| Proteopathy | |
|---|---|
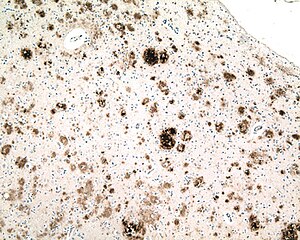 | |
| Micrograph of a section of the cerebral cortex from a patient with Alzheimer's disease, immunostained with an antibody to Aβ (brown), a protein fragment that accumulates in senile plaques and cerebral amyloid angiopathy. 10X microscope objective. |
In medicine, proteopathy (/proʊtiːˈɒpəθiː/; from proteo- [pref. protein]; -pathy [suff. disease]; proteopathies pl.; proteopathic adj) refers to a class of diseases in which certain proteins become structurally abnormal, and thereby disrupt the function of cells, tissues and organs of the body. Often the proteins fail to fold into their normal configuration; in this misfolded state, the proteins can become toxic in some way (a gain of toxic function) or they can lose their normal function. The proteopathies (also known as proteinopathies, protein conformational disorders, or protein misfolding diseases) include such diseases as Creutzfeldt–Jakob disease and other prion diseases, Alzheimer's disease, Parkinson's disease, amyloidosis, multiple system atrophy, and a wide range of other disorders (see List of Proteopathies). The term proteopathy was first proposed in 2000 by Lary Walker and Harry LeVine.
The concept of proteopathy can trace its origins to the mid-19th century, when, in 1854, Rudolf Virchow coined the term amyloid ("starch-like") to describe a substance in cerebral corpora amylacea that exhibited a chemical reaction resembling that of cellulose. In 1859, Friedreich and Kekulé demonstrated that, rather than consisting of cellulose, "amyloid" actually is rich in protein. Subsequent research has shown that many different proteins can form amyloid, and that all amyloids have in common birefringence in cross-polarized light after staining with the dye Congo Red, as well as a fibrillar ultrastructure when viewed with an electron microscope. However, some proteinaceous lesions lack birefringence and contain few or no classical amyloid fibrils, such as the diffuse deposits of Aβ protein in the brains of Alzheimer patients. Furthermore, evidence has emerged that small, non-fibrillar protein aggregates known as oligomers are toxic to the cells of an affected organ, and that amyloidogenic proteins in their fibrillar form may be relatively benign.
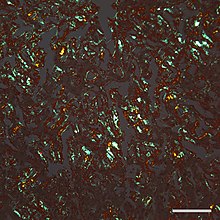
Micrograph of amyloid in a section of liver
that has been stained with the dye Congo Red and viewed with crossed
polarizing filters, yielding a typical orange-greenish birefringence.
20X microscope objective; the scale bar is 100 microns (0.1mm).
Pathophysiology
In
most, if not all proteopathies, a change in 3-dimensional folding
(conformation) increases the tendency of a specific protein to bind to
itself.
In this aggregated form, the protein is resistant to clearance and can
interfere with the normal capacity of the affected organs. In some
cases, misfolding of the protein results in a loss of its usual
function. For example, cystic fibrosis is caused by a defective cystic fibrosis transmembrane conductance regulator (CFTR) protein,
and in amyotrophic lateral sclerosis / frontotemporal lobar
degeneration (FTLD), certain gene-regulating proteins inappropriately
aggregate in the cytoplasm, and thus are unable to perform their normal
tasks within the nucleus. Because proteins share a common structural feature known as the polypeptide backbone, all proteins have the potential to misfold under some circumstances.
However, only a relatively small number of proteins are linked to
proteopathic disorders, possibly due to structural idiosyncrasies of the
vulnerable proteins. For example, proteins that are normally unfolded
or relatively unstable as monomers (that is, as single, unbound protein molecules) are more likely to misfold into an abnormal conformation. In nearly all instances, the disease-causing molecular configuration involves an increase in beta-sheet secondary structure of the protein.
The abnormal proteins in some proteopathies have been shown to fold
into multiple 3-dimensional shapes; these variant, proteinaceous
structures are defined by their different pathogenic, biochemical, and
conformational properties. They have been most thoroughly studied with regard to prion disease, and are referred to as protein strains.
