Medicare is a national health insurance program in the United States, begun in 1966 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, but also for some younger people with disability status as determined by the Social Security Administration, as well as people with end stage renal disease and amyotrophic lateral sclerosis (ALS or Lou Gehrig's disease).
In 2018, according to the 2019 Medicare Trustees Report, Medicare
provided health insurance for over 59.9 million individuals—more than
52 million people aged 65 and older and about 8 million younger people.
According to annual Medicare Trustees reports and research by the
government's MedPAC group, Medicare covers about half of healthcare
expenses of those enrolled. Enrollees almost always cover most of the
remaining costs by taking additional private insurance and/or by joining
a public Part C or Part D Medicare health plan. No matter which of
those two options the beneficiaries choose—or if they choose to do
nothing extra (around 1% according to annual Medicare Trustees reports
over time), beneficiaries also have other healthcare-related costs.
These additional so-called out of pocket (OOP) costs can include
deductibles and co-pays; the costs of uncovered services—such as for
long-term custodial, dental, hearing, and vision care; the cost of
annual physical exams for those not on Part C health plans that include
physicals; and the costs related to basic Medicare's lifetime and
per-incident limits. Medicare is funded by a combination of a specific payroll tax, beneficiary premiums and surtaxes from beneficiaries, co-pays and deductibles, and general U.S. Treasury revenue.
Medicare is divided into four Parts. Medicare Part A covers
hospital (inpatient, formally admitted only), skilled nursing (only
after being formally admitted to a hospital for three days and not for
custodial care), and hospice services. Part B covers outpatient services
including some providers' services while inpatient at a hospital,
outpatient hospital charges, most provider office visits even if the
office is "in a hospital", and most professionally administered
prescription drugs. Part D covers mostly self-administered prescription
drugs. Part C is an alternative called Managed Medicare or Medicare
Advantage which allows patients to choose health plans with at least the
same service coverage as Parts A and B (and most often more), often the
benefits of Part D, and always an annual out-of-pocket spend limit
which A and B lack. A beneficiary must enroll in Parts A and B first
before signing up for Part C.
History
Lyndon B. Johnson signing the Medicare amendment. Former President Harry S. Truman (seated) and his wife, Bess, are on the far right.
Originally, the name "Medicare" in the United States referred to a
program providing medical care for families of people serving in the
military as part of the Dependents' Medical Care Act, which was passed
in 1956. President Dwight D. Eisenhower
held the first White House Conference on Aging in January 1961, in
which creating a health care program for social security beneficiaries
was proposed.
In July 1965, under the leadership of President Lyndon Johnson, Congress enacted Medicare under Title XVIII of the Social Security Act to provide health insurance to people age 65 and older, regardless of income or medical history. Johnson signed the Social Security Amendments of 1965 into law on July 30, 1965, at the Harry S. Truman Presidential Library in Independence, Missouri. Former President Harry S. Truman and his wife, former First Lady Bess Truman became the first recipients of the program.
Before Medicare was created, only approximately 60% of people over the
age of 65 had health insurance, with coverage often unavailable or
unaffordable to many others, as older adults paid more than three times
as much for health insurance as younger people. Many of this group
(about 20% of the total in 2015) became "dual eligible" for both
Medicare and Medicaid with the passing of the law. In 1966, Medicare
spurred the racial integration
of thousands of waiting rooms, hospital floors, and physician practices
by making payments to health care providers conditional on desegregation.
Medicare has been operating for just over a half-century and,
during that time, has undergone several changes. Since 1965, the
program's provisions have expanded to include benefits for speech,
physical, and chiropractic therapy in 1972. Medicare added the option of payments to health maintenance organizations (HMO) in the 1970s. The government added hospice benefits to aid elderly people on a temporary basis in 1982, and made this permanent in 1984. Congress further expanded Medicare in 2001 to cover younger people with amyotrophic lateral sclerosis
(ALS, or Lou Gehrig's disease). As the years progressed, Congress
expanded Medicare eligibility to younger people with permanent
disabilities who receive Social Security Disability Insurance (SSDI) payments and to those with end-stage renal disease (ESRD). The association with HMOs that began in the 1970s was formalized and expanded under President Bill Clinton
in 1997 as Medicare Part C (although not all Part C health plans
sponsors have to be HMOs, about 75% are). In 2003, under President George W. Bush, a Medicare program for covering almost all self-administered prescription drugs was passed (and went into effect in 2006) as Medicare Part D.
Administration
The Centers for Medicare and Medicaid Services (CMS), a component of the U.S. Department of Health and Human Services (HHS), administers Medicare, Medicaid, the Children's Health Insurance Program (CHIP), the Clinical Laboratory Improvement Amendments (CLIA), and parts of the Affordable Care Act (ACA) ("Obamacare"). Along with the Departments of Labor and Treasury, the CMS also implements the insurance reform provisions of the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and most aspects of the Patient Protection and Affordable Care Act of 2010 as amended. The Social Security Administration
(SSA) is responsible for determining Medicare eligibility, eligibility
for and payment of Extra Help/Low Income Subsidy payments related to
Parts C and D of Medicare, and collecting most premium payments for the
Medicare program.
The Chief Actuary of the CMS must provide accounting information
and cost-projections to the Medicare Board of Trustees to assist them in
assessing the program's financial health. The Trustees are required by
law to issue annual reports on the financial status of the Medicare
Trust Funds, and those reports are required to contain a statement of
actuarial opinion by the Chief Actuary.
Since the Medicare program began, the CMS (that was not always
the name of the responsible bureaucracy) has contracted with private
insurance companies to operate as intermediaries between the government
and medical providers to administer Part A and Part B benefits.
Contracted processes include claims and payment processing, call center
services, clinician enrollment, and fraud investigation. Beginning in
1997 and 2005, respectively, these Part A and B administrators (whose
contracts are bid out periodically), along with other insurance
companies and other companies or organizations (such as integrated
health delivery systems, unions and pharmacies), also began
administering Part C and Part D plans.
The Specialty Society Relative Value Scale Update Committee (or Relative Value Update Committee; RUC), composed of physicians associated with the American Medical Association,
advises the government about pay standards for Medicare patient
procedures performed by doctors and other professionals under Medicare
Part B.
A similar but different CMS process determines the rates paid for acute
care and other hospitals—including skilled nursing facilities—under
Medicare Part A. The rates paid for both Part A and Part B type services
under Part C are whatever is agreed upon between the sponsor and the
provider. The amounts paid for mostly self administered drugs under Part
D is whatever is agreed upon between the sponsor (almost always through
a pharmacy benefit manager also used in commercial insurance) and
pharmaceutical distributors and/or manufacturers.
The expenditures from the trust funds under Parts A and B are fee
for service whereas the expenditures from the trust funds under Parts C
and D are capitated. In particular, it is important to understand that
Medicare itself does not purchase either self- administered or
professionally administered drugs. In Part D, the Part D Trust Fund
helps beneficiaries purchase drug insurance. For Part B drugs, the trust
funds reimburses the professional that administers the drugs and allows
a mark up for that service.
Financing
Medicare has several sources of financing.
Part A's inpatient admitted hospital and skilled nursing coverage is largely funded by revenue from a 2.9% payroll tax
levied on employers and workers (each pay 1.45%). Until December 31,
1993, the law provided a maximum amount of compensation on which the
Medicare tax could be imposed annually, in the same way that the Social
Security payroll tax operates.
Beginning on January 1, 1994, the compensation limit was removed.
Self-employed individuals must pay the entire 2.9% tax on self-employed
net earnings (because they are both employee and employer), but they may
deduct half of the tax from the income in calculating income tax.
Beginning in 2013, the rate of Part A tax on earned income exceeding
$200,000 for individuals ($250,000 for married couples filing jointly)
rose to 3.8%, in order to pay part of the cost of the subsidies mandated
by the Affordable Care Act.
Parts B and D are partially funded by premiums paid by Medicare
enrollees and general U.S. Treasury revenue (to which Medicare
beneficiaries contributed and may still contribute). In 2006, a surtax
was added to Part B premium for higher-income seniors to partially fund
Part D. In the Affordable Care Act legislation of 2010, another surtax
was then added to Part D premium for higher-income seniors to partially
fund the Affordable Care Act and the number of Part B beneficiaries
subject to the 2006 surtax was doubled, also partially to fund PPACA.
Parts A and B/D use separate trust funds to receive and disburse
the funds mentioned above. The Medicare Part C program uses these same
two trust funds as well at a proportion determined by the CMS reflecting
that Part C beneficiaries are fully on Parts A and B of Medicare just
as all other beneficiaries, but that their medical needs are paid for
through a sponsor (most often an integrated health delivery system or
spin out) to providers rather than "fee for service" (FFS) through an
insurance company called a Medicare Administrative Contractor to
providers.
In 2018, Medicare spending was over $740 billion, about 3.7% of
U.S. gross domestic product and over 15% of total US federal spending.
Because of the two Trust funds and their differing revenue sources (one
dedicated and one not), the Trustees analyze Medicare spending as a
percent of GDP rather than versus the Federal budget.
Retirement of the Baby Boom
generation is projected by 2030 to increase enrollment to more than 80
million. In addition, the fact that the number of workers per enrollee
will decline from 3.7 to 2.4 and that overall health care costs in the nation
are rising pose substantial financial challenges to the program.
Medicare spending is projected to increase from just over $740 billion
in 2018 to just over $1.2 trillion by 2026, or from 3.7% of GDP to 4.7%.
Baby-boomers are projected to have longer life spans, which will add to
the future Medicare spending. The 2019 Medicare Trustees Report
estimates that spending as a percent of GDP will grow to 6% by 2043
(when the last of the baby boomers turns 80) and then flatten out to
6.5% of GDP by 2093. In response to these financial challenges, Congress
made substantial cuts to future payouts to providers (primarily acute
care hospitals and skilled nursing facilities) as part of PPACA in 2010
and the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and policymakers have offered many additional competing proposals to reduce Medicare costs further.
