https://en.wikipedia.org/wiki/Sertraline
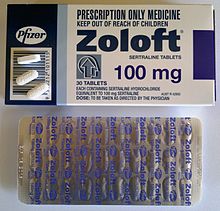
Sertraline, sold under the trade name Zoloft among others, is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. It is used to treat major depressive disorder, obsessive–compulsive disorder, panic disorder, post-traumatic stress disorder, premenstrual dysphoric disorder, and social anxiety disorder. Sertraline is taken by mouth.
Common side effects include diarrhea, sexual dysfunction, and troubles with sleep. Serious side effects include an increased risk of suicide in those less than 25 years old and serotonin syndrome. It is unclear whether use during pregnancy or breastfeeding is safe. It should not be used together with MAO inhibitor medication. Sertraline is believed to work by increasing serotonin effects in the brain.
Sertraline was approved for medical use in the United States in 1991 and initially sold by Pfizer. It is currently available as a generic medication. In the United States, the wholesale cost is about US$1.50 per month as of 2018. In 2016, it was the most prescribed psychiatric medication in the United States, with over 37 million prescriptions.
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˈsərtrəˌliːn/ |
| Trade names | Zoloft and others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697048 |
| Pregnancy category | |
| Addiction liability | None |
| Routes of administration | By mouth (tablets and solution) |
| Drug class | Selective serotonin reuptake inhibitor |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 44% |
| Protein binding | 98.5% |
| Metabolism | Hepatic (N-demethylation mainly by CYP2B6) |
| Metabolites | norsertraline |
| Elimination half-life | ~23–26 h (66 h [less-active metabolite, norsertraline]) |
| Excretion | Renal |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
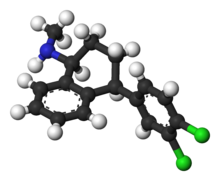
| Formula | C17H17Cl2N |
| Molar mass | 306.229 g/mol g·mol−1 |
| 3D model (JSmol) | |
Sertraline, sold under the trade name Zoloft among others, is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. It is used to treat major depressive disorder, obsessive–compulsive disorder, panic disorder, post-traumatic stress disorder, premenstrual dysphoric disorder, and social anxiety disorder. Sertraline is taken by mouth.
Common side effects include diarrhea, sexual dysfunction, and troubles with sleep. Serious side effects include an increased risk of suicide in those less than 25 years old and serotonin syndrome. It is unclear whether use during pregnancy or breastfeeding is safe. It should not be used together with MAO inhibitor medication. Sertraline is believed to work by increasing serotonin effects in the brain.
Sertraline was approved for medical use in the United States in 1991 and initially sold by Pfizer. It is currently available as a generic medication. In the United States, the wholesale cost is about US$1.50 per month as of 2018. In 2016, it was the most prescribed psychiatric medication in the United States, with over 37 million prescriptions.
Medical uses
Sertraline is used for a number of conditions, including major depressive disorder (MDD), obsessive–compulsive disorder (OCD), body dysmorphic disorder (BDD), posttraumatic stress disorder (PTSD), premenstrual dysphoric disorder (PMDD), panic disorder, and social anxiety disorder (SAD). It has also been used for premature ejaculation and vascular headaches but evidence of the effectiveness in treating those conditions is not robust. Sertraline is not approved for use in children except for those with OCD.
Depression
It is unclear if sertraline is any different from another SSRI, paroxetine, for depression; though escitalopram may have some benefits over sertraline.
Evidence does not show a benefit in children with depression.
With depression in dementia, there is no benefit compared to either placebo or mirtazapine.
Comparison with other antidepressants
Tricyclic antidepressants (TCAs) as a group are considered to work better than SSRIs for melancholic depression and in inpatients, but not necessarily for simply more severe depression. In line with this generalization, sertraline was no better than placebo in inpatients and as effective as the TCA clomipramine for severe depression.
The comparative efficacy of sertraline and TCAs for melancholic
depression has not been studied. A 1998 review suggested that, due to
its pharmacology, sertraline may be more efficacious than other SSRIs
and equal to TCAs for the treatment of melancholic depression.
