| Phenylketonuria | |
|---|---|
| Other names | Phenylalanine hydroxylase deficiency, PAH deficiency, Følling disease |
 | |
| Phenylalanine | |
| Specialty | Medical genetics, pediatrics |
| Symptoms | Without treatment intellectual disability, seizures, behavioral problems, mental disorders, musty smell |
| Usual onset | At birth |
| Types | Classic, variant |
| Causes | Genetic (autosomal recessive) |
| Diagnostic method | Newborn screening programs in many countries |
| Treatment | Diet low in foods that contain phenylalanine, special supplements |
| Medication | Sapropterin dihydrochloride, pegvaliase |
| Prognosis | Normal health with treatment |
| Frequency | ~1 in 12,000 newborns |
Phenylketonuria (PKU) is an inborn error of metabolism that results in decreased metabolism of the amino acid phenylalanine. Untreated, PKU can lead to intellectual disability, seizures, behavioral problems, and mental disorders. It may also result in a musty smell and lighter skin. A baby born to a mother who has poorly treated PKU may have heart problems, a small head, and low birth weight.
Phenylketonuria is a genetic disorder inherited from a person's parents. It is due to mutations in the PAH gene, which results in low levels of the enzyme phenylalanine hydroxylase. This results in the buildup of dietary phenylalanine to potentially toxic levels. It is autosomal recessive, meaning that both copies of the gene must be mutated for the condition to develop. There are two main types, classic PKU and variant PKU, depending on whether any enzyme function remains. Those with one copy of a mutated gene typically do not have symptoms. Many countries have newborn screening programs for the disease.
Treatment is with a diet low in foods that contain phenylalanine and special supplements. Babies should use a special formula with a small amount of breast milk. The diet should begin as soon as possible after birth and be continued for at least 10 years, if not lifelong. People who are diagnosed early and maintain a strict diet can have normal health and a normal life span. Effectiveness is monitored through periodic blood tests. The medication sapropterin dihydrochloride may be useful in some.
Phenylketonuria affects about 1 in 12,000 babies. Males and females are affected equally. The disease was discovered in 1934 by Ivar Asbjørn Følling, with the importance of diet determined in 1953. Gene therapy, while promising, requires a great deal more study as of 2014.
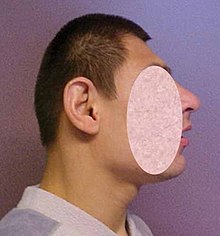
Signs and symptoms
Abnormally small head (microcephaly)
Untreated PKU can lead to intellectual disability, seizures, behavioral problems, and mental disorders. It may also result in a musty smell and lighter skin. A baby born to a mother who has poorly treated PKU may have heart problems, a small head, and low birth weight.
Because the mother's body is able to break down phenylalanine
during pregnancy, infants with PKU are normal at birth. The disease is
not detectable by physical examination at that time, because no damage
has yet been done. Newborn screening is performed to detect the disease
and initiate treatment before any damage is done. The blood sample is
usually taken by a heel prick,
typically performed 2–7 days after birth. This test can reveal elevated
phenylalanine levels after one or two days of normal infant feeding.
If a child is not diagnosed during the routine newborn screening
test and a phenylalanine restricted diet is not introduced, then
phenylalanine levels in the blood will increase over time. Toxic levels
of phenylalanine (and insufficient levels of tyrosine) can interfere
with infant development in ways which have permanent effects. The
disease may present clinically with seizures, hypopigmentation (excessively fair hair and skin), and a "musty odor" to the baby's sweat and urine (due to phenylacetate,
a carboxylic acid produced by the oxidation of phenylketone). In most
cases, a repeat test should be done at approximately two weeks of age to
verify the initial test and uncover any phenylketonuria that was
initially missed.
Untreated children often fail to attain early developmental
milestones, develop microcephaly, and demonstrate progressive impairment
of cerebral function. Hyperactivity, EEG abnormalities, and seizures, and severe learning disabilities are major clinical problems later in life. A characteristic "musty or mousy" odor on the skin, as well as a predisposition for eczema, persist throughout life in the absence of treatment.
The damage done to the brain if PKU is untreated during the first
months of life is not reversible. It is critical to control the diet of
infants with PKU very carefully so that the brain has an opportunity to
develop normally. Affected children who are detected at birth and
treated are much less likely to develop neurological problems or have
seizures and intellectual disability (though such clinical disorders are
still possible.)