Micrograph of immunostained α-synuclein (brown) in Lewy bodies (large clumps) and Lewy neurites (thread-like structures) in the cerebral cortex of a patient with Lewy body disease, a synucleinopathy. 40X microscope objective.
The likelihood that proteopathy will develop is increased by certain risk factors that promote the self-assembly of a protein. These include destabilizing changes in the primary amino acid sequence of the protein, post-translational modifications (such as hyperphosphorylation), changes in temperature or pH, an increase in production of a protein, or a decrease in its clearance. Advancing age is a strong risk factor, as is traumatic brain injury. In the aging brain, multiple proteopathies can overlap. For example, in addition to tauopathy
and Aβ-amyloidosis (which coexist as key pathologic features of
Alzheimer's disease), many Alzheimer patients have concomitant
synucleinopathy (Lewy bodies) in the brain.
It is hypothesized that chaperones and co-chaperones (proteins that assist protein folding) may antagonize proteotoxicity during aging and in protein misfolding-diseases to maintain proteostasis.
Seeded induction
Some
proteins can be induced to form abnormal assemblies by exposure to the
same (or similar) protein that has folded into a disease-causing
conformation, a process called 'seeding' or 'permissive templating'. In this way, the disease state can be brought about in a susceptible host by the introduction of diseased tissue extract from an afflicted donor. The best known form of such inducible proteopathy is prion disease, which can be transmitted by exposure of a host organism to purified prion protein in a disease-causing conformation. There is now evidence that other proteopathies can be induced by a similar mechanism, including Aβ amyloidosis, amyloid A (AA) amyloidosis, and apolipoprotein AII amyloidosis, tauopathy, synucleinopathy, and the aggregation of superoxide dismutase-1 (SOD1), polyglutamine, and TAR DNA-binding protein-43 (TDP-43).
In all of these instances, an aberrant form of the protein itself
appears to be the pathogenic agent. In some cases, the deposition of
one type of protein can be experimentally induced by aggregated
assemblies of other proteins that are rich in β-sheet structure,
possibly because of structural complementarity of the protein molecules.
For example, AA amyloidosis can be stimulated in mice by such diverse macromolecules as silk, the yeast amyloid Sup35, and curli fibrils from the bacterium Escherichia coli. In addition, apolipoprotein AII amyloid can be induced in mice by a variety of β-sheet rich amyloid fibrils, and cerebral tauopathy can be induced by brain extracts that are rich in aggregated Aβ. There is also experimental evidence for cross-seeding between prion protein and Aβ. In general, such heterologous seeding is less efficient than is seeding by a corrupted form of the same protein.
List of proteopathies
Management
The development of effective treatments for many proteopathies has been challenging.
Because the proteopathies often involve different proteins arising from
different sources, treatment strategies must be customized to each
disorder; however, general therapeutic approaches include maintaining
the function of affected organs, reducing the formation of the
disease-causing proteins, preventing the proteins from misfolding and/or
aggregating, or promoting their removal.
For example, in Alzheimer's disease, researchers are seeking ways to
reduce the production of the disease-associated protein Aβ by inhibiting
the enzymes that free it from its parent protein. Another strategy is to use antibodies to neutralize specific proteins by active or passive immunization. In some proteopathies, inhibiting the toxic effects of protein oligomers might be beneficial. Amyloid A (AA) amyloidosis can be reduced by treating the inflammatory state that increases the amount of the protein in the blood (referred to as serum amyloid A, or SAA). In immunoglobulin light chain amyloidosis (AL amyloidosis), chemotherapy
can be used to lower the number of the blood cells that make the light
chain protein that forms amyloid in various bodily organs. Transthyretin (TTR) amyloidosis (ATTR) results from the deposition of misfolded TTR in multiple organs. Because TTR is mainly produced in the liver, TTR amyloidosis can be slowed in some hereditary cases by liver transplantation. TTR amyloidosis also can be treated by stabilizing the normal assemblies of the protein (called tetramers because they consist of four TTR molecules bound together). Stabilization prevents individual TTR molecules from escaping, misfolding, and aggregating into amyloid.
Several other treatment strategies for proteopathies are being investigated, including small molecules and biologic medicines such as small interfering RNAs, antisense oligonucleotides, peptides, and engineered immune cells. In some cases, multiple therapeutic agents may be combined to improve effectiveness.