Cost reduction is influenced by factors including reduction in inappropriate and unnecessary care by evaluating evidence-based practices
as well as reducing the amount of unnecessary, duplicative, and
inappropriate care. Cost reduction may also be effected by reducing
medical errors, investment in healthcare information technology,
improving transparency of cost and quality data, increasing
administrative efficiency, and by developing both clinical/non-clinical
guidelines and quality standards.
Eligibility
In
general, all persons 65 years of age or older who have been legal
residents of the United States for at least five years are eligible for
Medicare. People with disabilities under 65 may also be eligible if they receive Social Security Disability Insurance (SSDI) benefits. Specific medical conditions may also help people become eligible to enroll in Medicare.
People qualify for Medicare coverage, and Medicare Part A premiums are entirely waived, if the following circumstances apply:
- They are 65 years or older and US citizens or have been permanent legal residents for five continuous years, and they or their spouse (or qualifying ex-spouse) has paid Medicare taxes for at least 10 years.
- or
- They are under 65, disabled, and have been receiving either Social Security SSDI benefits or Railroad Retirement Board disability benefits; they must receive one of these benefits for at least 24 months from date of entitlement (eligibility for first disability payment) before becoming eligible to enroll in Medicare.
- or
- They get continuing dialysis for end stage renal disease or need a kidney transplant.
Those who are 65 and older who choose to enroll in Part A Medicare
must pay a monthly premium to remain enrolled in Medicare Part A if they
or their spouse have not paid the qualifying Medicare payroll taxes.
People with disabilities
who receive SSDI are eligible for Medicare while they continue to
receive SSDI payments; they lose eligibility for Medicare based on
disability if they stop receiving SSDI. The coverage does not begin
until 24 month after the SSDI start date. The 24-month exclusion means
that people who become disabled must wait two years before receiving
government medical insurance, unless they have one of the listed
diseases. The 24-month period is measured from the date that an
individual is determined to be eligible for SSDI payments, not
necessarily when the first payment is actually received. Many new SSDI
recipients receive "back" disability pay, covering a period that usually
begins six months from the start of disability and ending with the
first monthly SSDI payment.
Some beneficiaries are dual-eligible. This means they qualify for both Medicare and Medicaid.
In some states for those making below a certain income, Medicaid will
pay the beneficiaries' Part B premium for them (most beneficiaries have
worked long enough and have no Part A premium), as well as some of their
out of pocket medical and hospital expenses.
Benefits and parts
Medicare cards
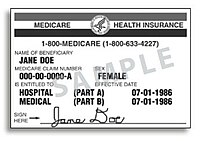
A sample of the Medicare card format used through 2018. The ID number is the subscriber's Social Security number, followed by a suffix indicating the holder's relationship to the subscriber (generally "A" for self). There are separate lines for basic Part A and Part B's supplementary medical coverage, each with its own start date.
A
sample of the new Medicare cards mailed out in 2018 and 2019 depending
on state of residence on a Social Security database. The new ID number
is randomly generated and not tied to any personally identifying
information.[23]
Beneficiaries on Medicare Part C health plans are issued with a
separate card and ID number, in addition to their Original Medicare
card.
Medicare has four parts: loosely speaking Part A is Hospital Insurance. Part B is Medical Services Insurance. Medicare Part D covers many prescription drugs,
though some are covered by Part B. In general, the distinction is based
on whether or not the drugs are self-administered but even this
distinction is not total. Public Part C Medicare health plans, the most
popular of which are branded Medicare Advantage, are another way for
Original Medicare (Part A and B) beneficiaries to receive their Part A, B
and D benefits; simply, Part C is capitated fee and Original Medicare
is fee for service. All Medicare benefits are subject to medical necessity.
The original program included Parts A and B. Part-C-like plans
have existed as demonstration projects in Medicare since the early
1970s, but the Part was formalized by 1997 legislation. Part D was
enacted by 2003 legislation and introduced January 1, 2006. Previously,
coverage for self-administered prescription drugs (if desired) was
obtained by private insurance or through a public Part C plan (or by one
of its predecessor demonstration plans before enactment).
In April 2018, CMS began mailing out new Medicare cards with new ID numbers to all beneficiaries. Previous cards had ID numbers containing beneficiaries' Social Security numbers; the new ID numbers are randomly generated and not tied to any other personally identifying information.
Part A: Hospital/hospice insurance
Part A covers inpatient hospital
stays where the beneficiary has been formally admitted to the hospital,
including semi-private room, food, and tests. As of January 1, 2020,
Medicare Part A had an inpatient hospital deductible of $1408,
coinsurance per day as $352 after 61 days confinement within one "spell
of illness", coinsurance for "lifetime reserve days" (essentially, days
91-150 of one or more stay of more than 60 days) of $704 per day. The
structure of coinsurance in a Skilled Nursing Facility (following a
medically necessary hospital confinement of 3 nights in row or more) is
different: zero for days 1-20; $167.50 per day for days 21-100. Many
medical services provided under Part A (e.g., some surgery in an acute
care hospital, some physical therapy in a skilled nursing facility) is
covered under Part B. These coverage amounts increase or decrease yearly
on 1st day of the year.
The maximum length of stay that Medicare Part A covers in a
hospital admitted inpatient stay or series of stays is typically 90
days. The first 60 days would be paid by Medicare in full, except one
copay (also and more commonly referred to as a "deductible") at the
beginning of the 60 days of $1340 as of 2018. Days 61–90 require a
co-payment of $335 per day as of 2018. The beneficiary is also allocated
"lifetime reserve days" that can be used after 90 days. These lifetime
reserve days require a copayment of $670 per day as of 2018, and the
beneficiary can only use a total of 60 of these days throughout their
lifetime.
A new pool of 90 hospital days, with new copays of $1340 in 2018 and
$335 per day for days 61–90, starts only after the beneficiary has 60
days continuously with no payment from Medicare for hospital or Skilled
Nursing Facility confinement.
Some "hospital services" are provided as inpatient services,
which would be reimbursed under Part A; or as outpatient services, which
would be reimbursed, not under Part A, but under Part B instead. The
"Two-Midnight Rule" decides which is which. In August 2013, the Centers for Medicare and Medicaid Services
announced a final rule concerning eligibility for hospital inpatient
services effective October 1, 2013. Under the new rule, if a physician
admits a Medicare beneficiary as an inpatient with an expectation that
the patient will require hospital care that "crosses two midnights",
Medicare Part A payment is "generally appropriate". However, if it is
anticipated that the patient will require hospital care for less than
two midnights, Medicare Part A payment is generally not appropriate;
payment such as is approved will be paid under Part B.
The time a patient spends in the hospital before an inpatient admission
is formally ordered is considered outpatient time. But, hospitals and
physicians can take into consideration the pre-inpatient admission time
when determining if a patient's care will reasonably be expected to
cross two midnights to be covered under Part A.
In addition to deciding which trust fund is used to pay for these
various outpatient vs. inpatient charges, the number of days for which a
person is formally considered an admitted patient affects eligibility
for Part A skilled nursing services.
Medicare penalizes hospitals for readmissions.
After making initial payments for hospital stays, Medicare will take
back from the hospital these payments, plus a penalty of 4 to 18 times
the initial payment, if an above-average number of patients from the
hospital are readmitted within 30 days. These readmission penalties
apply after some of the most common treatments: pneumonia, heart failure, heart attack, COPD, knee replacement, hip replacement.
A study of 18 states conducted by the Agency for Healthcare Research
and Quality (AHRQ) found that 1.8 million Medicare patients aged 65 and
older were readmitted within 30 days of an initial hospital stay in
2011; the conditions with the highest readmission rates were congestive
heart failure, sepsis, pneumonia, and COPD and bronchiectasis.
The highest penalties on hospitals are charged after knee or hip replacements, $265,000 per excess readmission. The goals are to encourage better post-hospital care and more referrals to hospice and end-of-life care in lieu of treatment, while the effect is also to reduce coverage in hospitals that treat poor and frail patients. The total penalties for above-average readmissions in 2013 are $280 million, for 7,000 excess readmissions, or $40,000 for each readmission above the US average rate.
Part A fully covers brief stays for rehabilitation or convalescence in a skilled nursing facility and up to 100 days per medical necessity with a co-pay if certain criteria are met:
- A preceding hospital stay must be at least three days as an inpatient, three midnights, not counting the discharge date.
- The skilled nursing facility stay must be for something diagnosed during the hospital stay or for the main cause of hospital stay.
- If the patient is not receiving rehabilitation but has some other ailment that requires skilled nursing supervision (e.g., wound management) then the nursing home stay would be covered.
- The care being rendered by the nursing home must be skilled. Medicare part A does not pay for stays that only provide custodial, non-skilled, or long-term care activities, including activities of daily living (ADL) such as personal hygiene, cooking, cleaning, etc.
- The care must be medically necessary and progress against some set plan must be made on some schedule determined by a doctor.
The first 20 days would be paid for in full by Medicare with the
remaining 80 days requiring a co-payment of $167.50 per day as of 2018.
Many insurance
group retiree, Medigap and Part C insurance plans have a provision for
additional coverage of skilled nursing care in the indemnity insurance
policies they sell or health plans they sponsor. If a beneficiary uses
some portion of their Part A benefit and then goes at least 60 days
without receiving facility-based skilled services, the 90-day hospital
clock and 100-day nursing home clock are reset and the person qualifies
for new benefit periods.
Hospice benefits
are also provided under Part A of Medicare for terminally ill persons
with less than six months to live, as determined by the patient's
physician. The terminally ill person must sign a statement that hospice
care has been chosen over other Medicare-covered benefits, (e.g. assisted living or hospital care).