In general, however, outcomes for people treated for PKU are
good. Treated people may have no detectable physical, neurological, or
developmental problems at all.
Genetics
Phenylketonuria is inherited in an autosomal recessive fashion
PKU is an autosomal recessive metabolic genetic disorder. As an autosomal recessive disorder, two PKU alleles
are required for an individual to experience symptoms of the disease.
If both parents are carriers for PKU, there is a 25% chance any child
they have will be born with the disorder, a 50% chance the child will be
a carrier, and a 25% chance the child will neither develop nor be a
carrier for the disease.
PKU is characterized by homozygous or compound heterozygous mutations in the gene for the hepatic enzyme phenylalanine hydroxylase (PAH), rendering it nonfunctional. This enzyme is necessary to metabolize the amino acid phenylalanine (Phe) to the amino acid tyrosine (Tyr). When PAH activity is reduced, phenylalanine accumulates and is converted into phenylpyruvate (also known as phenylketone), which can be detected in the urine.
Carriers of a single PKU allele do not exhibit symptoms of the
disease but appear to be protected to some extent against the fungal
toxin ochratoxin A. This accounts for the persistence of the allele in certain populations in that it confers a selective advantage—in other words, being a heterozygote is advantageous.
The PAH gene is located on chromosome 12 in the bands 12q22-q24.2. As of 2000, around 400 disease-causing mutations had been found in the PAH gene. This is an example of allelic genetic heterogeneity.
Pathophysiology
When
Phe cannot be metabolized by the body, a typical diet that would be
healthy for people without PKU causes abnormally high levels of Phe to
accumulate in the blood, which is toxic to the brain. If left untreated,
complications of PKU include severe intellectual disability, brain
function abnormalities, microcephaly, mood disorders, irregular motor
functioning, and behavioral problems such as attention deficit hyperactivity disorder, as well as physical symptoms such as a "musty" odor, eczema, and unusually light skin and hair coloration.
Classical PKU
Classical PKU, and its less severe forms "mild PKU" and "mild hyperphenylalaninemia" are caused by a mutated gene for the enzyme phenylalanine hydroxylase
(PAH), which converts the amino acid phenylalanine ("Phe") to other
essential compounds in the body, in particular tyrosine. Tyrosine is a
conditionally essential amino acid
for PKU patients because without PAH it cannot be produced in the body
through the breakdown of phenylalanine. Tyrosine is necessary for the
production of neurotransmitters like epinephrine, norepinephrine, and
dopamine.
PAH deficiency causes a spectrum of disorders, including classic
phenylketonuria (PKU) and mild hyperphenylalaninemia (also known as
"hyperphe"
or "mild HPA"), a less severe accumulation of phenylalanine. Patients
with "hyperphe" may have more functional PAH enzyme and be able to
tolerate larger amounts of phenylalanine in their diets than those with
classic PKU, but unless dietary intake is at least somewhat restricted,
their blood Phe levels are still higher than the levels in people with
normal PAH activity.
Phenylalanine is a large, neutral amino acid (LNAA). LNAAs compete for transport across the blood–brain barrier (BBB) via the large neutral amino acid transporter
(LNAAT). If phenylalanine is in excess in the blood, it will saturate
the transporter. Excessive levels of phenylalanine tend to decrease the
levels of other LNAAs in the brain. As these amino acids are necessary
for protein and neurotransmitter synthesis, Phe buildup hinders the
development of the brain, causing intellectual disability.
Recent research suggests that neurocognitive, psychosocial,
quality of life, growth, nutrition, bone pathology are slightly
suboptimal even for patients who are treated and maintain their Phe
levels in the target range, if their diet is not supplemented with other
amino acids.
Classic PKU dramatically affects myelination and white matter
tracts in untreated infants; this may be one major cause of neurological
disorders associated with phenylketonuria. Differences in white matter
development are observable with magnetic resonance imaging.
Abnormalities in gray matter can also be detected, particularly in the
motor and pre-motor cortex, thalamus and the hippocampus.
It was recently suggested that PKU may resemble amyloid
diseases, such as Alzheimer's disease and Parkinson's disease, due to
the formation of toxic amyloid-like assemblies of phenylalanine.
Other non-PAH mutations can also cause PKU.
