| Hyperparathyroidism | |
|---|---|
 | |
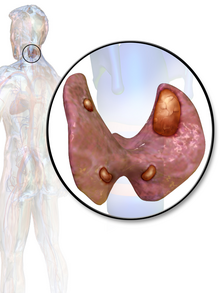
| Thyroid and parathyroid | |
| Specialty | Endocrinology |
| Symptoms | None, kidney stones, weakness, depression, bone pains, confusion, increased urination |
| Complications | Osteoporosis |
| Usual onset | 50 to 60 |
| Types | Primary, secondary |
| Causes | Primary: parathyroid adenoma, multiple benign tumors, parathyroid cancer Secondary: vitamin D deficiency, chronic kidney disease, low blood calcium |
| Diagnostic method | High blood calcium and high PTH levels |
| Treatment | Monitoring, surgery, intravenous normal saline, cinacalcet |
| Frequency | ~2 per 1,000 |
Hyperparathyroidism is an increase in parathyroid hormone (PTH) levels in the blood. This occurs from a disorder either within the parathyroid glands (primary hyperparathyroidism) or outside the parathyroid glands (secondary hyperparathyroidism). Most people with primary disease have no symptoms at the time of diagnosis. When symptoms occur, they are due to elevated blood calcium. With long-standing elevation, the most common symptom is kidney stones. Others symptoms may include bone pain, weakness, depression, confusion, and increased urination. Both primary and secondary may result in osteoporosis (weakening of the bones).
In 80% of cases, primary hyperparathyroidism is due to a single benign tumor known as a parathyroid adenoma. Most of the remainder are due to several of these adenomas. Rarely it may be due to parathyroid cancer. Secondary hyperparathyroidism typically occurs due to vitamin D deficiency, chronic kidney disease, or other causes of low blood calcium. The diagnosis of primary hyperparathyroidism is made by finding elevated calcium and PTH in the blood.
Primary hyperparathyroidism may be cured by removing the adenoma or overactive parathyroid glands. In those without symptoms, mildly increased blood calcium levels, normal kidneys, and normal bone density monitoring may be all that is required. The medication cinacalcet may also be used to decrease PTH levels. In those with very high blood calcium levels, treatment may include large amounts of intravenous normal saline. Low vitamin D levels should be corrected.
Primary hyperparathyroidism is the most common type. In the developed world, between one and four per thousand people are affected. It occurs three times more often in women than men and is typically diagnosed between the ages of 50 and 60. The disease was first described in the 1700s. In the late 1800s, it was determined to be related to the parathyroid. Surgery as a treatment was first carried out in 1925.
Signs and symptoms
Symptoms depend on whether the hyperparathyroidism is the result of parathyroid overactivity or secondary.
In primary hyperparathyroidism about 75% of people have no symptoms. The problem is often picked up during blood work for other reasons via a raised calcium.
Many other people only have non-specific symptoms. Symptoms directly
due to hypercalcemia are relatively rare, being more common in patients
with malignant hypercalcemia. If present, common manifestations of
hypercalcemia include weakness and fatigue, depression, bone pain,
muscle soreness (myalgias), decreased appetite, feelings of nausea and vomiting, constipation, polyuria, polydipsia, cognitive impairment, kidney stones, and osteopenia or osteoporosis. A history of acquired racquet nails (brachyonychia) may be indicative of bone resorption.
Parathyroid adenomas are very rarely detectable on clinical
examination. Surgical removal of a parathyroid tumor eliminates the
symptoms in most patients.
In secondary hyperparathyroidism the parathyroid gland is
behaving normally; clinical problems are due to bone resorption and
manifest as bone syndromes such as rickets, osteomalacia and renal osteodystrophy.
Causes
Radiation exposure increases the risk of primary hyperparathyroidism. A number of genetic conditions including multiple endocrine neoplasia syndromes also increase the risk.