Treatment provided includes pharmaceutical products for symptom control
and pain relief as well as other services not otherwise covered by
Medicare such as grief counseling.
Hospice is covered 100% with no co-pay or deductible by Medicare Part A
except that patients are responsible for a copay for outpatient drugs
and respite care, if needed.
Part B: Medical insurance
Part
B medical insurance helps pay for some services and products not
covered by Part A, generally on an outpatient basis (but also when on an
unadmitted observation status in a hospital). Part B is optional. It is
often deferred if the beneficiary or his/her spouse is still working and
has group health coverage through that employer. There is a lifetime
penalty (10% per year on the premium) imposed for not enrolling in Part B
when first eligible.
Part B coverage begins once a patient meets his or her deductible
($183 for 2017), then typically Medicare covers 80% of the RUC-set rate
for approved services, while the remaining 20% is the responsibility of
the patient, either directly or indirectly by private group retiree or Medigap insurance.
Part B coverage includes outpatient physician services, visiting nurse, and other services such as x-rays, laboratory and diagnostic tests, influenza and pneumonia vaccinations, blood transfusions, renal dialysis, outpatient hospital procedures, limited ambulance transportation, immunosuppressive drugs for organ transplant recipients, chemotherapy, hormonal treatments such as Lupron,
and other outpatient medical treatments administered in a doctor's
office. It also includes chiropractic care. Medication administration is
covered under Part B if it is administered by the physician during an
office visit.
Part B also helps with durable medical equipment (DME), including but not limited to canes, walkers, lift chairs, wheelchairs, and mobility scooters for those with mobility impairments. Prosthetic devices such as artificial limbs and breast prosthesis following mastectomy, as well as one pair of eyeglasses following cataract surgery, and oxygen for home use are also covered.
Complex rules control Part B benefits, and periodically issued
advisories describe coverage criteria. On the national level these
advisories are issued by CMS, and are known as National Coverage
Determinations (NCD). Local Coverage Determinations (LCD) apply within
the multi-state area managed by a specific regional Medicare Part B
contractor (which is an insurance company), and Local Medical Review
Policies (LMRP) were superseded by LCDs in 2003. Coverage information is
also located in the CMS Internet-Only Manuals (IOM), the Code of Federal Regulations (CFR), the Social Security Act, and the Federal Register.
The Monthly Premium for Part B for 2019 is $135.50 per month but
anyone on Social Security in 2019 is "held harmless" from that amount if
the increase in their SS monthly benefit does not cover the increase in
their Part B premium from 2019 to 2020. This hold harmless provision is
significant in years when SS does not increase but that is not the case
for 2020. There are additional income-weighted surtaxes for those with
incomes more than $85,000 per annum.
Part C: Medicare Advantage plans
With the passage of the Balanced Budget Act of 1997, Medicare beneficiaries were formally given the option to receive their Original Medicare benefits through capitated health insurance
Part C health plans, instead of through the Original fee for service
Medicare payment system. Many had previously had that option via a
series of demonstration projects that dated back to the early 1970s.
These Part C plans were initially known in 1997 as "Medicare+Choice". As
of the Medicare Modernization Act of 2003, most "Medicare+Choice" plans were re-branded as "Medicare Advantage"
(MA) plans (though MA is a government term and might not even be
"visible" to the Part C health plan beneficiary). Other plan types, such
as 1876 Cost plans, are also available in limited areas of the country.
Cost plans are not Medicare Advantage plans and are not capitated.
Instead, beneficiaries keep their Original Medicare benefits while their
sponsor administers their Part A and Part B benefits. The sponsor of a
Part C plan could be an integrated health delivery system or spin-out, a
union, a religious organization, an insurance company or other type of
organization.
Public Part C Medicare Advantage and other Part C health plans
are required to offer coverage that meets or exceeds the standards set
by Original Medicare but they do not have to cover every benefit in the
same way (the plan must be actuarially equivalent to Original Medicare
benefits). After approval by the Centers for Medicare and Medicaid
Services, if a Part C plan chooses to cover less than Original Medicare
for some benefits, such as Skilled Nursing Facility care, the savings
may be passed along to consumers by offering even lower co-payments for
doctor visits (or any other plus or minus aggregation approved by CMS).
Original "fee-for-service"
Medicare Parts A and B have a standard benefit package that covers
medically necessary care as described in the sections above that members
can receive from nearly any hospital or doctor in the country (if that
doctor or hospital accepts Medicare). Original Medicare beneficiaries
who choose to enroll in a Part C Medicare Advantage or other Part C
health plan instead give up none of their rights as an Original Medicare
beneficiary, receive the same standard benefits—as a minimum—as
provided in Original Medicare, and get an annual out of pocket (OOP)
upper spending limit not included in Original Medicare. However they
must typically use only a select network of providers except in
emergencies or for urgent care while travelling, typically restricted to
the area surrounding their legal residence (which can vary from tens to
over 100 miles depending on county). Most Part C plans are traditional health maintenance organizations (HMOs) that require the patient to have a primary care physician, though others are preferred provider organizations
(which typically means the provider restrictions are not as confining
as with an HMO). Others are hybrids of HMO and PPO called HMO-POS (for
point of service) and a few public Part C health plans are actually fee
for service hybrids.
Public Part C Medicare Advantage health plan members typically
also pay a monthly premium in addition to the Medicare Part B premium to
cover items not covered by traditional Medicare (Parts A & B), such
as the OOP limit, self-administered prescription drugs, dental care,
vision care, annual physicals, coverage outside the United States, and
even gym or health club memberships as well as—and probably most
importantly—reduce the 20% co-pays and high deductibles associated with
Original Medicare.
But in some situations the benefits are more limited (but they can
never be more limited than Original Medicare and must always include an
OOP limit) and there is no premium. The OOP limit can be as low as $1500
and as high as but no higher than $6700. In some cases, the sponsor
even rebates part or all of the Part B premium, though these types of
Part C plans are becoming rare.
Before 2003 Part C plans tended to be suburban HMOs tied to major
nearby teaching hospitals that cost the government the same as or even
5% less on average than it cost to cover the medical needs of a
comparable beneficiary on Original Medicare. The 2003-law payment
framework/bidding/rebate formulas overcompensated some Part C plan
sponsors by 7 percent (2009) on average nationally compared to what
Original Medicare beneficiaries cost per person on average nationally
that year and as much as 5 percent (2016) less nationally in other years
(see any recent year's Medicare Trustees Report, Table II.B.1).
The 2003 payment formulas succeeded in increasing the percentage
of rural and inner city poor that could take advantage of the OOP limit
and lower co-pays and deductibles—as well as the coordinated medical
care—associated with Part C plans. In practice however, one set of
Medicare beneficiaries received more benefits than others. The MedPAC
Congressional advisory group found in one year the comparative
difference for "like beneficiaries" was as high as 14% and have tended
to average about 2% higher.
The word "like" in the previous sentence is key. MedPAC does not
include all beneficiaries in its comparisons and MedPAC will not define
what it means by "like" but it apparently includes people who are only
on Part A, which severely skews its percentage comparisons—see January
2017 MedPAC meeting presentations. The differences caused by the
2003-law payment formulas were almost completely eliminated by PPACA and
have been almost totally phased out according to the 2018 MedPAC annual
report, March 2018. One remaining special-payment-formula
program—designed primarily for unions wishing to sponsor a Part C
plan—is being phased out beginning in 2017. In 2013 and since, on
average a Part C beneficiary cost the Medicare Trust Funds 2%-5% less
than a beneficiary on traditional fee for service Medicare, completely
reversing the situation in 2006-2009 right after implementation of the
2003 law and restoring the capitated fee vs fee for service funding
balance to its original intended parity level.
The intention of both the 1997 and 2003 law was that the
differences between fee for service and capitated fee beneficiaries
would reach parity over time and that has mostly been achieved, given
that it can never literally be achieved without a major reform of
Medicare because the Part C capitated fee in one year is based on the
fee for service spending the previous year.
Enrollment in public Part C health plans, including Medicare
Advantage plans, grew from about 1% of total Medicare enrollment in 1997
when the law was passed (the 1% representing people on pre-law
demonstration programs) to about 37% in 2019. Of course the absolute
number of beneficiaries on Part C has increased even more dramatically
on a percentage basis because of the large increase of people on
Original Medicare since 1997. Almost all Medicare beneficiaries have
access to at least two public Medicare Part C plans; most have access to
three or more.
Part D: Prescription drug plans
Medicare Part D
went into effect on January 1, 2006. Anyone with Part A or B is
eligible for Part D, which covers mostly self-administered drugs. It was
made possible by the passage of the Medicare Modernization Act
of 2003. To receive this benefit, a person with Medicare must enroll in
a stand-alone Prescription Drug Plan (PDP) or public Part C health plan
with integrated prescription drug coverage (MA-PD). These plans are
approved and regulated by the Medicare program, but are actually
designed and administered by various sponsors including charities,
integrated health delivery systems, unions and health insurance
companies; almost all these sponsors in turn use pharmacy benefit
managers in the same way as they are used by sponsors of health
insurance for those not on Medicare. Unlike Original Medicare (Part A
and B), Part D coverage is not standardized (though it is highly
regulated by the Centers for Medicare and Medicaid Services). Plans
choose which drugs they wish to cover (but must cover at least two drugs
in 148 different categories and cover all or "substantially all" drugs
in the following protected classes of drugs: anti-cancer;
anti-psychotic; anti-convulsant, anti-depressants, immuno-suppressant,
and HIV and AIDS drugs). The plans can also specify with CMS approval at
what level (or tier) they wish to cover it, and are encouraged to use step therapy.
Some drugs are excluded from coverage altogether and Part D plans that
cover excluded drugs are not allowed to pass those costs on to Medicare,
and plans are required to repay CMS if they are found to have billed
Medicare in these cases.