Tetrahydrobiopterin-deficient hyperphenylalaninemia
A rarer form of hyperphenylalaninemia is tetrahydrobiopterin deficiency, which occurs when the PAH enzyme is normal, and a defect is found in the biosynthesis or recycling of the cofactor tetrahydrobiopterin (BH4). BH4 is necessary for proper activity of the enzyme PAH, and this coenzyme
can be supplemented as treatment. Those who suffer from this form of
hyperphenylalaninemia may have a deficiency of tyrosine (which is
created from phenylalanine by PAH), in which case treatment is
supplementation of tyrosine to account for this deficiency.
Levels of dopamine can be used to distinguish between these two types. Tetrahydrobiopterin is required to convert Phe to Tyr and is required to convert Tyr to L-DOPA via the enzyme tyrosine hydroxylase. L-DOPA, in turn, is converted to dopamine. Low levels of dopamine lead to high levels of prolactin. By contrast, in classical PKU (without dihydrobiopterin involvement), prolactin levels would be relatively normal.
Tetrahydrobiopterin deficiency can be caused by defects in four genes. They are known as HPABH4A, HPABH4B, HPABH4C, and HPABH4D.
Metabolic pathways
Pathophysiology
of phenylketonuria, which is due to the absence of functional
phenylalanine hydroxylase (classical subtype) or functional enzymes for
the recycling of tetrahydrobiopterin (new variant subtype) utilized in the first step of the metabolic pathway.
The enzyme phenylalanine hydroxylase normally converts the amino acid phenylalanine into the amino acid tyrosine.
If this reaction does not take place, phenylalanine accumulates and
tyrosine is deficient. Excessive phenylalanine can be metabolized into
phenylketones through the minor route, a transaminase pathway with glutamate. Metabolites include phenylacetate, phenylpyruvate and phenethylamine.
Elevated levels of phenylalanine in the blood and detection of
phenylketones in the urine is diagnostic, however most patients are
diagnosed via newborn screening.
Screening
Blood is taken from a two-week-old baby to test for phenylketonuria
PKU is commonly included in the newborn screening
panel of many countries, with varied detection techniques. Most babies
in developed countries are screened for PKU soon after birth. Screening for PKU is done with bacterial inhibition assay (Guthrie test), immunoassays using fluorometric or photometric detection, or amino acid measurement using tandem mass spectrometry (MS/MS). Measurements done using MS/MS determine the concentration of Phe and the ratio of Phe to tyrosine, the ratio will be elevated in PKU.
Treatment
PKU
is not curable. However, if PKU is diagnosed early enough, an affected
newborn can grow up with normal brain development by managing and
controlling phenylalanine ("Phe") levels through diet, or a combination
of diet and medication.
Diet
People who
follow the prescribed dietary treatment from birth may have no symptoms.
Their PKU would be detectable only by a blood test. People must adhere
to a special diet low in Phe for optimal brain development. Since Phe is
necessary for the synthesis of many proteins, it is required for
appropriate growth, but levels must be strictly controlled.
For people who do not have phenylketonuria, the U.S. Institute of
Medicine set recommended at least 33 mg/kg body weight/day
phenylalanine plus tyrosine for adults 19 years and older.
For people with PKU, a recommendation for children up to age 10 years
is 200 to 500 mg/d; for older children and adults 220 to 1200 mg/day.
Where in the range depends on body weight and age, and on monitoring
blood concentration.
Optimal health ranges (or "target ranges") are between 120 and 360 µmol/L or equivalently 2 to 6 mg/dL, and aimed to be achieved during at least the first 10 years, to allow the brain to develop normally.
The age at which people with PKU may safely go off diet is
subject to some debate. The diet should be maintained at least until the
age of eight or ten. Some evidence supports discontinued after 10 years
as a normal diet after that does not appear to have negative effects. One study however has shown temporarily detrimental effects when off the diet. There is no evidence for permanent brain damage in people who have gone off diet in adulthood. In case of mild neurocognitive impairment, the re-introduction of diet is indicated.
The diet requires restricting or eliminating foods high in Phe, such as soybeans, egg whites, shrimp, chicken breast, spirulina, watercress, fish, nuts, crayfish, lobster, tuna, turkey, legumes, and lowfat cottage cheese. Starchy foods, such as potatoes and corn
are generally acceptable in controlled amounts, but the quantity of Phe
consumed from these foods must be monitored. A food diary is usually
kept to record the amount of Phe consumed with each meal, snack, or
drink. An "exchange" system can be used to calculate the amount of Phe
in a food from the protein content identified on a nutritional
information label. Lower-protein "medical food" substitutes are often
used in place of normal bread, pasta,
and other grain-based foods, which contain a significant amount of Phe.
