Mental health in China is a growing issue. Experts have estimated that about 173 million people living in China are suffering from a mental disorder.
The desire to seek treatment is largely hindered by China's strict
social norms (and subsequent stigmas), as well as religious and cultural
beliefs regarding personal reputation and social harmony.
While the Chinese government is committed to expanding mental health
care services and legislation, the country struggles with a lack of
mental health professionals and access to specialists in rural areas.
History
China's first mental institutions were introduced before 1849 by Western missionaries. Missionary and doctor John G. Kerr
opened the first psychiatric hospital in 1898, with the goal of
providing care to people with mental health issues, and treating them in
a more humane way.
In 1949, the country began developing its mental health resources
by building psychiatric hospitals and facilities for training mental
health professionals. However, many community programs were discontinued
during the Cultural Revolution.
In a meeting jointly held by Chinese ministries and the World Health Organization
in 1999, the Chinese government committed to creating a mental health
action plan and a national mental health law, among other measures to
expand and improve care.
The action plan, adopted in 2002, outlined China's priorities of
enacting legislation, educating its people on mental illness and mental
health resources, and developing a stable and comprehensive system of
care.
In 2000, the Minority Health Disparities Research and Education
Act was enacted. This act helped in raising national awareness on health
issues through research, health education, and data collection.
Since 2006, the government's 686 Program has worked to redevelop
community mental health programs and make these the primary resource,
instead of psychiatric hospitals, for people with mental illnesses.
These community programs make it possible for mental health care to
reach rural areas, and for people in these areas to become mental health
professionals. However, despite the improvement in access to
professional treatment, mental health specialists are still relatively
inaccessible to rural populations. The program also emphasizes
rehabilitation, rather than the management of symptoms.
In 2011, the legal institution of China's State Council published
a draft for a new mental health law, which includes new regulations
concerning the rights of patients to not to be hospitalized against
their will.
The draft law also promotes the transparency of patient treatment
management, as many hospitals were driven by financial motives and
disregarded patients' rights. The law, adopted in 2012, stipulates that a
qualified psychiatrist
must make the determination of mental illness; that patients can choose
whether to receive treatment in most cases; and that only those at risk
of harming themselves or others are eligible for compulsory inpatient
treatment. However, Human Rights Watch
has criticized the law. For example, although it creates some rights
for detained patients to request a second opinion from another state
psychiatrists and then an independent psychiatrist, there is no right to
a legal hearing such as a mental health tribunal and no guarantee of legal representation.
Since 1993, WHO has been collaborating with China in the development of a national mental health information system.
Current
Though
China continues to develop its mental health services, it continues to
have a large number of untreated and undiagnosed people with mental
illnesses. The aforementioned intense stigma associated with mental
illness, a lack of mental health professionals and specialists, and
culturally-specific expressions of mental illness may play a role in the
disparity.
Prevalence of mental disorders
Researchers estimate that roughly 173 million people in China have a mental disorder. Over 90 percent of people with a mental disorder have never been treated.
A lack of government data on mental disorders makes it difficult to
estimate the prevalence of specific mental disorders, as China has not
conducted a national psychiatric survey since 1993.
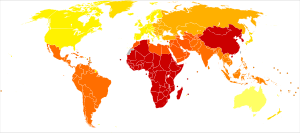
The map of disability-adjusted life years shows the disproportionate impact on the quality of life for persons with bipolar disorder in China and other East Asian countries.
Conducted
between 2001 and 2005, a non-governmental survey of 63,000 Chinese
adults found that 16 percent of the population had a mood disorder, including 6 percent of people with major depressive disorder. Thirteen percent of the population had an anxiety disorder and 9 percent had an alcohol use disorder.
Women were more likely to have a mood or anxiety disorder compared to
men, but men were significantly more likely to have an alcohol use
disorder. People living in rural areas were more likely to have major
depressive disorder or alcohol dependence.
In 2007, the Chief of China's National Centre for Mental Health,
Liu Jin, estimated that approximately 50 percent of outpatient
admissions were due to depression.
There is a disproportionate impact on the quality of life for people with bipolar disorder in China and other East Asian countries.
The suicide rate in China was approximately 23 per 100,000 people between 1995 and 1999.