Under the 2003 law that created Medicare Part D, the Social
Security Administration offers an Extra Help program to lower-income
seniors such that they have almost no drug costs; in addition
approximately 25 states offer additional assistance on top of Part D.
For beneficiaries who are dual-eligible (Medicare and Medicaid eligible)
Medicaid may pay for drugs not covered by Part D of Medicare. Most of
this aid to lower-income seniors was available to them through other
programs before Part D was implemented.
Coverage by beneficiary spending is broken up into four phases:
deductible, initial spend, gap (infamously called the "donut hole"), and
catastrophic. Under a CMS template, there is usually a $100 or so
deductible before benefits commence (maximum of $415 in 2019) followed
by the initial spend phase where the templated co-pay is 25%, followed
by gap phase (where originally the templated co-pay was 100% but that
will fall to 25% in 2020 for all drugs), followed by the catastrophic
phase with a templated co-pay of about 5%. The beneficiaries' OOP spend
amounts vary yearly but are approximately as of 2018 $1000 in the
initial spend phase and $3000 to reach the catastrophic phase. This is
just a template and about half of all Part D plans differ (for example,
no initial deductible, better coverage in the gap) with permission of
CMS, which it typically grants as long as the sponsor provides at least
the actuarial equivalent value.
Out-of-pocket costs
No
part of Medicare pays for all of a beneficiary's covered medical costs
and many costs and services are not covered at all. The program contains
premiums, deductibles and coinsurance, which the covered individual must pay out-of-pocket. A study published by the Kaiser Family Foundation in 2008 found the Fee-for-Service Medicare benefit package was less generous than either the typical large employer preferred provider organization plan or the Federal Employees Health Benefits Program Standard Option.
Some people may qualify to have other governmental programs (such as
Medicaid) pay premiums and some or all of the costs associated with
Medicare.
Premiums
Most
Medicare enrollees do not pay a monthly Part A premium, because they (or
a spouse) have had 40 or more 3-month quarters in which they paid Federal Insurance Contributions Act
taxes. The benefit is the same no matter how much or how little the
beneficiary paid as long as the minimum number of quarters is reached.
Medicare-eligible persons who do not have 40 or more quarters of
Medicare-covered employment may buy into Part A for an annual adjusted
monthly premium of:
- $248.00 per month (as of 2012) for those with 30–39 quarters of Medicare-covered employment, or
- $451.00 per month (as of 2012) for those with fewer than 30 quarters of Medicare-covered employment and who are not otherwise eligible for premium-free Part A coverage.
Most Medicare Part B enrollees pay an insurance premium for this coverage; the standard Part B premium for 2019 is $135.50 a month. A new income-based premium surtax schema
has been in effect since 2007, wherein Part B premiums are higher for
beneficiaries with incomes exceeding $85,000 for individuals or $170,000
for married couples. Depending on the extent to which beneficiary
earnings exceed the base income, these higher Part B premiums are from
30% to 70% higher with the highest premium paid by individuals earning
more than $214,000, or married couples earning more than $428,000.
Medicare Part B premiums are commonly deducted automatically from
beneficiaries' monthly Social Security deposits. They can also be paid
quarterly via bill sent directly to beneficiaries or via deduction from a
bank account. These alternatives are becoming more common because
whereas the eligibility age for Medicare has remained at 65 per the 1965
legislation, the so-called Full Retirement Age for Social Security has
been increased to over 66 and will go even higher over time. Therefore,
many people delay collecting Social Security but join Medicare at 65 and
have to pay their Part B premium directly.
If you have higher income, you will pay an additional premium
amount for Medicare Part B and Medicare prescription drug coverage. The
additional amount is called the income-related monthly adjustment
amount. (IRMAA)
• Part B - For most beneficiaries, the government pays a
substantial portion — about 75 percent — of the Part B premium, and the
beneficiary pays the remaining 25 percent. If you are a higher-income
beneficiary, you will pay a larger percentage of the total cost of Part B
based on the income you report to the Internal Revenue Service (IRS).
You will pay monthly Part B premiums equal to 35, 50, 65, 80, or 85
percent of the total cost, depending on what you report to the IRS (for
2020, that would be on your 2018 tax return).
• Part D - If you are a higher-income beneficiary with Medicare
prescription drug coverage, you will pay monthly premiums plus an
additional amount, which is based on what you report to the IRS (for
2020, that would be on your 2018 tax return).
If you filed as: With Modified Adjusted Gross Income of : Part B IRMAA Part D IRMAA
Single, Head $87,000.01 - $109,000.00 $ 57.80 $12.20
of Household, $109,000.01 - $136,000.00 $144.60 $31.50
or Qualifying $136,000.01 - $163,000.00 $231.40 $50.70
Widow(er) $163,000.01 - $499,999.99 $318.10 $70.00
More than $499,999.99 $347.00 $76.40
Married, filing $174,000.01 - $218,000.00 $57.80 $12.20
Jointly $218,000.01 - $272,000.00 $144.60 $31.50
$272,000.01 - $326,000.00 $231.40 $50.70
$326,000.01 - $749,999.99 $318.10 $70.00
More than $749,999.99 $347.00 $76.40
Married, filing $87,000.01 - $412,999.99 $318.10 $70.00
Separately More than $412,999.99 $347.00 $76.40
Part C plans may or may not charge premiums (almost all do),
depending on the plans' designs as approved by the Centers for Medicare
and Medicaid Services. Part D premiums vary widely based on the benefit
level.
Deductible and coinsurance
Part A—For each benefit period, a beneficiary pays an annually adjusted:
- A Part A deductible of $1,288 in 2016 and $1,316 in 2017 for a hospital stay of 1–60 days.
- A $322 per day co-pay in 2016 and $329 co-pay in 2017 for days 61–90 of a hospital stay.
- A $644 per day co-pay in 2016 and $658 co-pay in 2017 for days 91–150 of a hospital stay, as part of their limited Lifetime Reserve Days.
- All costs for each day beyond 150 days
- Coinsurance for a Skilled Nursing Facility is $161 per day in 2016 and $164.50 in 2017 for days 21 through 100 for each benefit period (no co-pay for the first 20 days).
- A blood deductible of the first 3 pints of blood needed in a calendar year, unless replaced. There is a 3-pint blood deductible for both Part A and Part B, and these separate deductibles do not overlap.
Part B—After beneficiaries meet the yearly deductible of $183.00
for 2017, they will be required to pay a co-insurance of 20% of the
Medicare-approved amount for all services covered by Part B with the
exception of most lab services, which are covered at 100%. Previously,
outpatient mental health services was covered at 50%, but under the Medicare Improvements for Patients and Providers Act of 2008, it gradually decreased over several years and now matches the 20% required for other services. They are also required to pay an excess charge of 15% for services rendered by physicians who do not accept assignment.
The deductibles, co-pays, and coinsurance charges for Part C and D
plans vary from plan to plan. All Part C plans include an annual out of
pocket (OOP) upper spend limit. Original Medicare does not include an
OOP limit.
Medicare supplement (Medigap) policies
Of the Medicare beneficiaries who are not dual eligible for both
Medicare (around 10% are fully dual eligible) and Medicaid or that do
not receive group retirement insurance via a former employer (about 30%)
or do not choose a public Part C Medicare health plan (about 35%) or
who are not otherwise insured (about 5%—e.g., still working and
receiving employer insurance, on VA, etc.), almost all the remaining
elect to purchase a type of private supplemental indemnity insurance
policy called a Medigap plan (about 20%), to help fill in the financial
holes in Original Medicare (Part A and B) in addition to public Part D.
Note that the percentages add up to over 100% because many beneficiaries
have more than one type of additional protection on top of Original
Medicare.
These Medigap insurance policies are standardized by CMS, but are
sold and administered by private companies. Some Medigap policies sold
before 2006 may include coverage for prescription drugs. Medigap
policies sold after the introduction of Medicare Part D on January 1,
2006 are prohibited from covering drugs. Medicare regulations prohibit a
Medicare beneficiary from being sold both a public Part C Medicare
health plan and a private Medigap Policy. As with public Part C health
plans, private Medigap policies are only available to beneficiaries who
are already signed up for Original Medicare Part A and Part B. These
policies are regulated by state insurance departments rather than the
federal government although CMS outlines what the various Medigap plans
must cover at a minimum. Therefore, the types and prices of Medigap
policies vary widely from state to state and the degree of underwriting,
discounts for new members, and open enrollment and guaranteed issue
rules also varies widely from state to state.
As of 2016, 11 policies are currently sold—though few are
available in all states, and some are not available at all in
Massachusetts, Minnesota and Wisconsin (although these states have
analogs to the lettered Medigap plans). These plans are standardized
with a base and a series of riders. These are Plan A, Plan B, Plan C,
Plan D, Plan F, High Deductible Plan F, Plan G, Plan K, Plan L, Plan M,
and Plan N. Cost is usually the only difference between Medigap policies
with the same letter sold by different insurance companies in the same
state. Unlike public Part C Medicare health Plans, Medigap plans have no
networks, and any provider who accepts Original Medicare must also
accept Medigap.
All insurance companies that sell Medigap policies are required
to make Plan A available, and if they offer any other policies, they
must also make either Plan C or Plan F available as well, though Plan F
is scheduled to sunset in the year 2020. Anyone who currently has a Plan F may keep it.
Many of the insurance companies that offer Medigap insurance policies
also sponsor Part C health plans but most Part C health plans are
sponsored by integrated health delivery systems and their spin-offs,
charities, and unions as opposed to insurance companies. The leading
sponsor of both public Part C health plans and private Medigap plans is AARP.
Payment for services
Medicare
contracts with regional insurance companies to process over one billion
fee-for-service claims per year. In 2008, Medicare accounted for 13%
($386 billion) of the federal budget.