Many fruits and vegetables are lower in Phe and can be eaten in larger
quantities. Infants may still be breastfed to provide all of the
benefits of breastmilk, but the quantity must also be monitored and
supplementation for missing nutrients will be required. The sweetener aspartame, present in many diet foods and soft drinks, must also be avoided, as aspartame is metabolised into phenylalanine.
Different people can tolerate different amounts of Phe in their
diet. Regular blood tests are used to determine the effects of dietary
Phe intake on blood Phe level.
Nutritional supplements
Supplementary
"protein substitute" formulas are typically prescribed for people PKU
(starting in infancy) to provide the amino acids and other necessary
nutrients that would otherwise be lacking in a low-phenylalanine diet.
Tyrosine, which is normally derived from phenylalanine and which is
necessary for normal brain function, is usually supplemented.
Consumption of the protein substitute formulas can actually reduce
phenylalanine levels, probably because it stops the process of protein catabolism
from releasing Phe stored in the muscles and other tissues into the
blood. Many PKU patients have their highest Phe levels after a period of
fasting (such as overnight), because fasting triggers catabolism.
A diet that is low in phenylalanine but does not include protein
substitutes may also fail to lower blood Phe levels, since a
nutritionally insufficient diet may also trigger catabolism. For all
these reasons, the prescription formula is an important part of the
treatment for patients with classic PKU.
Tentative evidence supports dietary supplementation with large neutral amino acids (LNAAs). The LNAAs (e.g. leu, tyr, trp, met, his, ile, val, thr)
may compete with phe for specific carrier proteins that transport LNAAs
across the intestinal mucosa into the blood and across the blood–brain barrier into the brain. Its use is really only indicated in adults who will not follow an appropriate diet.
Another interesting treatment strategy is casein
glycomacropeptide (CGMP), which is a milk peptide naturally free of Phe
in its pure form CGMP can substitute for the main part of the free amino acids in the
PKU diet and provides several beneficial nutritional effects compared to
free amino acids. The fact that CGMP is a peptide ensures that the
absorption rate of its amino acids is prolonged compared to free amino
acids and thereby results in improved protein retention and increased satiety compared to free amino acids. Another important benefit of CGMP is that the taste is significantly improved[37] when CGMP substitutes part of the free amino acids and this may help ensure improved compliance to the PKU diet.
Furthermore, CGMP contains a high amount of the Phe-lowering LNAAs, which constitutes about 41 g per 100 g protein and will therefore help maintain plasma phe levels in the target range.
Enzyme substitutes
In 2018, the FDA approved an enzyme substitute called pegvaliase which metabolizes phenylalanine. It is for adults who are poorly managed on other treatments.
Tetrahydrobiopterin (BH4) (a cofactor for the oxidation of phenylalanine) when taken by mouth can reduce blood levels of this amino acid in some people. Most people, however, with the "classical" sequence of mutations, will have little or no benefit.
Mothers
For women with PKU, it is important for the health of their children to maintain low Phe levels before and during pregnancy.
Though the developing fetus may only be a carrier of the PKU gene, the
intrauterine environment can have very high levels of phenylalanine,
which can cross the placenta. The child may develop congenital heart
disease, growth retardation, microcephaly and intellectual disability as
a result. PKU-affected women themselves are not at risk of additional complications during pregnancy.
In most countries, women with PKU who wish to have children are
advised to lower their blood Phe levels (typically to between 2 and
6 mg/dL) before they become pregnant, and carefully control their levels
throughout the pregnancy. This is achieved by performing regular blood
tests and adhering very strictly to a diet, in general monitored on a
day-to-day basis by a specialist metabolic dietitian. In many cases, as
the fetus' liver begins to develop and produce PAH normally, the
mother's blood Phe levels will drop, requiring an increased intake to
remain within the safe range of 2–6 mg/dL. The mother's daily Phe intake
may double or even triple by the end of the pregnancy, as a result.
When maternal blood Phe levels fall below 2 mg/dL, anecdotal reports
indicate that the mothers may suffer adverse effects, including
headaches, nausea, hair loss, and general malaise. When low
phenylalanine levels are maintained for the duration of pregnancy, there
are no elevated levels of risk of birth defects compared with a baby
born to a non-PKU mother.