A meta-analysis of 12 new-generation antidepressants showed that sertraline and escitalopram are the best in terms of efficacy and acceptability in the acute-phase treatment of adults with unipolar MDD. Reboxetine was significantly worse.
Comparative clinical trials demonstrated that sertraline is similar in efficacy against depression to moclobemide, nefazodone, escitalopram, bupropion, citalopram, fluvoxamine, paroxetine, and mirtazapine. There is low quality evidence that sertraline is more efficacious for the treatment of depression than fluoxetine.
Elderly
Sertraline used for the treatment of depression in elderly (older than 60) patients was superior to placebo and comparable to another SSRI fluoxetine, and TCAs amitriptyline, nortriptyline (Pamelor) and imipramine.
Sertraline had much lower rates of adverse effects than these TCAs,
with the exception of nausea, which occurred more frequently with
sertraline. In addition, sertraline appeared to be more effective than
fluoxetine or nortriptyline in the older-than-70 subgroup. A 2003 trial of sertraline vs. placebo in elderly patients showed a statistically significant (that is, unlikely to occur by chance), but clinically very modest improvement in depression and no improvement in quality of life.
A meta-analysis on SSRIs and SNRIs that look at partial response
(defined as at least a 50% reduction in depression score from baseline)
found that sertraline, paroxetine and duloxetine were better than
placebo.
Obsessive–compulsive disorder
Sertraline is effective for the treatment of OCD in adults and children. It was better tolerated and, based on intention to treat analysis, performed better than the gold standard of OCD treatment clomipramine.
It is generally accepted that the sertraline dosages necessary for the
effective treatment of OCD are higher than the usual dosage for
depression. The onset of action is also slower for OCD than for depression.
Cognitive behavioral therapy
alone was superior to sertraline in both adults and children; however,
the best results were achieved using a combination of these treatments.
Panic disorder
Treatment of panic disorder with sertraline results in a decrease of the number of panic attacks and an improved quality of life. In four double-blind studies sertraline was shown to be superior to placebo
for the treatment of panic disorder. The response rate was independent
of the dose. In addition to decreasing the frequency of panic attacks by
about 80% (vs. 45% for placebo) and decreasing general anxiety,
sertraline resulted in improvement of quality of life on most
parameters. The patients rated as "improved" on sertraline reported
better quality of life than the ones who "improved" on placebo. The
authors of the study argued that the improvement achieved with
sertraline is different and of a better quality than the improvement
achieved with placebo. Sertraline was equally effective for men and women. While imprecise, comparison of the results of trials of sertraline with separate trials of other anti-panic agents (clomipramine, imipramine, clonazepam, alprazolam, fluvoxamine and paroxetine) indicates approximate equivalence of these medications.
Other anxiety disorders
Sertraline is effective for the treatment of social phobia. Improvement in scores on the Liebowitz Social Anxiety Scale were found with sertraline but not with placebo. In children, a combination of sertraline and cognitive behavioural therapy
had a superior response rate to each intervention alone, and both
sertraline and CBT were alone superior to placebo and not significantly
different from one another.
There is tentative evidence that sertraline, as well as other SSRI/SNRI antidepressants, can help with the symptoms of general anxiety disorder.
The trials have generally been short in length (6–12 weeks) and
pharmacological treatments are associated with more frequent side
effects.
Premenstrual dysphoric disorder
SSRIs, including sertraline, reduce the symptoms of premenstrual syndrome. Side effects such as nausea are common. Sertraline is effective in alleviating the symptoms of premenstrual dysphoric disorder (PMDD), a severe form of premenstrual syndrome.
Significant improvement was observed in 50–60% of cases treated with
sertraline vs. 20–30% of cases on placebo. The improvement began during
the first week of treatment, and in addition to mood, irritability, and
anxiety, improvement was reflected in better family functioning, social
activity and general quality of life. Work functioning and physical
symptoms, such as swelling, bloating and breast tenderness, were less
responsive to sertraline. Taking sertraline only during the luteal phase, that is, the 12–14 days before menses, was shown to work as well as continuous treatment.
