surgery is done at a major center. Very few individuals require any blood transfusions
during or after surgery. All potential donors should know there is a
0.5 to 1.0 percent chance of death. Other risks of donating a liver
include bleeding, infection, painful incision, possibility of blood clots and a prolonged recovery. The vast majority of donors enjoy complete and full recovery within 2–3 months.
Pediatric transplantation
In children, due to their smaller abdominal cavity,
there is only space for a partial segment of liver, usually the left
lobe of the donor's liver. This is also known as a "split" liver
transplant. There are four anastomoses required for a "split" liver transplant: hepaticojejunostomy (biliary drainage connecting to a roux limb of jejunum), portal venous anatomosis, hepatic arterial anastomosis, and inferior vena cava anastomosis.
In children, living liver donor transplantations have become very
accepted. The accessibility of adult parents who want to donate a piece
of the liver for their children/infants has reduced the number of
children who would have otherwise died waiting for a transplant. Having a
parent as a donor also has made it a lot easier for children - because
both patients are in the same hospital and can help boost each other's
morale.
Benefits
There are several advantages of living liver donor transplantation over cadaveric donor transplantation, including:
- Transplant can be done on an elective basis because the donor is readily available
- There are fewer possibilities for complications and death than there would be while waiting for a cadaveric organ donor
- Because of donor shortages, UNOS has placed limits on cadaveric organ allocation to foreigners who seek medical help in the USA. With the availability of living donor transplantation, this will now allow foreigners a new opportunity to seek medical care in the USA.
Screening for donors
Living
donor transplantation is a multidisciplinary approach. All living liver
donors undergo medical evaluation. Every hospital which performs
transplants has dedicated nurses that provide specific information about
the procedure and answer questions that families may have. During the
evaluation process, confidentiality is assured on the potential donor.
Every effort is made to ensure that organ donation is not made by
coercion from other family members. The transplant team provides both
the donor and family thorough counseling and support which continues
until full recovery is made.
All donors are assessed medically to ensure that they can undergo
the surgery. Blood type of the donor and recipient must be compatible
but not always identical. Other things assessed prior to surgery include
the anatomy of the donor liver. However, even with mild variations in blood vessels and bile duct,
surgeons today are able to perform transplantation without problems.
The most important criterion for a living liver donor is to be in
excellent health.
Post-transplant immunosuppression
Like most other allografts, a liver transplant will be rejected by the recipient unless immunosuppressive
drugs are used. The immunosuppressive regimens for all solid organ
transplants are fairly similar, and a variety of agents are now
available. Most liver transplant recipients receive corticosteroids plus a calcineurin inhibitor such as tacrolimus or ciclosporin, (also spelled cyclosporine and cyclosporin) plus a purine antagonist such as mycophenolate mofetil. Clinical outcome is better with tacrolimus than with ciclosporin during the first year of liver transplantation.
If the patient has a co-morbidity such as active hepatitis B, high
doses of hepatitis B immunoglubins are administrated in liver transplant
patients.
Liver transplantation is unique in that the risk of chronic
rejection also decreases over time, although the great majority of
recipients need to take immunosuppressive medication for the rest of
their lives. It is possible to be slowly taken off anti rejection
medication but only in certain cases. It is theorized that the liver may
play a yet-unknown role in the maturation of certain cells pertaining
to the immune system. There is at least one study by Thomas E. Starzl's team at the University of Pittsburgh which consisted of bone marrow biopsies taken from such patients which demonstrate genotypic chimerism in the bone marrow of liver transplant recipients.
Recovery and outcomes
The
prognosis following liver transplant is variable, depending on overall
health, technical success of the surgery, and the underlying disease
process affecting the liver. There is no exact model to predict survival rates; those with transplant have a 58% chance of surviving 15 years.
Failure of the new liver occurs in 10% to 15% of all cases. These
percentages are contributed to by many complications. Early graft
failure is probably due to preexisting disease of the donated organ.
Others include technical flaws during surgery such as revascularization
that may lead to a nonfunctioning graft.
History
As with
many experimental models used in early surgical research, the first
attempts at liver transplantation were performed on dogs. The earliest
published reports of canine liver transplantations were performed in
1955 by Vittorio Staudacher at Opedale Maggiore Policlinico in Milan,
Italy. This initial attempt varied significantly from contemporary
techniques; for example, Staudacher reported "arterialization" of the
donor portal vein via the recipient hepatic artery, and use of
cholecystostomy for biliary drainage.
The first attempted human liver transplant was performed in 1963 by Thomas Starzl, although the pediatric patient died intraoperatively due to uncontrolled bleeding.
Multiple subsequent attempts by various surgeons remained unsuccessful
until 1967, when Starzl transplanted a 19 month old girl with hepatoblastoma who was able to survive for over 1 year before dying of metastatic disease.
Despite the development of viable surgical techniques, liver
transplantation remained experimental through the 1970s, with one year
patient survival in the vicinity of 25%. The introduction of ciclosporin by Sir Roy Calne,
Professor of Surgery Cambridge, markedly improved patient outcomes, and
the 1980s saw recognition of liver transplantation as a standard
clinical treatment for both adult and pediatric patients with
appropriate indications.