Epidemiology
| Country | Incidence |
|---|---|
| Australia | 1 in 10,000 |
| Brazil | 1 in 8,690 |
| Canada | 1 in 22,000 |
| China | 1 in 17,000 |
| Czechoslovakia | 1 in 7,000 |
| Denmark | 1 in 12,000 |
| Finland | 1 in 200,000 |
| France | 1 in 13,500 |
| India | 1 in 18,300 |
| Ireland | 1 in 4,500 |
| Italy | 1 in 17,000 |
| Japan | 1 in 125,000 |
| Korea | 1 in 41,000 |
| Netherlands | 1 in 18,000 |
| Norway | 1 in 14,500 |
| Philippines | 1 in 102,000 |
| Poland | 1 in 8,000 |
| Scotland | 1 in 5,300 |
| Spain | 1 in 20,000 |
| Sweden | 1 in 20,000 |
| Turkey | 1 in 2,600 |
| United Kingdom | 1 in 10,000 |
| United States | 1 in 25,000 |
The average number of new cases of PKU varies in different human
populations. United States Caucasians are affected at a rate of 1 in
10,000.[50]
Turkey has the highest documented rate in the world, with 1 in 2,600
births, while countries such as Finland and Japan have extremely low
rates with fewer than one case of PKU in 100,000 births. A 1987 study
from Slovakia reports a Roma population with an extremely high incidence
of PKU (one case in 40 births) due to extensive inbreeding.[51] It is the most common amino acid metabolic problem in the United Kingdom.[citation needed]
History
Before
the causes of PKU were understood, PKU caused severe disability in most
people who inherited the relevant mutations. Nobel and Pulitzer Prize
winning author Pearl S. Buck
had a daughter named Carol who lived with PKU before treatment was
available, and wrote a moving account of its effects in a book called The Child Who Never Grew.
Many untreated PKU patients born before widespread newborn screening
are still alive, largely in dependent living homes/institutions.
Phenylketonuria was discovered by the Norwegian physician Ivar Asbjørn Følling in 1934
when he noticed hyperphenylalaninemia (HPA) was associated with
intellectual disability. In Norway, this disorder is known as Følling's
disease, named after its discoverer. Følling was one of the first physicians to apply detailed chemical analysis to the study of disease.
In 1934 at Rikshospitalet,
Følling saw a young woman named Borgny Egeland. She had two children,
Liv and Dag, who had been normal at birth but subsequently developed
intellectual disability. When Dag was about a year old, the mother
noticed a strong smell to his urine. Følling obtained urine samples from
the children and, after many tests, he found that the substance causing
the odor in the urine was phenylpyruvic acid. The children, he
concluded, had excess phenylpyruvic acid in the urine, the condition
which came to be called phenylketonuria (PKU).
His careful analysis of the urine of the two affected siblings
led him to request many physicians near Oslo to test the urine of other
affected patients. This led to the discovery of the same substance he
had found in eight other patients. He conducted tests and found
reactions that gave rise to benzaldehyde and benzoic acid, which led him to conclude that the compound contained a benzene ring. Further testing showed the melting point to be the same as phenylpyruvic acid, which indicated that the substance was in the urine.
In 1954, Horst Bickel, Evelyn Hickmans and John Gerrard published a paper that described how they created a diet that was low in phenylalanine and the patient recovered. Bickel, Gerrard and Hickmans were awarded the John Scott Medal in 1962 for their discovery.
PKU was the first disorder to be routinely diagnosed through widespread newborn screening. Robert Guthrie introduced the newborn screening test for PKU in the early 1960s.
With the knowledge that PKU could be detected before symptoms were
evident, and treatment initiated, screening was quickly adopted around
the world. Ireland was the first country to introduce a national
screening programme in February 1966, Austria also started screening in 1966 and England in 1968.
In 2017 the European Guidelines were published. They were called for by the patient organizations such as the European Society for Phenylketonuria and Allied Disorders Treated as Phenylketonuria. They have received some critical reception.
Etymology and pronunciation
The word phenylketonuria uses combining forms of phenyl + ketone + -uria; it is pronounced /ˌfiːnaɪlˌkiːtəˈnjʊəriə, ˌfɛn-, -nɪl-, -nəl-, -toʊ-/.
Research
Other therapies are currently under investigation, including gene therapy.
Biomarin is currently conducting clinical trials to investigate PEG-PAL (PEGylated recombinant phenylalanine ammonia lyase
or ‘PAL’) is an enzyme substitution therapy in which the missing PAH
enzyme is replaced with an analogous enzyme that also breaks down Phe.
PEG-PAL is now in Phase 2 clinical development.