In 2016 it is projected to account for close to 15% ($683 billion) of
the total expenditures. For the decade 2010–2019 Medicare is projected
to cost 6.4 trillion dollars.
Reimbursement for Part A services
For institutional care, such as hospital and nursing home care, Medicare uses prospective payment systems.
In a prospective payment system, the health care institution receives a
set amount of money for each episode of care provided to a patient,
regardless of the actual amount of care. The actual allotment of funds
is based on a list of diagnosis-related groups
(DRG). The actual amount depends on the primary diagnosis that is
actually made at the hospital. There are some issues surrounding
Medicare's use of DRGs because if the patient uses less care, the
hospital gets to keep the remainder. This, in theory, should balance the
costs for the hospital. However, if the patient uses more care, then
the hospital has to cover its own losses. This results in the issue of
"upcoding", when a physician makes a more severe diagnosis to hedge
against accidental costs.
Reimbursement for Part B services
Payment
for physician services under Medicare has evolved since the program was
created in 1965. Initially, Medicare compensated physicians based on
the physician's charges, and allowed physicians to bill Medicare
beneficiaries the amount in excess of Medicare's reimbursement. In 1975,
annual increases in physician fees were limited by the Medicare
Economic Index (MEI). The MEI was designed to measure changes in costs
of physician's time and operating expenses, adjusted for changes in
physician productivity. From 1984 to 1991, the yearly change in fees was
determined by legislation. This was done because physician fees were
rising faster than projected.
The Omnibus Budget Reconciliation Act of 1989 made several
changes to physician payments under Medicare. Firstly, it introduced the
Medicare Fee Schedule, which took effect in 1992. Secondly, it limited
the amount Medicare non-providers could balance bill Medicare
beneficiaries. Thirdly, it introduced the Medicare Volume Performance
Standards (MVPS) as a way to control costs.
On January 1, 1992, Medicare introduced the Medicare Fee Schedule
(MFS), a list of about 7,000 services that can be billed for. Each
service is priced within the Resource-Based Relative Value Scale (RBRVS) with three Relative Value Units
(RVUs) values largely determining the price. The three RVUs for a
procedure are each geographically weighted and the weighted RVU value is
multiplied by a global Conversion Factor (CF), yielding a price in
dollars. The RVUs themselves are largely decided by a private group of
29 (mostly specialist) physicians—the American Medical Association's Specialty Society Relative Value Scale Update Committee (RUC).
From 1992 to 1997, adjustments to physician payments were
adjusted using the MEI and the MVPS, which essentially tried to
compensate for the increasing volume of services provided by physicians
by decreasing their reimbursement per service.
In 1998, Congress replaced the VPS with the Sustainable Growth Rate
(SGR). This was done because of highly variable payment rates under the
MVPS. The SGR attempts to control spending by setting yearly and
cumulative spending targets. If actual spending for a given year exceeds
the spending target for that year, reimbursement rates are adjusted
downward by decreasing the Conversion Factor (CF) for RBRVS RVUs.
In 2002, payment rates were cut by 4.8%. In 2003, payment rates
were scheduled to be reduced by 4.4%. However, Congress boosted the
cumulative SGR target in the Consolidated Appropriation Resolution of
2003 (P.L. 108-7), allowing payments for physician services to rise
1.6%. In 2004 and 2005, payment rates were again scheduled to be
reduced. The Medicare Modernization Act (P.L. 108-173) increased
payments 1.5% for those two years.
In 2006, the SGR mechanism was scheduled to decrease physician
payments by 4.4%. (This number results from a 7% decrease in physician
payments times a 2.8% inflation adjustment increase.) Congress overrode
this decrease in the Deficit Reduction Act (P.L. 109-362), and held
physician payments in 2006 at their 2005 levels. Similarly, another
congressional act held 2007 payments at their 2006 levels, and HR 6331
held 2008 physician payments to their 2007 levels, and provided for a
1.1% increase in physician payments in 2009. Without further continuing
congressional intervention, the SGR is expected to decrease physician
payments from 25% to 35% over the next several years.
MFS has been criticized for not paying doctors enough because of
the low conversion factor. By adjustments to the MFS conversion factor,
it is possible to make global adjustments in payments to all doctors.
The SGR was the subject of possible reform legislation again in 2014. On March 14, 2014, the United States House of Representatives passed the SGR Repeal and Medicare Provider Payment Modernization Act of 2014 (H.R. 4015; 113th Congress), a bill that would have replaced the (SGR) formula with new systems for establishing those payment rates. However, the bill would pay for these changes by delaying the Affordable Care Act's individual mandate requirement, a proposal that was very unpopular with Democrats.
The SGR was expected to cause Medicare reimbursement cuts of 24 percent
on April 1, 2014, if a solution to reform or delay the SGR was not
found. This led to another bill, the Protecting Access to Medicare Act of 2014 (H.R. 4302; 113th Congress), which would delay those cuts until March 2015. This bill was also controversial. The American Medical Association and other medical groups opposed it, asking Congress to provide a permanent solution instead of just another delay.
The SGR process was replaced by new rules as of the passage of MACRA in 2015.
Provider participation
There
are two ways for providers to be reimbursed in Medicare.
"Participating" providers accept "assignment", which means that they
accept Medicare's approved rate for their services as payment (typically
80% from Medicare and 20% from the beneficiary). Some non participating
doctors do not take assignment, but they also treat Medicare enrollees
and are authorized to balance bill no more than a small fixed amount
above Medicare's approved rate. A minority of doctors are "private
contractors" from a Medicare perspective, which means they opt out of
Medicare and refuse to accept Medicare payments altogether. These
doctors are required to inform patients that they will be liable for the
full cost of their services out-of-pocket, often in advance of
treatment.
While the majority of providers accept Medicare assignments, (97 percent for some specialties), and most physicians still accept at least some new Medicare patients, that number is in decline.
While 80% of physicians in the Texas Medical Association accepted new
Medicare patients in 2000, only 60% were doing so by 2012.
A study published in 2012 concluded that the Centers for Medicare and
Medicaid Services (CMS) relies on the recommendations of an American
Medical Association advisory panel. The study led by Dr. Miriam J.
Laugesen, of Columbia Mailman School of Public Health,
and colleagues at UCLA and the University of Illinois, shows that for
services provided between 1994 and 2010, CMS agreed with 87.4% of the
recommendations of the committee, known as RUC or the Relative Value
Update Committee.
Office medication reimbursement
Chemotherapy and other medications dispensed in a physician's office are reimbursed according to the Average Sales Price,
a number computed by taking the total dollar sales of a drug as the
numerator and the number of units sold nationwide as the denominator.
The current reimbursement formula is known as "ASP+6" since it
reimburses physicians at 106% of the ASP of drugs. Pharmaceutical
company discounts and rebates are included in the calculation of ASP,
and tend to reduce it. In addition, Medicare pays 80% of ASP+6, which is
the equivalent of 84.8% of the actual average cost of the drug. Some
patients have supplemental insurance or can afford the co-pay. Large
numbers do not. This leaves the payment to physicians for most of the
drugs in an "underwater" state. ASP+6 superseded Average Wholesale Price
in 2005, after a 2003 front-page New York Times article drew attention to the inaccuracies of Average Wholesale Price calculations.
This procedure is scheduled to change dramatically in 2017 under a CMS proposal that will likely be finalized in October 2016.
Medicare 10 percent incentive payments
"Physicians
in geographic Health Professional Shortage Areas (HPSAs) and Physician
Scarcity Areas (PSAs) can receive incentive payments from Medicare.
Payments are made on a quarterly basis, rather than claim-by-claim, and
are handled by each area's Medicare carrier."
Enrollment
Generally, if an individual already receives Social Security
payments, at age 65 the individual becomes automatically enrolled in
Medicare Part A (Hospital Insurance) and Medicare Part B (Medical
Insurance). If the individual chooses not to enroll in Part B (typically
because the individual is still working and receiving employer
insurance), then the individual must proactively opt out of it when
receiving the automatic enrollment package. Delay in enrollment in Part B
carries no penalty if the individual has other insurance (e.g. the
employment situation noted above), but may be penalized under other
circumstances. An individual who does not receive Social Security
benefits upon turning 65 must proactively join Medicare if they want it.
Penalties may apply if the individual chooses not to enroll at age 65
and does not have other insurance.
Parts A & B
Part A Late Enrollment Penalty
If
an individual is not eligible for premium-free Part A, and they do not
buy a premium-based Part A when they are first eligible, the monthly
premium may go up 10%.
The individual must pay the higher premium for twice the number of
years that they could have had Part A, but did not sign up. For example,
if they were eligible for Part A for two years but did not sign up,
they must pay the higher premium for four years. Usually, individuals do
not have to pay a penalty if they meet certain conditions that allow
them to sign up for Part A during a Special Enrollment Period.
Part B Late Enrollment Penalty
If
an individual does not sign up for Part B when they are first eligible,
they may have to pay a late enrollment penalty for as long as they have
Medicare. Their monthly premium for Part B may go up 10% for each full
12-month period that they could have had Part B, but did not sign up for
it. Usually, they do not pay a late enrollment penalty if they meet
certain conditions that allow them to sign up for Part B during a
special enrollment period.
Comparison with private insurance
Medicare differs from private insurance available to working Americans in that it is a social insurance
program. Social insurance programs provide statutorily guaranteed
benefits to the entire population (under certain circumstances, such as
old age or unemployment). These benefits are financed in significant
part through universal taxes. In effect, Medicare is a mechanism by
which the state takes a portion of its citizens' resources to provide
health and financial security to its citizens in old age or in case of
disability, helping them cope with the enormous, unpredictable cost of
health care. In its universality, Medicare differs substantially from
private insurers, which must decide whom to cover and what benefits to
offer to manage their risk pools and ensure that their costs do not
exceed premiums.