Other indications
Sertraline when taken daily can be useful for the treatment of some aspects of premature ejaculation. A disadvantage of SSRIs is that they require continuous daily treatment to delay ejaculation significantly,
and it is not clear how they affect psychological distress of those
with the condition or the person's control over ejaculation timing.
The benefit of sertraline in PTSD is not significant per the National Institute of Clinical Excellence. Others, however, do feel that there is a benefit from its use.
Side effects
Zoloft 50 mg & 25 mg tablets (US)
Zoloft 100 mg tablets (AU)
Compared to other SSRIs, sertraline tends to be associated with a higher rate of psychiatric side effects and diarrhea.
It tends to be more activating (that is, associated with a higher rate
of anxiety, agitation, insomnia, etc.) than other SSRIs, aside from fluoxetine.
Over more than six months of sertraline therapy for depression, people showed a nonsignificant weight increase of 0.1%. Similarly, a 30-month-long treatment with sertraline for OCD resulted in a mean weight gain of 1.5% (1 kg). Although the difference did not reach statistical significance, the weight gain was lower for fluoxetine (1%) but higher for citalopram, fluvoxamine and paroxetine
(2.5%). Of the sertraline group, 4.5% gained a large amount of weight
(defined as more than 7% gain). This result compares favorably with
placebo, where, according to the literature, 3–6% of patients gained
more than 7% of their initial weight. The large weight gain was observed
only among female members of the sertraline group; the significance of
this finding is unclear because of the small size of the group. The incidence of diarrhea is higher with sertraline—especially when prescribed at higher doses—in comparison to other SSRIs.
Over a two-week treatment of healthy volunteers, sertraline slightly improved verbal fluency but did not affect word learning, short-term memory, vigilance, flicker fusion time, choice reaction time, memory span, or psychomotor coordination.[58][59]
In spite of lower subjective rating, that is, feeling that they
performed worse, no clinically relevant differences were observed in the
objective cognitive performance in a group of people treated for
depression with sertraline for 1.5 years as compared to healthy
controls.[60]
In children and adolescents taking sertraline for six weeks for anxiety
disorders, 18 out of 20 measures of memory, attention and alertness
stayed unchanged. Divided attention was improved and verbal memory under interference conditions
decreased marginally. Because of the large number of measures taken, it
is possible that these changes were still due to chance. The unique effect of sertraline on dopaminergic neurotransmission may be related to these effects on cognition and vigilance. Sertraline's effect on the dopaminergic system may explain the risk of oromandibular dystonia.
Sexual
Like other SSRIs, sertraline is associated with sexual side effects, including sexual arousal disorder and difficulty achieving orgasm.
The frequency of sexual side effects depends on whether they are
reported by people spontaneously, as in the manufacturer's trials, or
actively solicited by physicians. While nefazodone, bupropion, and reboxetine
do not have negative effects on sexual functioning, 67% of men on
sertraline experienced ejaculation difficulties versus 18% before the
treatment. Sexual arousal
disorder, defined as "inadequate lubrication and swelling for women and
erectile difficulties for men", occurred in 12% of people on sertraline
as compared with 1% of patients on placebo. The mood improvement
resulting from the treatment with sertraline sometimes counteracted
these side effects, so that sexual desire
and overall satisfaction with sex stayed the same as before the
sertraline treatment. However, under the action of placebo the desire
and satisfaction slightly improved.
Some people experience persistent sexual side effects after they stop taking SSRIs.
This is known as Post-SSRI Sexual Dysfunction (PSSD). Common symptoms
in these cases include genital anesthesia, erectile dysfunction, anhedonia,
decreased libido, premature ejaculation, vaginal lubrication issues,
and nipple insensitivity in women. Rates of PSSD are unknown, and there
is no established treatment.
Pregnancy
Antidepressant
exposure (including sertraline) is associated with shorter average
duration of pregnancy (by three days), increased risk of preterm
delivery (by 55%), lower birth weight (by 75 g), and lower Apgar scores (by <0 .4="" among="" an="" children="" defects="" early="" heart="" in="" increased="" is="" it="" mothers="" of="" p="" points="" pregnancy.="" prescribed="" rate="" septal="" ssri="" there="" uncertain="" were="" whether="" whose="">
Suicide
The FDA requires all antidepressants, including sertraline, to carry a boxed warning
stating that antidepressants may increase the risk of suicide in
persons younger than 25 years. This warning is based on statistical
analyses conducted by two independent groups of FDA experts that found a
100% increase of suicidal ideation and behavior in children and
adolescents, and a 50% increase of suicidal behavior in the 18–24 age
group.