Mechanism
Normal parathyroid glands measure the ionized calcium (Ca2+)
concentration in the blood and secrete parathyroid hormone accordingly:
if the ionized calcium rises above normal, the secretion of PTH is
decreased, whereas when the Ca2+ level falls, parathyroid hormone secretion is increased.
Secondary hyperparathyroidism occurs if the calcium level is
abnormally low. The normal glands respond by secreting parathyroid
hormone at a persistently high rate. This typically occurs when the 1,25 dihydroxyvitamin D3 levels in the blood are low and there is hypocalcemia. A lack of 1,25 dihydroxyvitamin D3 can result from a deficient dietary intake of vitamin D, or from a lack of exposure of the skin to sunlight, so the body cannot make its own vitamin D from cholesterol. The resulting hypovitaminosis D is usually due to a partial combination of both factors. Vitamin D3 (or cholecalciferol) is converted to 25-hydroxyvitamin D (or calcidiol)
by the liver, from where it is transported via the circulation to the
kidneys where it is converted into the active hormone, 1,25
dihydroxyvitamin D3. Thus a third cause of secondary hyperparathyroidism is chronic kidney disease. Here the ability to manufacture 1,25 dihydroxyvitamin D3 is compromised, resulting in hypocalcemia.
Diagnosis
Calcification in the brain due to hyperparathyroidism
Pepper & Salt, classical X-Ray appearance of hyperparathyroidisim
The gold standard of diagnosis is the PTH immunoassay.
Once an elevated PTH has been confirmed, the goal of diagnosis is to
determine whether the hyperparathyroidism is primary or secondary in
origin by obtaining a serum calcium level:
| Serum calcium | Phosphate | ALP | PTH | Likely type |
| ↑ | ↓ | ↑ | ↑ | Primary hyperparathyroidism |
| ↓ | ↑ | ↑ | ↑ | Secondary hyperparathyroidism |
Tertiary hyperparathyroidism has a high PTH and a high serum calcium.
It is differentiated from primary hyperparathyroidism by a history of chronic kidney failure and secondary hyperparathyroidism.
Hyperparathyroidism can cause hyperchloremia and increase renal
bicarbonate loss, which may result in a normal anion gap metabolic
acidosis.
Differential diagnosis
Familial benign hypocalciuric hypercalcaemia can present with similarly lab changes. In this condition the calcium creatinine clearance ratio; however, is typically under 0.01.
Blood tests
Intact PTH
In
primary hyperparathyroidism, parathyroid hormone (PTH) levels are
either elevated or "inappropriately normal" in the presence of elevated
calcium. Typically PTH levels vary greatly over time in the affected
patient and (as with Ca and Ca++ levels) must be retested several times
to see the pattern. The currently accepted test for PTH is Intact PTH,
which detects only relatively intact and biologically active PTH
molecules. Older tests often detected other, inactive fragments. Even
"Intact PTH" may be inaccurate in patients with kidney dysfunction.
Calcium levels
In cases of primary hyperparathyroidism or tertiary hyperparathyroidism heightened PTH leads to increased serum calcium (hypercalcemia) due to:
- Increased bone resorption, allowing flow of calcium from bone to blood
- Reduced kidney clearance of calcium
- Increased intestinal calcium absorption
Serum phosphate
In
primary hyperparathyroidism, serum phosphate levels are abnormally low
as a result of decreased reabsorption of phosphate in the kidney
tubules. However, this is only present in about 50% of cases. This
contrasts with secondary hyperparathyroidism, in which serum phosphate levels are generally elevated because of kidney disease.
Alkaline phosphatase
Alkaline phosphatase
levels are usually elevated in hyperparathyroidism. In primary
hyperparathyroidism, levels may remain within the normal range, however
this is 'inappropriately normal' given the increased levels of plasma
calcium.
