| Vitamin B6 | |
|---|---|
| |
| Class identifiers | |
| Use | Vitamin B6 deficiency |
| ATC code | A11HA02 |
| Biological target | enzyme cofactor |
| Clinical data | |
| Drugs.com | International Drug Names |
| External links | |
| MeSH | D025101 |
Vitamin B6 refers to a group of chemically similar compounds which can be interconverted in biological systems. Vitamin B6 is part of the vitamin B group of essential nutrients. Its active form, pyridoxal 5′-phosphate, serves as a coenzyme in some 100 enzyme reactions in amino acid, glucose, and lipid metabolism.
Forms
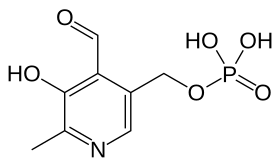
- Pyridoxine (PN), the form most commonly given as vitamin B6 supplement
- Pyridoxine 5′-phosphate (P5P)
- Pyridoxal (PL)
- Pyridoxal 5′-phosphate (PLP), the metabolically active form
- Pyridoxamine (PM)
- Pyridoxamine 5′-phosphate (PMP)
- 4-Pyridoxic acid (PA), the catabolite which is excreted in urine
- Pyritinol, a semi-synthetic derivative of pyridoxine, where two pyridoxine moieties are bound by a disulfide bridge.
All forms except pyridoxic acid and pyritinol can be interconverted. Absorbed pyridoxamine is converted to PMP by pyridoxal kinase, which is further converted to PLP by pyridoxamine-phosphate transaminase or pyridoxine 5′-phosphate oxidase which also catalyzes the conversion of PNP to PLP. Pyridoxine 5′-phosphate oxidase is dependent on flavin mononucleotide (FMN) as a cofactor produced from riboflavin (vitamin B2).
Functions
PLP, the metabolically active form of vitamin B6, is involved in many aspects of macronutrient metabolism, neurotransmitter synthesis, histamine synthesis, hemoglobin synthesis and function, and gene expression. PLP generally serves as a coenzyme (cofactor) for many reactions including decarboxylation, transamination, racemization, elimination, replacement, and beta-group interconversion. The liver is the site for vitamin B6 metabolism.
Amino acid metabolism
- PLP is a cofactor in the biosynthesis of five important neurotransmitters: serotonin, dopamine, epinephrine, norepinephrine, and gamma-aminobutyric acid (GABA). PLP is also involved in the synthesis of histamine.
- Transaminases break down amino acids with PLP as a cofactor. The proper activity of these enzymes is crucial for the process of moving amine groups from one amino acid to another.
- Serine racemase which synthesizes the neuromodulator d-serine from its enantiomer is a PLP-dependent enzyme.
- PLP is a coenzyme needed for the proper function of the enzymes cystathionine synthase and cystathionase. These enzymes catalyze reactions in the catabolism of methionine. Part of this pathway (the reaction catalyzed by cystathionase) also produces cysteine.
- Selenomethionine is the primary dietary form of selenium. PLP is needed as a cofactor for the enzymes that allow selenium to be used from the dietary form. PLP also plays a cofactor role in releasing selenium from selenohomocysteine to produce hydrogen selenide, which can then be used to incorporate selenium into selenoproteins.
- PLP is required for the conversion of tryptophan to niacin, so low vitamin B6 status impairs this conversion.
Glucose metabolism
PLP is a required coenzyme of glycogen phosphorylase, the enzyme necessary for glycogenolysis to occur. PLP can catalyze transamination reactions that are essential for providing amino acids as a substrate for gluconeogenesis.
Lipid metabolism
PLP is an essential component of enzymes that facilitate the biosynthesis of sphingolipids. Particularly, the synthesis of ceramide requires PLP. In this reaction, serine is decarboxylated and combined with palmitoyl-CoA to form sphinganine, which is combined with a fatty acyl-CoA to form dihydroceramide.
Dihydroceramide is then further desaturated to form ceramide. In
addition, the breakdown of sphingolipids is also dependent on vitamin B6 because sphingosine-1-phosphate lyase, the enzyme responsible for breaking down sphingosine-1-phosphate, is also PLP-dependent.
Hemoglobin synthesis and function
PLP aids in the synthesis of hemoglobin, by serving as a coenzyme for the enzyme ALA synthase. It also binds to two sites on hemoglobin to enhance the oxygen binding of hemoglobin.
Gene expression
PLP has been implicated in increasing or decreasing the expression of certain genes. Increased intracellular levels of the vitamin lead to a decrease in the transcription of glucocorticoids. Also, vitamin B6 deficiency leads to the increased gene expression of albumin mRNA. Also, PLP influences expression of glycoprotein IIb by interacting with various transcription factors. The result is inhibition of platelet aggregation.
