A spectrum disorder is a mental disorder that includes a range of linked conditions, sometimes also extending to include singular symptoms and traits.
The different elements of a spectrum either have a similar appearance
or are thought to be caused by the same underlying mechanism. In either
case, a spectrum approach is taken because there appears to be "not a
unitary disorder but rather a syndrome composed of subgroups". The spectrum may represent a range of severity, comprising relatively "severe" mental disorders through to relatively "mild and nonclinical deficits".
In some cases, a spectrum approach joins together conditions that were previously considered separately. A notable example of this trend is the autism spectrum, where conditions on this spectrum may now all be referred to as autism spectrum disorders. In other cases, what was treated as a single disorder comes to be seen (or seen once again) as comprising a range of types, a notable example being the bipolar spectrum. A spectrum approach may also expand the type or the severity of issues which are included, which may lessen the gap with other diagnoses or with what is considered "normal". Proponents of this approach argue that it is in line with evidence of gradations in the type or severity of symptoms in the general population.
In some cases, a spectrum approach joins together conditions that were previously considered separately. A notable example of this trend is the autism spectrum, where conditions on this spectrum may now all be referred to as autism spectrum disorders. In other cases, what was treated as a single disorder comes to be seen (or seen once again) as comprising a range of types, a notable example being the bipolar spectrum. A spectrum approach may also expand the type or the severity of issues which are included, which may lessen the gap with other diagnoses or with what is considered "normal". Proponents of this approach argue that it is in line with evidence of gradations in the type or severity of symptoms in the general population.
Origin
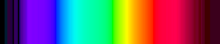
The visible color spectrum
The term spectrum was originally used in physics to indicate an apparent qualitative distinction arising from a quantitative continuum (i.e. a series of distinct colors experienced when a beam of white light is dispersed by a prism according to wavelength). Isaac Newton first used the word spectrum (Latin for "appearance" or "apparition") in print in 1671, in describing his experiments in optics.
The term was first used by analogy in psychiatry
with a slightly different connotation, to identify a group of
conditions that is qualitatively distinct in appearance but believed to
be related from an underlying pathogenic point of view. It has been
noted that for clinicians trained after the publication of DSM-III
(1980), the spectrum concept in psychiatry may be relatively new, but
that it has a long and distinguished history that dates back to Emil Kraepelin and beyond. A dimensional concept was proposed by Ernst Kretschmer in 1921 for schizophrenia (schizothymic – schizoid – schizophrenic) and for affective disorders (cyclothymic temperament – cycloid 'psychopathy' – manic-depressive disorder), as well as by Eugen Bleuler
in 1922. The term "spectrum" was first used in psychiatry in 1968 in
regard to a postulated schizophrenia spectrum, at that time meaning a
linking together of what were then called "schizoid personalities", in people diagnosed with schizophrenia and their genetic relatives (see Seymour S. Kety).
For different investigators, the hypothetical common disease-causing link has been of a different nature.
Related concepts
A spectrum approach generally overlays or extends a categorical approach, which today is most associated with the Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Statistical Classification of Diseases and Related Health Problems
(ICD). In these diagnostic guides, disorders are considered present if
there is a certain combination and number of symptoms. Gradations of
present versus absent are not allowed, although there may be subtypes of
severity within a category. The categories are also polythetic, because
a constellation of symptoms is laid out and different patterns of them
can qualify for the same diagnosis. These categories are aids important
for us practical purposes such as providing specific labels to
facilitate payments for mental health professionals.
They have been described as clearly worded, with observable criteria,
and therefore an advance over some previous models for research
purposes.
A spectrum approach sometimes starts with the nuclear, classic
DSM diagnostic criteria for a disorder (or may join together several
disorders), and then include an additional broad range of issues such as
temperaments or traits, lifestyle, behavioral patterns, and personality
characteristics.
In addition, the term 'spectrum' may be used interchangeably with continuum,
although the latter goes further in suggesting a direct straight line
with no significant discontinuities. Under some continuum models, there
are no set types or categories at all, only different dimensions along
which everyone varies (hence a dimensional approach).
An example can be found in personality or temperament models. For example, a model that was derived from linguistic expressions of individual differences is subdivided into the Big Five personality traits, where everyone can be assigned a score along each of the five dimensions. This is by contrast to models of 'personality types' or temperament, where some have a certain type and some do not. Similarly, in the classification of mental disorders,
a dimensional approach, which is being considered for the DSM-V, would
involve everyone having a score on personality trait measures. A
categorical approach would only look for the presence or absence of
certain clusters of symptoms, perhaps with some cut-off points for
severity for some symptoms only, and as a result diagnose some people
with personality disorders.
A spectrum approach, by comparison, suggests that although there
is a common underlying link, which could be continuous, particular sets
of individuals present with particular patterns of symptoms (i.e.
syndrome or subtype), reminiscent of the visible spectrum of distinct colors after refraction of light by a prism.
It has been argued that within the data used to develop the DSM
system there is a large literature leading to the conclusion that a
spectrum classification provides a better perspective on phenomenology (appearance and experience) of psychopathology
(mental difficulties) than a categorical classification system.