Because the federal government is legally obligated to provide
Medicare benefits to older and some disabled Americans, it cannot cut
costs by restricting eligibility or benefits, except by going through a
difficult legislative process, or by revising its interpretation of medical necessity.
By statute, Medicare may only pay for items and services that are
"reasonable and necessary for the diagnosis or treatment of illness or
injury or to improve the functioning of a malformed body member", unless
there is another statutory authorization for payment.
Cutting costs by cutting benefits is difficult, but the program can
also achieve substantial economies of scale in terms of the prices it
pays for health care and administrative expenses—and, as a result,
private insurers' costs have grown almost 60% more than Medicare's since
1970. Medicare's cost growth is now the same as GDP growth and expected to stay well below private insurance's for the next decade.
Because Medicare offers statutorily determined benefits, its
coverage policies and payment rates are publicly known, and all
enrollees are entitled to the same coverage. In the private insurance
market, plans can be tailored to offer different benefits to different
customers, enabling individuals to reduce coverage costs while assuming
risks for care that is not covered. Insurers, however, have far fewer
disclosure requirements than Medicare, and studies show that customers
in the private sector can find it difficult to know what their policy
covers, and at what cost.
Moreover, since Medicare collects data about utilization and costs for
its enrollees—data that private insurers treat as trade secrets—it gives
researchers key information about health care system performance.
Medicare also has an important role driving changes in the entire
health care system. Because Medicare pays for a huge share of health
care in every region of the country, it has a great deal of power to set
delivery and payment policies. For example, Medicare promoted the
adaptation of prospective payments based on DRG's, which prevents
unscrupulous providers from setting their own exorbitant prices. Meanwhile, the Patient Protection and Affordable Care Act
has given Medicare the mandate to promote cost-containment throughout
the health care system, for example, by promoting the creation of
accountable care organizations or by replacing fee-for-service payments
with bundled payments.
Costs and funding challenges
Medicare and Medicaid Spending as % GDP (2013)
Medicare spending as a percent of GDP
Medicare expenses and revenue
Over the long-term, Medicare faces significant financial challenges
because of rising overall health care costs, increasing enrollment as
the population ages, and a decreasing ratio of workers to enrollees.
Total Medicare spending is projected to increase from $523 billion in
2010 to around $900 billion by 2020. From 2010 to 2030, Medicare
enrollment is projected to increase dramatically, from 47 million to 79
million, and the ratio of workers to enrollees is expected to decrease
from 3.7 to 2.4.
However, the ratio of workers to retirees has declined steadily for
decades, and social insurance systems have remained sustainable due to
rising worker productivity. There is some evidence that productivity gains will continue to offset demographic trends in the near future.
The Congressional Budget Office
(CBO) wrote in 2008 that "future growth in spending per beneficiary for
Medicare and Medicaid—the federal government's major health care
programs—will be the most important determinant of long-term trends in
federal spending. Changing those programs in ways that reduce the growth
of costs—which will be difficult, in part because of the complexity of
health policy choices—is ultimately the nation's central long-term
challenge in setting federal fiscal policy."
Overall health care costs were projected in 2011 to increase by
5.8 percent annually from 2010 to 2020, in part because of increased
utilization of medical services, higher prices for services, and new
technologies.
Health care costs are rising across the board, but the cost of
insurance has risen dramatically for families and employers as well as
the federal government. In fact, since 1970 the per-capita cost of
private coverage has grown roughly one percentage point faster each year
than the per-capita cost of Medicare. Since the late 1990s, Medicare
has performed especially well relative to private insurers.
Over the next decade, Medicare's per capita spending is projected to
grow at a rate of 2.5 percent each year, compared to private insurance's
4.8 percent.
Nonetheless, most experts and policymakers agree containing health care
costs is essential to the nation's fiscal outlook. Much of the debate
over the future of Medicare revolves around whether per capita costs
should be reduced by limiting payments to providers or by shifting more
costs to Medicare enrollees.
Indicators
Several
measures serve as indicators of the long-term financial status of
Medicare. These include total Medicare spending as a share of gross domestic product (GDP), the solvency of the Medicare HI trust fund, Medicare per-capita spending growth relative to inflation
and per-capita GDP growth; general fund revenue as a share of total
Medicare spending; and actuarial estimates of unfunded liability over
the 75-year timeframe and the infinite horizon (netting expected
premium/tax revenue against expected costs). The major issue in all
these indicators is comparing any future projections against current law
vs. what the actuaries expect to happen. For example, current law
specifies that Part A payments to hospitals and skilled nursing
facilities will be cut substantially after 2028 and that doctors will
get no raises after 2025. The actuaries expect that the law will change
to keep these events from happening.
Medicare cost and non-interest income by source as a percentage of GDP
This measure, which examines Medicare spending in the context of the
US economy as a whole, is projected to increase from 3.7 percent in 2017
to 6.2 percent by 2092
under current law and over 9 percent under what the actuaries really
expect will happen (called an "illustrative example" in recent-year
Trustees Reports).
The solvency of the Medicare HI trust fund
This
measure involves only Part A. The trust fund is considered insolvent
when available revenue plus any existing balances will not cover 100
percent of annual projected costs. According to the latest estimate by
the Medicare trustees (2018), the trust fund is expected to become
insolvent in 8 years (2026), at which time available revenue will cover
around 85 percent of annual projected costs for Part A services. Since Medicare began, this solvency projection has ranged from two to 28 years, with an average of 11.3 years.
This and other projections in Medicare Trustees reports are based on
what its actuaries call intermediate scenario but the reports also
include worst-case and best case scenarios that are quite different
(other scenarios presume Congress will change present law).
Medicare per-capita spending growth relative to inflation and per-capita GDP growth
Per capita spending relative to inflation per-capita GDP growth was to be an important factor used by the PPACA-specified Independent Payment Advisory Board
(IPAB), as a measure to determine whether it must recommend to Congress
proposals to reduce Medicare costs. However the IPAB never formed and
was formally repealed by the Balanced Budget Act of 2018.
This measure, established under the Medicare Modernization Act
(MMA), examines Medicare spending in the context of the federal budget.
Each year, MMA requires the Medicare trustees to make a determination
about whether general fund revenue is projected to exceed 45 percent of
total program spending within a seven-year period. If the Medicare
trustees make this determination in two consecutive years, a "funding
warning" is issued. In response, the president must submit cost-saving
legislation to Congress, which must consider this legislation on an
expedited basis. This threshold was reached and a warning issued every
year between 2006 and 2013 but it has not been reached since that time
and is not expected to be reached in the 2016–2022 "window". This is a
reflection of the reduced spending growth mandated by the ACA according
to the Trustees.
Unfunded obligation
Medicare's
unfunded obligation is the total amount of money that would have to be
set aside today such that the principal and interest would cover the gap
between projected revenues (mostly Part B premiums and Part A payroll
taxes to be paid over the timeframe under current law) and spending over
a given timeframe. By law the timeframe used is 75 years though the
Medicare actuaries also give an infinite-horizon estimate because life
expectancy consistently increases and other economic factors underlying
the estimates change.
As of January 1, 2016, Medicare's unfunded obligation over the 75
year timeframe is $3.8 trillion for the Part A Trust Fund and $28.6
trillion for Part B. Over an infinite timeframe the combined unfunded
liability for both programs combined is over $50 trillion, with the
difference primarily in the Part B estimate.
These estimates assume that CMS will pay full benefits as currently
specified over those periods though that would be contrary to current
United States law. In addition, as discussed throughout each annual
Trustees' report, "the Medicare projections shown could be substantially
understated as a result of other potentially unsustainable elements of
current law." For example, current law effectively provides no raises
for doctors after 2025; that is unlikely to happen. It is impossible for
actuaries to estimate unfunded liability other than assuming current
law is followed (except relative to benefits as noted), the Trustees
state "that actual long-range present values for (Part A) expenditures
and (Part B/D) expenditures and revenues could exceed the amounts
estimated by a substantial margin."
Public opinion
Popular
opinion surveys show that the public views Medicare's problems as
serious, but not as urgent as other concerns. In January 2006, the Pew Research Center
found 62 percent of the public said addressing Medicare's financial
problems should be a high priority for the government, but that still
put it behind other priorities. Surveys suggest that there's no public consensus behind any specific strategy to keep the program solvent.
Fraud and waste
The Government Accountability Office
lists Medicare as a "high-risk" government program in need of reform,
in part because of its vulnerability to fraud and partly because of its
long-term financial problems. Fewer than 5% of Medicare claims are audited.
Criticism
Robert
M. Ball, a former commissioner of Social Security under President
Kennedy in 1961 (and later under Johnson, and Nixon) defined the major
obstacle to financing health insurance for the elderly: the high cost of
care for the aged combined with the generally low incomes of retired
people. Because retired older people use much more medical care than
younger employed people, an insurance premium related to the risk for
older people needed to be high, but if the high premium had to be paid
after retirement, when incomes are low, it was an almost impossible
burden for the average person. The only feasible approach, he said, was
to finance health insurance in the same way as cash benefits for
retirement, by contributions paid while at work, when the payments are
least burdensome, with the protection furnished in retirement without
further payment.
In the early 1960s relatively few of the elderly had health insurance,
and what they had was usually inadequate. Insurers such as Blue Cross, which had originally applied the principle of community rating,
faced competition from other commercial insurers that did not community
rate, and so were forced to raise their rates for the elderly.
Medicare is not generally an unearned entitlement. Entitlement is
most commonly based on a record of contributions to the Medicare fund.
As such it is a form of social insurance
making it feasible for people to pay for insurance for sickness in old
age when they are young and able to work and be assured of getting back
benefits when they are older and no longer working. Some people will pay
in more than they receive back and others will receive more benefits
than they paid in. Unlike private insurance where some amount must be
paid to attain coverage, all eligible persons can receive coverage
regardless of how much or if they had ever paid in.