Suicidal ideation
and behavior in clinical trials are rare. For the above analysis, the
FDA combined the results of 295 trials of 11 antidepressants for
psychiatric indications in order to obtain statistically significant
results. Considered separately, sertraline use in adults decreased the
odds of suicidal behavior with a marginal statistical significance by
37% or 50%
depending on the statistical technique used. The authors of the FDA
analysis note that "given the large number of comparisons made in this
review, chance is a very plausible explanation for this difference". The more complete data submitted later by the sertraline manufacturer Pfizer indicated increased suicidal behavior. Similarly, the analysis conducted by the UK MHRA
found a 50% increase of odds of suicide-related events, not reaching
statistical significance, in the patients on sertraline as compared to
the ones on placebo.
Concerns have been raised that suicidal acts among participants
in multiple studies were not reported in published articles reporting
the studies.
Discontinuation syndrome
Antidepressant discontinuation syndrome is a condition that can occur
following the interruption, dose reduction, or discontinuation of
antidepressant drugs, including sertraline. The symptoms can include
flu-like symptoms, "brain zaps," and disturbances in sleep, senses,
movement, mood, and thinking. In most cases symptoms are mild,
short-lived, and resolve without treatment. More severe cases are often
successfully treated by temporary reintroduction of the drug with a
slower tapering off rate.
Overdose
Acute
overdosage is often manifested by emesis, lethargy, ataxia, tachycardia
and seizures. Plasma, serum or blood concentrations of sertraline and
norsertraline, its major active metabolite,
may be measured to confirm a diagnosis of poisoning in hospitalized
patients or to aid in the medicolegal investigation of fatalities. As with most other SSRIs its toxicity in overdose is considered relatively low.
Interactions
Sertraline is a moderate inhibitor of CYP2D6 and CYP2B6 in vitro. Accordingly, in human trials it caused increased blood levels of CYP2D6 substrates such as metoprolol, dextromethorphan, desipramine, imipramine and nortriptyline, as well as the CYP3A4/CYP2D6 substrate haloperidol. This effect is dose-dependent. In a placebo-controlled study, the concomitant administration of sertraline and methadone caused a 40% increase in blood levels of the latter, which is primarily metabolized by CYP2B6. Sertraline is often used in combination with stimulant medication for the treatment of co-morbid depression and/or anxiety in ADHD. Amphetamine metabolism inhibits enzyme CYP2D6, but has not been known to interfere with Sertraline metabolism.
Sertraline had a slight inhibitory effect on the metabolism of diazepam, tolbutamide and warfarin, which are CYP2C9 or CYP2C19 substrates; this effect was not considered to be clinically relevant.[7] As expected from in vitro data, sertraline did not alter the human metabolism of the CYP3A4 substrates erythromycin, alprazolam, carbamazepine, clonazepam, and terfenadine; neither did it affect metabolism of the CYP1A2 substrate clozapine.
Sertraline had no effect on the actions of digoxin and atenolol, which are not metabolized in the liver. Case reports suggest that taking sertraline with phenytoin or zolpidem may induce sertraline metabolism and decrease its efficacy, and that taking sertraline with lamotrigine may increase the blood level of lamotrigine, possibly by inhibition of glucuronidation.
Clinical reports indicate that interaction between sertraline and the MAOIs isocarboxazid and tranylcypromine may cause serotonin syndrome. In a placebo-controlled study in which sertraline was co-administered with lithium, 35% of the subjects experienced tremors, while none of those taking placebo did.
According to the label, sertraline is contraindicated in individuals taking monoamine oxidase inhibitors or the antipsychotic pimozide (Orap). Sertraline concentrate contains alcohol, and is therefore contraindicated with disulfiram (Antabuse).