Liver transplantation is now performed at over one hundred centers in
the US, as well as numerous centres in Europe and elsewhere.
The limited supply of liver allografts from non-living donors relative to the number of potential recipients spurred the development of living donor liver transplantation. The first altruistic living liver donation in Britain was performed in December 2012 in St James University Hospital Leeds.
Society and culture
Famous liver transplant recipients
- Eric Abidal (born 1979), French footballer (Olympique Lyonnais, FC Barcelona), transplant in 2012
- Gregg Allman (1947-2017), American musician (The Allman Brothers Band), transplant in 2010 (survival: 7 years)
- George Best (1946-2005), Northern-Irish footballer (Manchester United), transplant in 2002 (survival: 3 years)
- David Bird (1959–2014), American journalist (The Wall Street Journal), transplant in 2004 (survival: 10 years)
- Jack Bruce (1943-2014), English musician (Cream), transplant in 2003 (survival: 11 years)
- Robert P. Casey (1932-2000), American politician (42nd Governor of Pennsylvania), transplant in 1993 (survival: 7 years)
- David Crosby (born 1941), American musician (The Byrds, Crosby Stills, Nash (& Young)), transplant in 1994
- Gerald Durrell (1925-1995), British zookeeper (Durrell Wildlife Park), transplant in 1994 (survival <1 small="" year="">
- Shelley Fabares (born 1944), American actress (The Donna Reed Show, Coach) and singer ("Johnny Angel"), transplant in 2000
- Freddy Fender (1937-2006), American musician ("Before the Next Teardrop Falls," "Wasted Days and Wasted Nights"), transplant in 2004 (survival: 2 years)
- "Superstar" Billy Graham (born 1943), American wrestler (WWF), transplant in 2002
- Larry Hagman (1931-2012), American actor (Dallas, Harry and Tonto, Nixon, Primary Colors), transplant in 1995 (survival: 17 years)
- Steve Jobs (1955-2011), American businessman (Apple Inc.), transplant in 2009 (survival: 2 years)
- Chris Klug (born 1972), American snowboarder, transplant in 2000
- Evel Knievel (1938-2007), American stunt performer, transplant in 1999 (survival: 8 years)
- Chris LeDoux (1948-2005), American musician and rodeo champion, transplant in 2000 (survival: 5 years)
- Phil Lesh (born 1940), American musician (Grateful Dead), transplant in 1998
- Linda Lovelace (1949-2002), American pornographic actress (Deep Throat), transplant in 1987 (survival: 15 years)
- Mickey Mantle (1931-1995), American baseball player (New York Yankees), transplant in 1995 (survival: <1 small="" year="">
- Mike MacDonald (1954-2018), Canadian comedian and actor (Mr. Nice Guy), transplant in 2013 (survival: 5 years)
- Jim Nabors (1930-2017), American actor (The Andy Griffith Show), transplant in 1994 (survival: 23 years)
- John Phillips (1935-2001), American musician (The Mamas & the Papas), transplant in 1992 (survival: 9 years)
- Lou Reed (1942-2013), American musician (The Velvet Underground), transplant in 2013 (survival: <1 small="" year="">
- U. Srinivas (1969-2014), Indian musician, transplant in 2014 (survival: <1 small="" year="">
Research directions
Cooling
There
is increasing interest in improving methods for allograft preservation
following organ harvesting. The standard "static cold storage" technique
relies on decreased temperature to slow of anaerobic metabolic
breakdown. This is currently being investigated at cold (hypothermic),
body temperature (normothermic), and under body temperature
(subnormothermic). Hypothermic machine perfusion has been used
successfully at Columbia University and at the University of Zurich.
A 2014 study showed that the liver preservation time could be
significantly extended using a supercooling technique, which preserves
the liver at subzero temperatures (-6 °C)
More recently, the first randomised controlled clinical trial comparing
machine preservation with conventional cold storage showed comparable
outcomes, with better early function, fewer discarded organs, and longer
preservation times compared with cold stored livers.
Special populations
Alcohol dependence
The high incidence of liver transplants given to those with alcoholic cirrhosis
has led to a recurring controversy regarding the eligibility of such
patients for liver transplant. The controversy stems from the view of alcoholism
as a self-inflicted disease and the perception that those with
alcohol-induced damage are depriving other patients who could be
considered more deserving.
It is an important part of the selection process to differentiate
transplant candidates who suffer from alcoholism as opposed to those who
were susceptible to non-dependent alcohol use. The latter who gain
control of alcohol use have a good prognosis following transplantation.
Once a diagnosis of alcoholism has been established, however, it is
necessary to assess the likelihood of future sobriety.
HIV
Historically,
HIV was considered an "absolute" contraindication to liver
transplantation. This was in part due to concern that the infection
would be worsened by the immunosuppressive medication which is required
after transplantation.
However, with the advent of highly active antiretroviral therapy
(HAART), people with HIV have much improved prognosis. Transplantation
may be offered selectively, although consideration of overall health and
life circumstances may still be limiting. Uncontrolled HIV disease
(AIDS) remains an absolute contraindication.