Nutrition
Food sources
Vitamin B6 is widely distributed in foods in both its free and bound forms. Cooking, storage, and processing losses of vitamin B6 vary and in some foods may be more than 50%,
depending on the form of vitamin present in the food. Plant foods lose
the least during processing, as they contain mostly pyridoxine, which is
far more stable than the pyridoxal or pyridoxamine found in animal
foods. For example, milk can lose 30–70% of its vitamin B6 content when dried. Vitamin B6 is found in the germ and aleurone
layer of grains, and milling results in the reduction of this vitamin
in white flour. The heating that occurs before most freezing and canning
processes may also result in the loss of vitamin B6 in foods.
Foods that contain large amounts of vitamin B6 include:
Dietary recommendations
The U.S. Institute of Medicine (renamed National Academy of Medicine in 2015) updated Estimated Average Requirements (EARs) and Recommended Dietary Allowances (RDAs) for vitamin B6 in 1998. EARs for vitamin B6
for women and men ages 14 and up increase with age from 1.0 to
1.3 mg/day and from 1.1 to 1.4 mg/day, respectively; the RDAs increase
with age from 1.2 to 1.5 and from 1.3 to 1.7 mg/day, respectively. RDAs
are higher than EARs so as to identify amounts that will cover people
with higher than average requirements. RDA for pregnancy is 1.9 mg/day.
RDA for lactation is 2.0 mg/day. For infants up to 12 months the
Adequate Intake (AI) is 0.1–0.3 mg/day. and for children ages 1–13 years
the RDA increases with age from 0.5 to 1.0 mg/day. As for safety, Tolerable upper intake levels (ULs) for vitamins and minerals are identified when evidence is sufficient. In the case of vitamin B6 the UL is set at 100 mg/day. Collectively the EARs, RDAs, AIs and ULs are referred to as Dietary Reference Intakes (DRIs).
The European Food Safety Authority
(EFSA) refers to the collective set of information as Dietary Reference
Values, with Population Reference Intake (PRI) instead of RDA, and
Average Requirement instead of EAR. AI and UL defined the same as in
United States. For women and men ages 15 and older the PRI is set at 1.6
and 1.7 mg/day, respectively. AI for pregnancy is 1.8 mg/day, for
lactation 1.7 mg/day. For children ages 1–14 years the PRIs increase
with age from 0.6 to 1.4 mg/day. These PRIs are slightly higher than the
U.S. RDAs. The EFSA also reviewed the safety question and set its UL at 25 mg/day.
For U.S. food and dietary supplement labeling purposes the amount
in a serving is expressed as a percent of Daily Value (% DV). For
vitamin B6 labeling purposes 100% of the Daily Value was
2.0 mg, but as of May 27, 2016 it was revised to 1.7 mg to bring it into
agreement with the RDA. A table of the old and new adult Daily Values is provided at Reference Daily Intake. Food and supplement companies have until January 1, 2020 to comply with the change.
Absorption and excretion
Vitamin B6 is absorbed in the jejunum and ileum
by passive diffusion. With the capacity for absorption being so great,
animals are able to absorb quantities much greater than necessary for
physiological demands. The absorption of pyridoxal phosphate and
pyridoxamine phosphate involves their dephosphorylation catalyzed by a
membrane-bound alkaline phosphatase.
Those products and nonphosphorylated forms in the digestive tract are
absorbed by diffusion, which is driven by trapping of the vitamin as
5′-phosphates through the action of phosphorylation (by a pyridoxal
kinase) in the jejunal mucosa. The trapped pyridoxine and pyridoxamine
are oxidized to pyridoxal phosphate in the tissue.
The products of vitamin B6 metabolism are excreted in the urine, the major product of which is 4-pyridoxic acid. An estimated 40–60% of ingested vitamin B6 is oxidized to 4-pyridoxic acid. Several studies have shown that 4-pyridoxic acid is undetectable in the urine of vitamin B6-deficient subjects, making it a useful clinical marker to assess the vitamin B6 status of an individual. Other products of vitamin B6
metabolism excreted in the urine when high doses of the vitamin have
been given include pyridoxal, pyridoxamine, and pyridoxine and their
phosphates. A small amount of vitamin B6 is also excreted in the feces.
Deficiency
Signs and symptoms
The classic clinical syndrome for vitamin B6 deficiency is a seborrhoeic dermatitis-like eruption, atrophic glossitis with ulceration, angular cheilitis, conjunctivitis, intertrigo, and neurologic symptoms of somnolence, confusion, and neuropathy (due to impaired sphingosine synthesis) and sideroblastic anemia (due to impaired heme synthesis).