The prescribing information recommends that treatment of the elderly
and patients with liver impairment "must be approached with caution."
Due to the slower elimination of sertraline in these groups, their
exposure to sertraline may be as high as three times the average
exposure for the same dose.
Pharmacology
Sertraline is a selective serotonin re-uptake inhibitor.
It targets the sodium dependent serotonin transporter to inhibit the
re-uptake of serotonin by neurons. This increases the concentration of
serotonin in the synaptic cleft, meaning more is available to act on the
post synaptic neurons resulting in antidepressant effects.
Sertraline does not inhibit noradrenalin re-uptake, has little
anticholinergic activity and has less sedative and cardiovascular
effects than tricyclic antidepressant drugs.
Mechanism of action
| Site | Ki (nM) | Species | ||
|---|---|---|---|---|
| SERT | 0.4 2.8 (IC50) |
Human | ||
| NET | 420–817 925 (IC50) |
Human | ||
| DAT | 22–25 315 (IC50) |
Human | ||
| 5-HT1A | >35,000 | Human | ||
| 5-HT2A | 2,207 | Rat | ||
| 5-HT2C | 2,298 | Pig | ||
| α1 | 36–480 | Human | ||
| α2 | 477–4,100 | Human | ||
| D2 | 10,700 | Human | ||
| H1 | 24,000 | Human | ||
| mACh | 427–2,100 | Human | ||
| σ1 | 32–57 | Rat | ||
| σ2 | 5,297 | Rat | ||
| Values are Ki (nM), unless otherwise noted. The smaller the value, the more strongly the drug binds to or inhibits the site. | ||||
Sertraline acts as a potent serotonin reuptake inhibitor (SRI), with an affinity (Ki) for the serotonin transporter (SERT) of 0.4 nM and an IC50 value of 2.8 nM, according to a couple of studies. It is highly selective in its inhibition of serotonin reuptake. By inhibiting the reuptake of serotonin, sertraline increases extracellular levels of serotonin and thereby increases serotonergic neurotransmission in the brain. It is this action that is thought to be responsible for the antidepressant, anxiolytic, and antiobsessional effects of sertraline.
Sertraline does not have significant affinity for the norepinephrine transporter (NET) or the serotonin, dopamine, adrenergic, histamine, or acetylcholine receptors. On the other hand, it does show high affinity for the dopamine transporter (DAT) and the sigma σ1 receptor (but not the σ2 receptor). However, its affinities for these sites are around 100-fold or lower than for the SERT.
Dopamine reuptake inhibition
Sertraline is an SSRI, but, uniquely among most antidepressants, it shows relatively high (nanomolar) affinity for the DAT in addition to the SERT. As such, it has been suggested that clinically it may weakly inhibit the reuptake of dopamine, particularly at high dosages. For this reason, sertraline has sometimes been described as a serotonin–dopamine reuptake inhibitor (SDRI). This is relevant as dopamine is thought to be involved in the pathophysiology
of depression, and increased dopaminergic neurotransmission by
sertraline in addition to serotonin may have additional benefits against
depression.
Tatsumi et al. (1997) found Ki values of sertraline at the human SERT, DAT, and NET of 0.29, 25, and 420 nM, respectively. The selectivity of sertraline for the SERT over the DAT was 86-fold.
In any case, of the wide assortment of antidepressants assessed in the
study, sertraline showed the highest affinity of them all for the DAT,
even higher than the norepinephrine–dopamine reuptake inhibitors (NDRIs) nomifensine (Ki = 56 nM) and bupropion (Ki = 520 nM). Sertraline also has similar affinity for the DAT as the NDRI methylphenidate (Ki = 24 nM). Tametraline (CP-24,441), a very close analogue of sertraline and the compound from which sertraline was originally derived, is an NDRI that was never marketed.
Single doses of 50 to 200 mg sertraline have been found to result in peak plasma concentrations of 20 to 55 ng/mL (65–180 nM),
while chronic treatment with 200 mg/day sertraline, the maximum
recommended dosage, has been found to result in maximal plasma levels of
118 to 166 ng/mL (385–542 nM). However, sertraline is highly protein-bound in plasma, with a bound fraction of 98.5%. Hence, only 1.5% is free and theoretically bioactive.