Politicized payment
Bruce Vladeck, director of the Health Care Financing Administration in the Clinton
administration, has argued that lobbyists have changed the Medicare
program "from one that provides a legal entitlement to beneficiaries to
one that provides a de facto political entitlement to providers."
Quality of beneficiary services
A 2001 study by the Government Accountability Office
evaluated the quality of responses given by Medicare contractor
customer service representatives to provider (physician) questions. The
evaluators assembled a list of questions, which they asked during a
random sampling of calls to Medicare contractors. The rate of complete,
accurate information provided by Medicare customer service
representatives was 15%. Since then, steps have been taken to improve the quality of customer service given by Medicare contractors, specifically the 1-800-MEDICARE contractor. As a result, 1-800-MEDICARE
customer service representatives (CSR) have seen an increase in
training, quality assurance monitoring has significantly increased, and a
customer satisfaction survey is offered to random callers.
Hospital accreditation
In most states the Joint Commission, a private, non-profit organization
for accrediting hospitals, decides whether or not a hospital is able to
participate in Medicare, as currently there are no competitor
organizations recognized by CMS.
Other organizations can also accredit hospitals for Medicare. These include the Community Health Accreditation Program, the Accreditation Commission for Health Care, the Compliance Team and the Healthcare Quality Association on Accreditation.
Accreditation is voluntary and an organization may choose to be evaluated by their State Survey Agency or by CMS directly.
Graduate medical education
Medicare funds the vast majority of residency
training in the US. This tax-based financing covers resident salaries
and benefits through payments called Direct Medical Education payments.
Medicare also uses taxes for Indirect Medical Education, a subsidy paid
to teaching hospitals in exchange for training resident physicians. For the 2008 fiscal year these payments were $2.7 and $5.7 billion respectively.
Overall funding levels have remained at the same level since 1996, so
that the same number or fewer residents have been trained under this
program.
Meanwhile, the US population continues to grow both older and larger,
which has led to greater demand for physicians, in part due to higher
rates of illness and disease among the elderly compared to younger
individuals. At the same time the cost of medical services continue
rising rapidly and many geographic areas face physician shortages, both
trends suggesting the supply of physicians remains too low.
Medicare thus finds itself in the odd position of having assumed
control of the single largest funding source for graduate medical
education, currently facing major budget constraints, and as a result,
freezing funding for graduate medical education, as well as for
physician reimbursement rates. This has forced hospitals to look for
alternative sources of funding for residency slots.
This halt in funding in turn exacerbates the exact problem Medicare
sought to solve in the first place: improving the availability of
medical care. However, some healthcare administration experts believe
that the shortage of physicians may be an opportunity for providers to
reorganize their delivery systems to become less costly and more
efficient. Physician assistants and Advanced Registered Nurse
Practitioners may begin assuming more responsibilities that
traditionally fell to doctors, but do not necessarily require the
advanced training and skill of a physician.
Of the 35,476 total active applicants who participated in The
National Resident Matching Program in 2016, 75.6% (26,836) were able to
find PGY-1 (R-1)
matches. Out of the total active applicants, 51.27% (18,187) were
graduates of conventional US medical schools; 93.8% (17,057) were able
to find a match. In comparison, match rates were 80.3% of osteopathic
graduates, 53.9% of US citizen international medical school graduates,
and 50.5% of non-US citizen international medical schools graduates.
Legislation and reform
- 1960: PL 86-778 Social Security Amendments of 1960 (Kerr-Mills aid)
- 1965: PL 89-97 Social Security Act of 1965, Establishing Medicare Benefits
- 1980: Medicare Secondary Payer Act of 1980, prescription drugs coverage added
- 1988: PL 100-360 Medicare Catastrophic Coverage Act of 1988
- 1989: Medicare Catastrophic Coverage Repeal Act of 1989
- 1997: PL 105-33 Balanced Budget Act of 1997
- 2003: PL 108-173 Medicare Prescription Drug, Improvement, and Modernization Act
- 2010: Patient Protection and Affordable Care Act and Health Care and Education Reconciliation Act of 2010
- 2013: Sequestration effects on Medicare due to Budget Control Act of 2011
- 2015: Extensive changes to Medicare, primarily to the SGR provisions of the Balanced Budget Act of 1997 as part of the Medicare Access and CHIP Reauthorization Act (MACRA)
- 2016: Changes to the Social Security "hold harmless" laws as they affect Part B premiums based on the Bipartisan Budget Act of 2015
In 1977, the Health Care Financing Administration
(HCFA) was established as a federal agency responsible for the
administration of Medicare and Medicaid. This would be renamed to Centers for Medicare and Medicaid Services (CMS) in 2001. By 1983, the diagnosis-related group (DRG) replaced pay for service reimbursements to hospitals for Medicare patients.
President Bill Clinton attempted an overhaul of Medicare through his health care reform plan in 1993–1994 but was unable to get the legislation passed by Congress.
In 2003 Congress passed the Medicare Prescription Drug, Improvement, and Modernization Act, which President George W. Bush signed into law on December 8, 2003.
Part of this legislation included filling gaps in prescription-drug
coverage left by the Medicare Secondary Payer Act that was enacted in
1980. The 2003 bill strengthened the Workers' Compensation Medicare
Set-Aside Program (WCMSA) that is monitored and administered by CMS.
On August 1, 2007, the US House of Representatives voted to
reduce payments to Medicare Advantage providers in order to pay for
expanded coverage of children's health under the SCHIP
program. As of 2008, Medicare Advantage plans cost, on average, 13
percent more per person insured for like beneficiaries than direct
payment plans. Many health economists have concluded that payments to Medicare Advantage providers have been excessive.
The Senate, after heavy lobbying from the insurance industry, declined
to agree to the cuts in Medicare Advantage proposed by the House.
President Bush subsequently vetoed the SCHIP extension.
Effects of the Patient Protection and Affordable Care Act
The Patient Protection and Affordable Care Act
("PPACA") of 2010 made a number of changes to the Medicare program.
Several provisions of the law were designed to reduce the cost of
Medicare. The most substantial provisions slowed the growth rate of
payments to hospitals and skilled nursing facilities under Parts A of
Medicare, through a variety of methods (e.g., arbitrary percentage cuts,
penalties for readmissions).
Congress also attempted to reduce payments to public Part C
Medicare health plans by aligning the rules that establish Part C plans'
capitated fees more closely with the FFS paid for comparable care to
"similar beneficiaries" under Parts A and B of Medicare. Primarily these
reductions involved much discretion on the part of CMS and examples of
what CMS did included effectively ending a Part C program Congress had
previously initiated to increase the use of Part C in rural areas (the
so-called Part C PFFS plan) and reducing over time a program that
encouraged employers and unions to create their own Part C plans not
available to the general Medicare beneficiary base (so-called Part C
EGWP plans) by providing higher reimbursement. These two types of Part C
plans had been identified by MedPAC as the programs that most
negatively affected parity between the cost of Medicare beneficiaries on
Parts A/B/C and the costs of beneficiaries not on Parts A/B/C. These
efforts to reach parity have been more than successful. As of 2015, all
beneficiaries on A/B/C cost 4% less per person than all beneficiaries
not on A/B/C. But whether that is because the cost of the former
decreased or the cost of the latter increased is not known.
PPACA also slightly reduced annual increases in payments to
physicians and to hospitals that serve a disproportionate share of
low-income patients. Along with other minor adjustments, these changes
reduced Medicare's projected cost over the next decade by $455 billion.
Additionally, the PPACA created the Independent Payment Advisory Board
("IPAB"), which was empowered to submit legislative proposals to reduce
the cost of Medicare if the program's per-capita spending grows faster
than per-capita GDP plus one percent. The IPAB was never formed and was
formally repealed by the Balanced Budget Act of 2018.
The PPACA also made some changes to Medicare enrollee's'
benefits. By 2020, it will "close" the so-called "donut hole" between
Part D plans' initial spend phase coverage limits and the catastrophic
cap on out-of-pocket spending, reducing a Part D enrollee's' exposure to
the cost of prescription drugs by an average of $2,000 a year.
That is, the template co-pay in the gap (which legally still exists)
will be the same as the template co-pay in the initial spend phase, 25%.
This lowered costs for about 5% of the people on Medicare. Limits were
also placed on out-of-pocket costs for in-network care for public Part C
health plan enrollees.
Most of these plans had such a limit but ACA formalized the annual out
of pocket spend limit. Beneficiaries on traditional Medicare do not get
such a limit but can effectively arrange for one through private
insurance.
Meanwhile, Medicare Part B and D premiums were restructured in
ways that reduced costs for most people while raising contributions from
the wealthiest people with Medicare. The law also expanded coverage of or eliminated co-pays for some preventive services.
The PPACA instituted a number of measures to control Medicare
fraud and abuse, such as longer oversight periods, provider screenings,
stronger standards for certain providers, the creation of databases to
share data between federal and state agencies, and stiffer penalties for
violators. The law also created mechanisms, such as the Center for
Medicare and Medicaid Innovation to fund experiments to identify new
payment and delivery models that could conceivably be expanded to reduce
the cost of health care while improving quality.
Proposals for reforming Medicare
As
legislators continue to seek new ways to control the cost of Medicare, a
number of new proposals to reform Medicare have been introduced in
recent years.
Premium support
Since
the mid-1990s, there have been a number of proposals to change Medicare
from a publicly run social insurance program with a defined benefit,
for which there is no limit to the government's expenses, into a
publicly run health plan program that offers "premium support" for
enrollees.
The basic concept behind the proposals is that the government would
make a defined contribution, that is a premium support, to the health
plan of a Medicare enrollee's choice. Sponsors would compete to provide
Medicare benefits and this competition would set the level of fixed
contribution. Additionally, enrollees would be able to purchase greater
coverage by paying more in addition to the fixed government
contribution. Conversely, enrollees could choose lower cost coverage and
keep the difference between their coverage costs and the fixed
government contribution.