Since then, the rate is thought to have fallen to roughly 7 per 100,000
people, according to government data. WHO states that the rate of
suicide is thought to be three to four times higher in rural areas than
in urban areas. The most common method, poisoning by pesticides,
accounts for 62 percent of incidences.
It is estimated that 18 percent of the Chinese population of over 244 million people believe in Buddhism. Another 22 percent of the population, roughly 294 million people believe in folk religions which are a group of beliefs that share characteristics with Confucianism, Buddhism, Taoism, and shamanism.
Common between all of these philosophical and religious beliefs is an
emphasis on acting harmoniously with nature, with strong morals, and
with a duty to family. Followers of these religions perceive behavior as
being tightly connected with health; illnesses are often thought to be a
result of moral failure or insufficiently honoring one's family in
current or past life. Furthermore, an emphasis on social harmony may
discourage people with mental illness from bringing attention to
themselves and seeking help. They may also refuse to speak about their
mental illness because of the shame it would bring upon themselves and
their family members, who could also be held responsible and experience
social isolation.
Also, reputation might be a factor that prevents individuals from seeking professional help. Good reputations
are highly valued. In a Chinese household, every individual shares the
responsibility of maintaining and raising the family's reputation. It is
believed that mental health will hinder individuals from achieving the
standards and goals- whether academic, social, career-based, or other-
expected from parents. Without reaching the expectations, individuals
are anticipated to bring shame to the family, which will affect the
family's overall reputation. Therefore, mental health issues are seen as
an unacceptable weakness. This perception of mental health disorders
causes individuals to internalize their mental health problems, possibly
worsening them, and making it difficult to seek treatment. Eventually,
it becomes ignored and overlooked by families.
In addition, many of these philosophies teach followers to accept one's fate.
Consequently, people with mental disorders may be less inclined to seek
medical treatment because they believe they should not actively try to
prevent any symptoms that may manifest. They may also be less likely to
question the stereotypes associated with people with mental illness, and
instead agreeing with others that they deserve to be ostracized.
Lack of qualified staff
China has 17,000 certified psychiatrists, which is 10 percent of that of other developed countries per capita.
China averages one psychologist for every 83,000 people, and some of
these psychologists are not board-licensed or certified to diagnose
illnesses. Individuals without any academic background in mental health
can obtain a license to counsel, following several months of training
through the National Exam for Psychological Counselors. Many psychiatrists or psychologists study psychology for personal use and do not intend to pursue a career in counseling.
Patients are likely to leave clinics with false diagnoses, and often do
not return for follow-up treatments, which is detrimental to the
degenerative nature of many psychiatric disorders.
The disparity between psychiatric services available between rural and urban areas partially contributes to this statistic, as rural areas have traditionally relied on barefoot doctors
since the 1970s for medical advice. These doctors are one of the few
modes of healthcare able to reach isolated parts of rural China, and are
unable to obtain modern medical equipment, and therefore, unable to
reliably diagnose psychiatric illnesses. Furthermore, the nearest
psychiatric clinic may be hundreds of miles away, and families may be
unable to afford professional psychiatric treatment for the afflicted.
Physical symptoms
Multiple
studies have found that Chinese patients with mental illness report
more physical symptoms compared to Western patients, who tend to report
more psychological symptoms.
For example, Chinese patients with depression are more likely to report
feelings of fatigue and muscle aches instead of feelings of depression.
However, it is unclear whether this occurs because they feel more
comfortable reporting physical symptoms or if depression manifests in a
more physical way among Chinese people.
Chinese Military Mental Health
Overview
Military
mental health has recently become an area of focus and improvement,
particularly in Western countries. For example, in the United States, it
is estimated that about twenty-five percent of active military members
suffer from a mental health problem, such as PTSD, Traumatic Brain
Injury, and depression.
Currently, there are no clear initiatives from the government about
mental health treatment towards military personnel in China.
Specifically, China has been investing in resources towards researching
and understanding how the mental health needs of military members and
producing policies to reinforce the research results.
Background
Research
on the mental health status of active Chinese military men began in the
1980s where psychologists investigated soldiers' experiences in the
plateaus.
The change of emphasis from physical to mental health can be seen in
China's four dominant military academic journals: First Military
Journal, Second Military Journal, Third Military Journal, and Fourth
Military Journal. In the 1980s, researchers mostly focused on the
physical health of soldiers; as the troops' ability to perform their
services declined, the government began looking at their mental health
to provide an explanation for this trend. In the 1990s, research on it
increased with the hope that by improving the mental health of soldiers,
combat effectiveness improves.