Nuclear medicine
A technetium sestamibi scan is a procedure in nuclear medicine that identifies hyperparathyroidism (or parathyroid adenoma). It is used by surgeons to locate ectopic parathyroid adenomas, most commonly found in the anterior mediastinum.
Classification
Primary
Primary hyperparathyroidism results from a hyperfunction of the parathyroid glands themselves. There is oversecretion of PTH due to a parathyroid adenoma, parathyroid hyperplasia or, rarely, a parathyroid carcinoma. This disease is often characterized by the quartet stones, bones, groans, and psychiatric overtones referring to the presence of kidney stones, hypercalcemia, constipation and peptic ulcers, as well as depression, respectively.
In a minority of cases this occurs as part of a multiple endocrine neoplasia (MEN) syndrome, either type 1 (caused by a mutation in the gene MEN1) or type 2a (caused by a mutation in the gene RET). Other mutations that have been linked to parathyroid neoplasia include mutations in the genes HRPT2, and CASR.
Patients with bipolar disorder who are receiving long-term lithium treatment are at increased risk for hyperparathyroidism.
Elevated calcium levels are found in 15% to 20% of patients who have
been taking lithium long-term. However, only a few of these patients
have significantly elevated levels of parathyroid hormone and clinical
symptoms of hyperparathyroidism. Lithium-associated hyperparathyroidism
is usually caused by a single parathyroid adenoma.
Secondary
Secondary hyperparathyroidism is due to physiological (i.e. appropriate) secretion of parathyroid hormone (PTH) by the parathyroid glands in response to hypocalcemia (low blood calcium levels). The most common causes are vitamin D deficiency (caused by lack of sunlight, diet or malabsorption) and chronic kidney failure.
Lack of vitamin D leads to reduced calcium absorption by the
intestine leading to hypocalcemia and increased parathyroid hormone
secretion. This increases bone resorption.
In chronic kidney failure the problem is more specifically failure to
convert vitamin D to its active form in the kidney. The bone disease in
secondary hyperparathyroidism caused by kidney failure is termed renal osteodystrophy.
Tertiary
Tertiary hyperparathyroidism
is seen in those with long-term secondary hyperparathyroidism, which
eventually leads to hyperplasia of the parathyroid glands and a loss of
response to serum calcium levels. This disorder is most often seen in
patients with end-stage kidney disease and is an autonomous activity.
Treatment
Treatment depends on the type of hyperparathyroidism encountered.
Primary
People with primary hyperparathyroidism who are symptomatic benefit from parathyroidectomy—surgery to remove the parathyroid tumor (parathyroid adenoma). Indications for surgery are as follows:
- Symptomatic hyperparathyroidism
- Asymptomatic hyperparathyroidism with any of the following:
- 24-hour urinary calcium > 400 mg (see Foot Note, below)
- serum calcium > 1 mg/dL above upper limit of normal
- Creatinine clearance > 30% below normal for patient's age
- Bone density > 2.5 standard deviations below peak (i.e., T-score of -2.5)
- People age < 50
Surgery can rarely result in hypoparathyroidism.
Secondary
In
people with secondary hyperparathyroidism, the high PTH levels are an
appropriate response to low calcium and treatment must be directed at
the underlying cause of this (usually vitamin D deficiency or chronic kidney failure).
If this is successful PTH levels return to normal levels, unless PTH
secretion has become autonomous (tertiary hyperparathyroidism).
Calcimimetics
A calcimimetic (such as cinacalcet)
is a potential therapy for some people with severe hypercalcemia and
primary hyperparathyroidism who are unable to undergo parathyroidectomy,
and for secondary hyperparathyroidism on dialysis.
Treatment of secondary hyperparathyroidism with a calcimimetic in
those on dialysis for CKD does not alter the risk of early death;
however, it does decrease the likelihood of needing a parathyroidectomy. Treatment carries the risk of low blood calcium levels and vomiting.
History
The oldest known case was found in a cadaver from an Early Neolithic cemetery in southwest Germany.