However, the term has a varied history, meaning one thing when referring
to a schizophrenia spectrum and another when referring to bipolar or
obsessive–compulsive disorder spectrum, for example.
Types of spectrum
The widely used DSM and ICD (Chapter 5)
manuals are generally limited to categorical diagnoses. However, some
categories include a range of subtypes which vary from the main
diagnosis in clinical presentation or typical severity. Some categories
could be considered subsyndromal (not meeting criteria for the full diagnosis) subtypes. In addition, many of the categories include a 'not otherwise specified'
subtype, where enough symptoms are present but not in the main
recognized pattern; in some categories this is the most common
diagnosis.
Spectrum concepts used in research or clinical practice include the following.
Anxiety, stress, and dissociation
Several types of spectrum are in use in these areas, some of which are being considered in the DSM-5.
A generalized anxiety spectrum
– this spectrum has been defined by duration of symptoms: a type
lasting over six months (a DSM-IV criterion), over one month (DSM-III),
or lasting two weeks or less (though may recur), and also isolated
anxiety symptoms not meeting criteria for any type.
A social anxiety spectrum – this has been defined to span shyness to social anxiety disorder, including typical and atypical presentations, isolated signs and symptoms, and elements of avoidant personality disorder.
A panic-agoraphobia spectrum – due to the heterogeneity
(diversity) found in individual clinical presentations of panic
disorder and agoraphobia, attempts have been made to identify symptom
clusters in addition to those included in the DSM diagnoses, including
through the development of a dimensional questionnaire measure.
A post-traumatic stress spectrum or trauma and loss spectrum
– work in this area has sought to go beyond the DSM category and
consider in more detail a spectrum of severity of symptoms (rather than
just presence or absence for diagnostic purposes), as well as a spectrum
in terms of the nature of the stressor (e.g. the traumatic incident)
and a spectrum of how people respond to trauma. This identifies a
significant amount of symptoms and impairment below threshold for DSM
diagnosis but nevertheless important, and potentially also present in
other disorders a person might be diagnosed with.
A depersonalization-derealization spectrum
– although the DSM identifies only a chronic and severe form of
depersonalization disorder, and the ICD a
'depersonalization-derealization syndrome', a spectrum of severity has
long been identified, including short-lasting episodes commonly
experienced in the general population and often associated with other
disorders.
Obsessions and compulsions
An obsessive–compulsive spectrum – this can include a wide range of disorders from Tourette syndrome to the hypochondrias, as well as forms of eating disorder, itself a spectrum of related conditions.
General developmental disorders
An autistic spectrum – in its simplest form this joins together autism and Asperger syndrome, and can additionally include other pervasive developmental disorders (PDD). These include PDD 'not otherwise specified' (including 'atypical autism'), as well as Rett syndrome and childhood disintegrative disorder
(CDD). The first three of these disorders are commonly called the
autism spectrum disorders; the last two disorders are much rarer, and
are sometimes placed in the autism spectrum and sometimes not.
The merging of these disorders is based on findings that the symptom
profiles are similar, such that individuals are better differentiated by
clinical specifiers (i.e. dimensions of severity, such as extent of
social communication difficulties or how fixed or restricted behaviors
or interests are) and associated features (e.g. known genetic disorders,
epilepsy, intellectual disabilities). The term specific developmental disorders is reserved for categorizing particular specific learning disabilities and developmental disorders affecting coordination.
Psychosis
The schizophrenia spectrum or psychotic spectrum – there are numerous psychotic spectrum disorders already in the DSM, many involving reality distortion. These include:
- Five subtypes of schizophrenia (although eliminated in DSM-5)
- Two forms of shorter duration (schizophreniform disorder and brief psychotic disorder)
- Two delusional disorders (delusional disorder and shared psychotic disorder)
- Schizoaffective disorder
- Catatonia
- Schizotypal personality disorder
There are also traits identified in first degree relatives of those diagnosed with schizophrenia associated with the spectrum.
Other spectrum approaches include more specific individual phenomena
which may also occur in non-clinical forms in the general population,
such as some paranoid beliefs or hearing voices. Some researchers have
also proposed that avoidant personality disorder and related social anxiety traits should be considered part of a schizophrenia spectrum.
Psychosis accompanied by mood disorder may be included as a
schizophrenia spectrum disorder, or may be classed separately as below.
Schizoaffective disorders
A schizoaffective spectrum
– this spectrum refers to features of both psychosis (hallucinations,
delusions, thought disorder etc.) and mood disorder (see below). The DSM
has, on the one hand, a category of schizoaffective disorder (which may
be more affective
(mood) or more schizophrenic), and on the other hand psychotic bipolar
disorder and psychotic depression categories. A spectrum approach joins
these together, and may additionally include specific clinical variables
and outcomes, which initial research suggested may not be particularly
well captured by the different diagnostic categories except at the
extremes.
Schizophrenia-like PDs
Schizoid personality disorder, schizotypal personality disorder, and paranoid personality disorder can be considered Schizophrenia-like Personality Disorders because of their links to the schizophrenia spectrum.