Less severe cases present with metabolic disease associated with insufficient activity of the coenzyme PLP. The most prominent of the lesions is due to impaired tryptophan–niacin conversion. This can be detected based on urinary excretion of xanthurenic acid after an oral tryptophan load. Vitamin B6 deficiency can also result in impaired transsulfuration of methionine to cysteine.
The PLP-dependent transaminases and glycogen phosphorylase provide the
vitamin with its role in gluconeogenesis, so deprivation of vitamin B6 results in impaired glucose tolerance.
Diagnosis
The assessment of vitamin B6 status is essential, as the clinical signs and symptoms in less severe cases are not specific.
The three biochemical tests most widely used are the activation
coefficient for the erythrocyte enzyme aspartate aminotransferase,
plasma PLP concentrations, and the urinary excretion of vitamin B6
degradation products, specifically urinary PA. Of these, plasma PLP is
probably the best single measure, because it reflects tissue stores.
Plasma PLP less than 10 nmol/l is indicative of vitamin B6 deficiency.
A PLP concentration greater than 20 nmol/l has been chosen as a level
of adequacy for establishing Estimated Average Requirements and
Recommended Daily Allowances in the USA. Urinary PA is also an indicator of vitamin B6 deficiency; levels of less than 3.0 mmol/day is suggestive of vitamin B6 deficiency.
The classic syndrome for vitamin B6 deficiency is
rare, even in developing countries. A handful of cases were seen between
1952 and 1953, particularly in the United States, and occurred in a
small percentage of infants who were fed a formula lacking in
pyridoxine.
Causes
A deficiency of vitamin B6 alone is relatively uncommon and often occurs in association with other vitamins of the B complex. The elderly and alcoholics have an increased risk of vitamin B6 deficiency, as well as other micronutrient deficiencies. Evidence exists for decreased levels of vitamin B6 in women with type 1 diabetes and in patients with systemic inflammation, liver disease, rheumatoid arthritis, and those infected with HIV. Use of oral contraceptives and treatment with certain anticonvulsants, isoniazid, cycloserine, penicillamine, and hydrocortisone negatively impact vitamin B6 status. Hemodialysis reduces vitamin B6 plasma levels.
Toxicity
Adverse effects have been documented from vitamin B6 supplements, but never from food sources. Damage to the dorsal root ganglia is documented in human cases of overdose of pyridoxine.
Although it is a water-soluble vitamin and is excreted in the urine,
doses of pyridoxine in excess of the dietary upper limit (UL) over long
periods cause painful and ultimately irreversible neurological problems.
The primary symptoms are pain and numbness of the extremities. In
severe cases, motor neuropathy may occur with "slowing of motor
conduction velocities, prolonged F wave latencies, and prolonged sensory
latencies in both lower extremities", causing difficulty in walking. Sensory neuropathy
typically develops at doses of pyridoxine in excess of 1,000 mg per
day, but adverse effects can occur with much less, so doses over 200 mg
are not considered safe. Symptoms among women taking lower doses have been reported.
Existing authorizations and valuations vary considerably
worldwide. As noted, the U.S. Institute of Medicine set an adult UL at
100 mg/day. The European Community Scientific Committee on Food defined intakes of 50 mg of vitamin B6 per day as harmful and established a UL of 25 mg/day.
The nutrient reference values in Australia and New Zealand recommend an
upper limit of 50 mg/day in adults. "The same figure was set for
pregnancy and lactation as there is no evidence of teratogenicity at
this level. The UL was set based on metabolic body size and growth
considerations for all other ages and life stages except infancy. It was
not possible to set a UL for infants, so intake is recommended in the
form of food, milk or formula." The ULs were set using results of
studies involving long-term oral administration of pyridoxine at doses
of less than 1 g/day. "A no-observed-adverse-effect level (NOAEL) of 200 mg/day was identified from the studies of Bernstein & Lobitz (1988) and Del Tredici et al
(1985). These studies involved subjects who had generally been on the
supplements for five to six months or less. The study of Dalton and
Dalton (1987), however, suggested the symptoms might take substantially
longer than this to appear. In this latter retrospective survey,
subjects who reported symptoms had been on supplements for 2.9 years, on
average. Those reporting no symptoms had taken supplements for 1.9
years."
History
In 1934, the Hungarian physician Paul György discovered a substance that was able to cure a skin disease in rats (dermatitis acrodynia). He named this substance vitamin B6. In 1938, Samuel Lepkovsky isolated vitamin B6
from rice bran. Harris and Folkers in 1939 determined the structure of
pyridoxine, and, in 1945, Snell was able to show the two forms of
vitamin B6, pyridoxal and pyridoxamine. Vitamin B6 was named pyridoxine to indicate its structural homology to pyridine.