The goal of premium Medicare plans is for greater cost-effectiveness;
if such a proposal worked as planned, the financial incentive would be
greatest for Medicare plans that offer the best care at the lowest cost.
This concept is basically how public Medicare Part C already
works (but with a much more complicated competitive bidding process that
drives up costs for the Trustees, but is very advantageous to the
beneficiaries). Given that only about 1% of people on Medicare got
premium support when Aaron and Reischauer first wrote their proposal in
1995 and the percentage is now 35%, on the way to 50% by 2040 according
to the Trustees, perhaps no further reform is needed.
There have been a number of criticisms of the premium support
model. Some have raised concern about risk selection, where insurers
find ways to avoid covering people expected to have high health care
costs. Premium support proposals, such as the 2011 plan proposed by Senator Ron Wyden and Rep. Paul Ryan (R–Wis.),
have aimed to avoid risk selection by including protection language
mandating that plans participating in such coverage must provide
insurance to all beneficiaries and are not able to avoid covering higher
risk beneficiaries.
Some critics are concerned that the Medicare population, which has
particularly high rates of cognitive impairment and dementia, would have
a hard time choosing between competing health plans. Robert Moffit, a senior fellow of The Heritage Foundation
responded to this concern, stating that while there may be research
indicating that individuals have difficulty making the correct choice of
health care plan, there is no evidence to show that government
officials can make better choices.
Henry Aaron, one of the original proponents of premium supports, has
recently argued that the idea should not be implemented, given that Medicare Advantage
plans have not successfully contained costs more effectively than
traditional Medicare and because the political climate is hostile to the
kinds of regulations that would be needed to make the idea workable.
Currently public Part C Medicare health plans avoid this issue
with an indexed risk formula that provides lower per capita payments to
sponsors for relatively (remember all these people are over 65) healthy
plan members and higher per capita payments for less healthy members.
Raising the age of eligibility
A number of different plans have been introduced that would raise the age of Medicare eligibility.
Some have argued that, as the population ages and the ratio of workers
to retirees increases, programs for the elderly need to be reduced.
Since the age at which Americans can retire with full Social Security
benefits is rising to 67, it is argued that the age of eligibility for
Medicare should rise with it (though people can begin receiving reduced
Social Security benefits as early as age 62).
The CBO projected that raising the age of Medicare eligibility
would save $113 billion over 10 years after accounting for the necessary
expansion of Medicaid and state health insurance exchange subsidies
under health care reform, which are needed to help those who could not
afford insurance purchase it. The Kaiser Family Foundation
found that raising the age of eligibility would save the federal
government $5.7 billion a year, while raising costs for other payers.
According to Kaiser, raising the age would cost $3.7 billion to 65- and
66-year-olds, $2.8 billion to other consumers whose premiums would rise
as insurance pools absorbed more risk, $4.5 billion to employers
offering insurance, and $0.7 billion to states expanding their Medicaid
rolls. Ultimately Kaiser found that the plan would raise total social
costs by more than twice the savings to the federal government.
Negotiating the prices of prescription drugs
Currently,
people with Medicare can get prescription drug coverage through a
public Medicare Part C plan or through the standalone Part D
prescription drug plans (PDPs) program. Each plan sponsor establishes
its own coverage policies and could if desired independently negotiate
the prices it pays to drug manufacturers. But because each plan has a
much smaller coverage pool than the entire Medicare program, many argue
that this system of paying for prescription drugs undermines the
government's bargaining power and artificially raises the cost of drug
coverage. Conversely, negotiating for the sponsors is almost always done
by one of three or four companies typically tied to pharmacy retailers
each of whom alone has much more buying power than the entire Medicare
program. That pharmacy-centric vs. government-centric approach appears
to have worked given that Part D has come in at 50% or more under
original projected spending and has held average annual drug spending by
seniors in absolute dollars fairly constant for over 10 years.
Many look to the Veterans Health Administration
as a model of lower cost prescription drug coverage. Since the VHA
provides healthcare directly, it maintains its own formulary and
negotiates prices with manufacturers. Studies show that the VHA pays
dramatically less for drugs than the PDP plans Medicare Part D
subsidizes.
One analysis found that adopting a formulary similar to the VHA's would
save Medicare $14 billion a year (over 10 years the savings would be
around $140 billion).
There are other proposals for savings on prescription drugs that
do not require such fundamental changes to Medicare Part D's payment and
coverage policies. Manufacturers who supply drugs to Medicaid are
required to offer a 15 percent rebate on the average manufacturer's
price. Low-income elderly individuals who qualify for both Medicare and
Medicaid receive drug coverage through Medicare Part D, and no
reimbursement is paid for the drugs the government purchases for them.
Reinstating that rebate would yield savings of $112 billion, according
to a recent CBO estimate.
Some have questioned the ability of the federal government to achieve
greater savings than the largest PDPs, since some of the larger plans
have coverage pools comparable to Medicare's, though the evidence from
the VHA is promising. Some also worry that controlling the prices of
prescription drugs would reduce incentives for manufacturers to invest
in R&D, though the same could be said of anything that would reduce
costs. However the comparisons with the VHA point out that the VA only covers about half the drugs as Part D.
Reforming care for the "dual-eligibles"
Roughly nine million Americans—mostly older adults with low incomes—are eligible for both Medicare and Medicaid. These men and women tend to have particularly poor health—more than half are being treated for five or more chronic conditions—and high costs. Average annual per-capita spending for "dual-eligibles" is $20,000, compared to $10,900 for the Medicare population as a whole all enrollees.
The dual-eligible population comprises roughly 20 percent of Medicare's enrollees but accounts for 36 percent of its costs.
There is substantial evidence that these individuals receive highly
inefficient care because responsibility for their care is split between
the Medicare and Medicaid programs—most
see a number of different providers without any kind of mechanism to
coordinate their care, and they face high rates of potentially
preventable hospitalizations.
Because Medicaid and Medicare cover different aspects of health care,
both have a financial incentive to shunt patients into care the other
program pays for.
Many experts have suggested that establishing mechanisms to
coordinate care for the dual-eligibles could yield substantial savings
in the Medicare program, mostly by reducing hospitalizations. Such
programs would connect patients with primary care, create an
individualized health plan, assist enrollees in receiving social and
human services as well as medical care, reconcile medications prescribed
by different doctors to ensure they do not undermine one another, and
oversee behavior to improve health. The general ethos of these proposals is to "treat the patient, not the condition," and maintain health while avoiding costly treatments.
There is some controversy over who exactly should take
responsibility for coordinating the care of the dual eligibles. There
have been some proposals to transfer dual eligibles into existing
Medicaid managed care plans, which are controlled by individual states.
But many states facing severe budget shortfalls might have some
incentive to stint on necessary care or otherwise shift costs to
enrollees and their families to capture some Medicaid savings. Medicare
has more experience managing the care of older adults, and is already
expanding coordinated care programs under the ACA, though there are some questions about private Medicare plans' capacity to manage care and achieve meaningful cost savings.
Estimated savings from more effective coordinated care for the dual eligibles range from $125 billion to over $200 billion, mostly by eliminating unnecessary, expensive hospital admissions.
Both
House Republicans and President Obama proposed increasing the
additional premiums paid by the wealthiest people with Medicare,
compounding several reforms in the ACA that would increase the number of
wealthier individuals paying higher, income-related Part B and Part D
premiums. Such proposals are projected to save $20 billion over the
course of a decade,
and would ultimately result in more than a quarter of Medicare
enrollees paying between 35 and 90 percent of their Part B costs by
2035, rather than the typical 25 percent. If the brackets mandated for
2035 were implemented today,
it would mean that anyone earning more than $47,000 (as an individual)
or $94,000 (as a couple) would be affected. Under the Republican
proposals, affected individuals would pay 40 percent of the total Part B
and Part D premiums, which would be equivalent of $2,500 today.
More limited income-relation of premiums only raises limited
revenue. Currently, only 5 percent of Medicare enrollees pay an
income-related premium, and most only pay 35 percent of their total
premium, compared to the 25 percent most people pay. Only a negligible
number of enrollees fall into the higher income brackets required to
bear a more substantial share of their costs—roughly half a percent of
individuals and less than three percent of married couples currently pay
more than 35 percent of their total Part B costs.
There is some concern that tying premiums to income would weaken
Medicare politically over the long run, since people tend to be more
supportive of universal social programs than of means-tested ones.
Medigap restrictions
Some
Medicare supplemental insurance (or "Medigap") plans cover all of an
enrollee's cost-sharing, insulating them from any out-of-pocket costs
and guaranteeing financial security to individuals with significant
health care needs. Many policymakers believe that such plans raise the
cost of Medicare by creating a perverse incentive
that leads patients to seek unnecessary, costly treatments. Many argue
that unnecessary treatments are a major cause of rising costs and
propose that people with Medicare should feel more of the cost of their
care to create incentives to seek the most efficient alternatives.
Various restrictions and surcharges on Medigap coverage have appeared in
recent deficit reduction proposals.
One of the furthest-reaching reforms proposed, which would prevent
Medigap from covering any of the first $500 of coinsurance charges and
limit it to covering 50 percent of all costs beyond that, could save $50
billion over 10 years. But it would also increase health care costs substantially for people with costly health care needs.
There is some evidence that claims of Medigap's tendency to cause
over-treatment may be exaggerated and that potential savings from
restricting it might be smaller than expected.
Meanwhile, there are some concerns about the potential effects on
enrollees. Individuals who face high charges with every episode of care
have been shown to delay or forgo needed care, jeopardizing their health
and possibly increasing their health care costs down the line.
Given their lack of medical training, most patients tend to have
difficulty distinguishing between necessary and unnecessary treatments.
The problem could be exaggerated among the Medicare population, which
has low levels of health literacy.