Mood
A mood disorder (affective) spectrum or bipolar spectrum or depressive spectrum. These approaches have expanded out in different directions. On the one hand, work on major depressive disorder
has identified a spectrum of subcategories and subthreshold symptoms
which are prevalent, recurrent and associated with treatment needs.
People are found to move between the subtypes and the main diagnostic
type over time, suggesting a spectrum. This spectrum can include already
recognised categories of minor depressive disorder, 'melancholic depression' and various kinds of atypical depression.
Going in another direction, numerous links and overlaps have been
found between major depressive disorder and bipolar syndromes,
including mixed states (simultaneous depression and mania or hypomania).
Hypomanic ('below manic') and more rarely manic signs and symptoms have
been found in a significant number of cases of major depressive
disorder, suggesting not a categorical distinction but a dimension of
frequency which is higher in bipolar II and higher again in bipolar I.
In addition, numerous subtypes of bipolar have been proposed beyond the
types already in the DSM (which includes a milder form called cyclothymia).
These extra subgroups have been defined in terms of more detailed
gradations of mood severity, or the rapidity of cycling, or the extent
or nature of psychotic symptoms. Furthermore, due to shared
characteristics between some types of bipolar disorder and borderline personality disorder,
some researchers have suggested they may both lie on a spectrum of
affective disorders, although others see more links to post-trauma
syndromes.
Substance use
A spectrum of drug use, drug abuse and substance dependence – one spectrum of this type, adopted by the Health Officers Council of British Columbia
in 2005, does not employ loaded terms and distinctions such as "use"
vs. "abuse", but explicitly recognizes a spectrum ranging from
potentially beneficial to chronic dependence
(also known as addiction). The model includes the role not just of the
individual but of society, culture and availability of substances. In
concert with the identified spectrum of drug use, a spectrum of policy
approaches was identified which depended partly on whether the drug in
question was available in a legal, for-profit commercial economy, or at
the other of the spectrum only in a criminal/prohibition, black-market
economy. In addition, a standardized questionnaire has been developed in psychiatry based on a spectrum concept of substance use.
Paraphilias and obsessions
The interpretative key of "Spectrum", developed from the concept of Related Disorders has been considered also in paraphilias.
Paraphilic behavior is triggered by thoughts or urges that are
psychopathologically close to obsessive impulsive area. Hollander (1996)
includes in the obsessive-compulsive spectrum neurological related
obsessive disorders, body perception related disorders and
impulsivity-compulsivity disorders. In this continuum from impulsivity
to compulsivity is particularly hard to find a clear borderline between
the two entities.
On this point of view, paraphilias represent such as sexual
behaviors due to a high impulsivity-compulsivity drive. It is difficult
to distinguish impulsivity from compulsivity: sometimes paraphilic
behaviors are prone to achieve pleasure (desire or fantasy), in some
other cases these attitudes are merely expressions of anxiety, and the
behavioral perversion is an attempt to reduce anxiety. In the last case,
the pleasure gained is short in time and is followed by a new increase
in anxiety levels, such as it can be seen in an obsessive patient after
he performs his compulsion.
Eibl-Eibelsfeldt (1984) underlines a female sexual arousal
condition during flight and fear reactions. Some women, with masochistic
traits, can reach orgasm in such conditions.
Broad spectrum approach
Various higher-level types of spectrum have also been proposed, that subsume conditions into fewer but broader overarching groups.
One psychological model based on factor analysis, originating from developmental studies but also applied to adults, posits that many disorders fall on either an "internalizing" spectrum (characterized by negative affectivity;
subdivides into a "distress" subspectrum and a "fear" subspectrum) or
an "externalizing" spectrum (characterized by negativity affectivity
plus disinhibition). These spectra are hypothetically linked to
underlying variation in some of the Big five personality traits. Another theoretical model proposes that the dimensions of fear and anger,
defined in a broad sense, underlie a broad spectrum of mood, behavioral
and personality disorders. In this model, different combinations of
excessive or deficient fear and anger correspond to different
neuropsychological temperament types hypothesized to underlie the
spectrum of disorders.
Similar approaches refer to the overall 'architecture' or
'meta-structure', particularly in relation to the development of the DSM
or ICD systems. Five proposed meta-structure groupings were recently
proposed in this way, based on views and evidence relating to risk
factors and clinical presention. The clusters of disorder that emerged
were described as neurocognitive (identified mainly by neural substrate
abnormalities), neurodevelopmental (identified mainly by early and
continuing cognitive deficits), psychosis (identified mainly by clinical
features and biomarkers for information processing deficits), emotional
(identified mainly by being preceded by a temperament of negative
emotionality), and externalizing (identified mainly be being preceded by
disinhibition).
However, the analysis was not necessarily able to validate one
arrangement over others. From a psychological point of view, it has been
suggested that the underlying phenomena are too complex, inter-related
and continuous – with too poorly understood a biological or
environmental basis – to expect that everything can be mapped into a set
of categories for all purposes. In this context the overall system of
classification is to some extent arbitrary, and could be thought of as a
user inferface which may need to satisfy different purposes.