Based on this percentage, free concentrations of sertraline would be
2.49 ng/mL (8.13 nM) at the very most, which is only about one-third of
the Ki value that Tatsumi et al. found with sertraline at the DAT.
A very high dosage of sertraline of 400 mg/day has been found to
produce peak plasma concentrations of about 250 ng/mL (816 nM).[7] This can be estimated to result in a free concentration of 3.75 ng/mL (12.2 nM), which is still only about half of the Ki of sertraline for the DAT.
As such, it seems unlikely that sertraline would produce much
inhibition of dopamine reuptake even at clinically used dosages well in
excess of the recommended maximum clinical dosage.
This is in accordance with its 86-fold selectivity for the SERT over
the DAT according to Tatsumi et al. and hence the fact that nearly
100-fold higher levels of sertraline would be necessary to also inhibit
dopamine reuptake. In accordance, while sertraline has very low abuse potential and may even be aversive at clinical dosages, a case report of sertraline abuse described dopaminergic-like effects such as euphoria, mental overactivity, and hallucinations only at a dosage 56 times the normal maximum and 224 times the normal minimum.
For these reasons, significant inhibition of dopamine reuptake by
sertraline at clinical dosages is controversial, and occupation by
sertraline of the DAT is thought by many experts to not be clinically
relevant.
Sigma receptor antagonism
Sertraline has relatively high (nanomolar) affinity for the sigma σ1 receptor. Conversely, it has low (micromolar) and insignificant affinity for the σ2 receptor. It acts as an antagonist of the σ1 receptor, and is able to reverse σ1 receptor-dependent actions of fluvoxamine, a potent agonist of the receptor, in vitro. However, the affinity of sertraline for the σ1 receptor is more than 100-fold lower than for the SERT. Although there could be a role for the σ1 receptor in the pharmacology of sertraline, the significance of this receptor in its actions is unclear and perhaps questionable.
Sertraline is associated with a significantly higher incidence of diarrhea than other SSRIs, especially at higher doses. Agonists of the σ1 receptor such as igmesine have been found to inhibit intestinal secretion and bacteria-induced secretory diarrhea in animal studies, and igmesine showed preliminary evidence of efficacy for the treatment of diarrhea in a small clinical trial. Sertraline is the only SSRI that acts as an antagonist of the σ1 receptor, so this action could in theory be responsible for its higher relative incidence of diarrhea.
Neurosteroidogenesis enhancement
Sertraline has been found to directly act on the enzyme 3α-hydroxysteroid dehydrogenase (3α-HSD) and modulate its activity, thereby enhancing the conversion of 5α-dihydroprogesterone into the neurosteroid allopregnanolone and thus increasing the production of allopregnanolone in the brain. The same is true for certain other SSRIs including fluoxetine and paroxetine. However, a subsequent study failed to reproduce these findings, and a direct interaction of SSRIs with 3α-HSD is controversial. In any case, another study found that, at least in the case of fluoxetine and its active metabolite norfluoxetine,
these drugs normalized low allopregnanolone levels in socially isolated
mice and at low doses that were inactive on serotonin reuptake (10- to
50-fold lower, specifically). On the basis of these results, SSRIs like fluoxetine and norfluoxetine were described as selective brain steroidogenic stimulants (SBSSs).
Pharmacokinetics
Norsertraline (desmethylsertraline)—sertraline's chief active metabolite
Sertraline is absorbed slowly when taken orally, achieving its
maximal concentration in the plasma 4 to 6 hours after ingestion. In the
blood, it is 98.5% bound to plasma proteins and a half life of 25 to 26 hours. Sertraline is metabolised in the liver by demethylation to an inactive metabolite. According to in vitro studies, sertraline is metabolized by multiple cytochrome 450 isoforms: CYP2D6, CYP2C9, CYP2B6, CYP2C19 and CYP3A4.