Mental health issue can impact active military members'
effectiveness in the army, and can create lasting effects on them after
they leave the military. Plateaus were an area of interest in this sense
because of harsh environmental conditions and the necessity of the
work done with low atmospheric pressure and intense UV radiation.
It was critical to place the military there to stabilize the outskirts
and protect the Chinese citizens who live nearby; this made it one of
the most important jobs in the army, then increasing the pressure on
those who worked in the plateaus. It not only affected the body
physically, like in the arteries, lungs, and back, but caused high
levels of depression in soldiers because of being away from family
members and with limited communication methods. Scientists found that
this may impact their lives as they saw that this population had higher
rates of divorce and unemployment.
Comparatively, assessing the mental health status of the People's
Liberation Army (PLA) is difficult, because military members work a
diverse array of duties over a large landscape. Military members also
play an active part in disaster relief, peacekeeping in foreign lands,
protecting borders, and domestic riot control. In a study of 11,000
soldiers, researchers found that those who work as peacekeepers have
higher levels of depression compared to those in the engineering and
medical departments.
With such diverse military roles over an area of 3.25 million miles, it
is difficult to gauge its impacts on soldiers’ psyche and provide a
single method to address mental health problems.
Researches have increased over the last two decades, but the
studies still lack a sense of comprehensiveness and reliability. In over
73 studies that together included 53,424 military members, some
research shows that there is gradual improvement in mental health at
high altitudes, such as mountain tops; other researchers found that depressive symptoms can worsen.
These research studies demonstrate how difficult it is to assess and
treat the mental illness that occurs in the army and how there are
inconsistent results. Studies of the military population focus on the
men of the military and exclude women, even though the number of women
that are joining the military has increased in the last two decades.
Chinese researchers try to provide solutions that are
preventative and reactive, such as implementing early mental health
training,
or mental health assessments to help service members understand their
mental health state, and how to combat these feelings themselves.
Researchers also suggest to improve the mental health of the military
members, programs should include psychoeducation, psychological
training, and attention to physical health to employ timely
intervention.
Implementation
In 2006, the People's Republic Minister for National Defense began
mental health vetting at the beginning of the military recruitment
process.
A Chinese military study consisting of 2500 male military personnel
found that some members are more predisposed to mental illness. The
study measured levels of anxious behaviors, symptoms of depression,
sensitivity to traumatic events, resilience and emotional intelligence
of existing personnel to aid the screening of new recruits.
Similar research has been conducted into the external factors that
impact a person's mental fortitude, including single-child status, urban
or rural environment, and education level. Subsequently, the government has incorporated mental illness coping techniques into their training manual. In 2013 leak by the Tibetan Center for Human Rights of a small portion of the People's Liberation Army
training manual from 2008, specifically concerned how military
personnel could combat PTSD and depression while on peacekeeping
missions in Tibet. The manual suggested that soldiers should:
“...close [their] eyes and imagine zooming in on the scene like a camera [when experiencing PTSD]. It may feel uncomfortable. Then zoom all the way out until you cannot see anything. Then tell yourself the flashback is gone.”
In
2012, the government specifically addressed military mental health in a
legal document for the first time. In article 84 of the Mental Health
Law of the People's Republic of China, it stated, “The State Council
and the Central Military Committee will formulate regulations based on
this law to manage mental health work in the military."
Besides screening, assessments and an excerpt of the manual, not
much is known about the services that are provided to active military
members and veterans. Analysis of more than 45 different studies,
moreover, has deemed that the level of anxiety in current and
ex-military personnel has increased despite efforts of the People's
Republic due to economic conditions, lack of social connects and the
feeling of a threat to military livelihood.
This growing anxiety manifested in both 2016 and 2018, as Chinese
veterans demonstrated their satisfaction with the system via protests
across China.
In both instances, veterans advocated for an increased focus on
post-service benefits, resources to aid in post-service jobs, and
justice for those who were treated poorly by the government.
As a way to combat the dissatisfaction of veterans and alleviate
growing tension, the government established the Ministry of Veteran
Affairs in 2018. At the same time, Xi Jinping, General Secretary of the Communist Party of China, promised to enact laws that protect the welfare of veterans.