It appeared unlikely that inhibition of any single isoform could cause
clinically significant changes in sertraline pharmacokinetics. No differences in sertraline pharmacokinetics were observed between people with high and low activity of CYP2D6; however, poor CYP2C19 metabolizers had a 1.5-times-higher level of sertraline than normal metabolizers. In vitro
data also indicate that the inhibition of CYP2B6 should have even
greater effect than the inhibition of CYP2C19, while the contribution of
CYP2C9 and CYP3A4 to the metabolism of sertraline would be minor. These conclusions have not been verified in human studies. Sertraline can be deaminated in vitro by monoamine oxidases; however, this metabolic pathway has never been studied in vivo. The major metabolite of sertraline, desmethylsertraline, is about 50 times weaker as a serotonin transporter inhibitor than sertraline and its clinical effect is negligible.
Non-amine metabolites may also contribute to the antidepressant effects of this medication. Sertraline deaminated is O-2098, a compound that has been found to inhibit the dopamine reuptake transporter proteins in spite of its lack of a nitrogen atom.
Its chief active metabolite is norsertraline (N-desmethylsertraline) which is significantly less biologically active than its parent compound.
Metabolism of sertraline in human liver microsomes.
History
Skeletal formulae of chlorprothixene and tametraline, from which sertraline was derived
The history of sertraline dates back to the early 1970s, when Pfizer chemist Reinhard Sarges invented a novel series of psychoactive compounds based on the structure of the neuroleptic chlorprothixene. Further work on these compounds led to lometraline and then to tametraline, a norepinephrine and weaker dopamine reuptake inhibitor. Development of tametraline was soon stopped because of undesired stimulant effects observed in animals. A few years later, in 1977, pharmacologist Kenneth Koe,
after comparing the structural features of a variety of reuptake
inhibitors, became interested in the tametraline series. He asked
another Pfizer chemist, Willard Welch, to synthesize some previously
unexplored tametraline derivatives. Welch generated a number of potent
norepinephrine and triple reuptake inhibitors, but to the surprise of the scientists, one representative of the generally inactive cis-analogs was a serotonin reuptake inhibitor. Welch then prepared stereoisomers of this compound, which were tested in vivo by animal behavioral scientist
Albert Weissman. The most potent and selective (+)-isomer was taken
into further development and eventually named sertraline. Weissman and
Koe recalled that the group did not set up to produce an antidepressant
of the SSRI type—in that sense their inquiry was not "very goal driven",
and the discovery of the sertraline molecule was serendipitous.
According to Welch, they worked outside the mainstream at Pfizer, and
even "did not have a formal project team". The group had to overcome
initial bureaucratic reluctance to pursue sertraline development, as
Pfizer was considering licensing an antidepressant candidate from
another company.
Sertraline was approved by the U.S. Food and Drug Administration
(FDA) in 1991 based on the recommendation of the Psychopharmacological
Drugs Advisory Committee; it had already become available in the United Kingdom the previous year. The FDA committee achieved a consensus that sertraline was safe and effective for the treatment of MDD.
Sertraline entered the Australian market in 1994 and became the most often prescribed antidepressant in 1996 (2004 data).
It was measured as among the top ten drugs ranked by cost to the
Australian government in 1998 and 2000–01, having cost $45 million and
$87 million in subsidies respectively.
Sertraline is less popular in the UK (2003 data) and Canada (2006
data)—in both countries it was fifth (among drugs marketed for the
treatment of MDD, or antidepressants), based on the number of
prescriptions.
Until 2002, sertraline was only approved for use in adults ages
18 and over; that year, it was approved by the FDA for use in treating
children aged 6 or older with severe OCD. In 2003, the U.K. Medicines and Healthcare products Regulatory Agency issued a guidance that, apart from fluoxetine (Prozac), SSRIs are not suitable for the treatment of depression in patients under 18. However, sertraline can still be used in the UK for the treatment of OCD in children and adolescents. In 2005, the FDA added a boxed warning concerning pediatric suicidal behavior to all antidepressants,
including sertraline. In 2007, labeling was again changed to add a
warning regarding suicidal behavior in young adults ages 18 to 24.
Society and culture
Generic availability
The U.S. patent for Zoloft expired in 2006, and sertraline is now available in generic form and is marketed under many brand names worldwide.