| Pesticide toxicity | |
|---|---|
 | |
| A sign warning about potential pesticide exposure. | |
| Specialty | Emergency medicine, toxicology |
A pesticide poisoning occurs when chemicals intended to control a pest affect non-target organisms such as humans, wildlife, or bees. There are three types of pesticide poisoning. The first of the three is a single and short-term very high level of exposure which can be experienced by individuals who commit suicide, as well as pesticide formulators. The second type of poisoning is long-term high-level exposure, which can occur in pesticide formulators and manufacturers. The third type of poisoning is a long-term low-level exposure, which individuals are exposed to from sources such as pesticide residues in food as well as contact with pesticide residues in the air, water, soil, sediment, food materials, plants and animals.
In developing countries, such as Sri Lanka, pesticide poisonings from short-term very high level of exposure (acute poisoning) is the most worrisome type of poisoning. However, in developed countries, such as Canada, it is the complete opposite: acute pesticide poisoning is controlled, thus making the main issue long-term low-level exposure of pesticides.
Cause
The most common exposure scenarios for pesticide-poisoning cases are accidental or suicidal poisonings, occupational exposure, by-stander exposure to off-target drift, and the general public who are exposed through environmental contamination.
Accidental or suicidal
Self-poisoning
with agricultural pesticides represents a major hidden public health
problem accounting for approximately one-third of all suicides
worldwide. It is one of the most common forms of self-injury in the Global South. The World Health Organization estimates that 300,000 people die from self-harm each year in the Asia-Pacific region alone.
Most cases of intentional pesticide poisoning appear to be impulsive
acts undertaken during stressful events, and the availability of
pesticides strongly influences the incidence of self poisoning.
Pesticides are the agents most frequently used by farmers and students
in India to commit suicide.
Occupational
Pesticide
poisoning is an important occupational health issue because pesticides
are used in a large number of industries, which puts many different
categories of workers at risk. Extensive use puts agricultural workers
in particular at increased risk for pesticide illnesses.
Exposure can occur through inhalation of pesticide fumes, and often
occurs in settings including greenhouse spraying operations and other
closed environments like tractor cabs or while operating rotary fan mist
sprayers in facilities or locations with poor ventilation systems.
Workers in other industries are at risk for exposure as well.
For example, commercial availability of pesticides in stores puts
retail workers at risk for exposure and illness when they handle
pesticide products. The ubiquity of pesticides puts emergency responders such as fire-fighters and police officers
at risk, because they are often the first responders to emergency
events and may be unaware of the presence of a poisoning hazard. The process of aircraft disinsection,
in which pesticides are used on inbound international flights for
insect and disease control, can also make flight attendants sick.
Different job functions can lead to different levels of exposure.
Most occupational exposures are caused by absorption through exposed
skin such as the face, hands, forearms, neck, and chest. This exposure
is sometimes enhanced by inhalation in settings including spraying
operations in greenhouses and other closed environments, tractor cabs,
and the operation of rotary fan mist sprayers.
Residential
When
thinking of pesticide poisoning, one does not take into consideration
the contribution that is made of their own household. The majority of
households in Canada use pesticides while taking part in activities such
as gardening. In Canada 96 percent of households report having a lawn
or a garden. 56 percent of the households who have a lawn or a garden utilize fertilizer or pesticide. This form of pesticide use may contribute to the third type of poisoning, which is caused by long-term low-level exposure.
As mentioned before, long-term low-level exposure affects individuals
from sources such as pesticide residues in food as well as contact with
pesticide residues in the air, water, soil, sediment, food materials,
plants and animals.
Pathophysiology
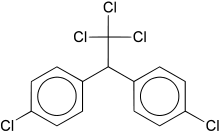
Organochlorines
DDT, an organochlorine
The organochlorine pesticides, like DDT, aldrin, and dieldrin,
are extremely persistent and accumulate in fatty tissue. Through the
process of bioaccumulation (lower amounts in the environment get
magnified sequentially up the food chain), large amounts of
organochlorines can accumulate in top species like humans. There is substantial evidence to suggest that DDT, and its metabolite DDE, act as endocrine disruptors, interfering with hormonal function of estrogen, testosterone, and other steroid hormones.
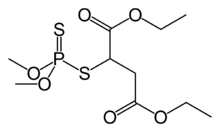
Anticholinesterase compounds
Malathion, an organophosphate anticholinesterase
Cholinesterase-inhibiting pesticides, also known as organophosphates, carbamates, and anticholinesterases, are most commonly reported in occupationally related pesticide poisonings globally. Besides acute symptoms including cholinergic crisis, certain organophosphates
have long been known to cause a delayed-onset toxicity to nerve cells,
which is often irreversible. Several studies have shown persistent
deficits in cognitive function in workers chronically exposed to
pesticides.
Diagnosis
Most
pesticide-related illnesses have signs and symptoms that are similar to
common medical conditions, so a complete and detailed environmental and
occupational history is essential for correctly diagnosing a pesticide
poisoning. A few additional screening questions about the patient's
work and home environment, in addition to a typical health
questionnaire, can indicate whether there was a potential pesticide
poisoning.
If one is regularly using carbamate and organophosphate pesticides, it is important to obtain a baseline cholinesterase
test. Cholinesterase is an important enzyme of the nervous system, and
these chemical groups kill pests and potentially injure or kill humans
by inhibiting cholinesterase.
If one has had a baseline test and later suspects a poisoning, one can
identify the extent of the problem by comparison of the current
cholinesterase level with the baseline level.
Prevention
Accidental
poisonings can be avoided by proper labeling and storage of containers.
When handling or applying pesticides, exposure can be significantly
reduced by protecting certain parts of the body where the skin shows
increased absorption, such as the scrotal region, underarms, face,
scalp, and hands. Safety protocols to reduce exposure include the use of personal protective equipment,
washing hands and exposed skin during as well as after work, changing
clothes between work shifts, and having first aid trainings and
protocols in place for workers.
Personal protective equipment for preventing pesticide exposure
includes the use of a respirator, goggles, and protective clothing,
which have all have been shown to reduce risk of developing
pesticide-induced diseases when handling pesticides.
A study found the risk of acute pesticide poisoning was reduced by 55%
in farmers who adopted extra personal protective measures and were
educated about both protective equipment and pesticide exposure risk.
Exposure can be significantly reduced when handling or applying
pesticides by protecting certain parts of the body where the skin shows
increased absorption, such as the scrotal region, underarms, face,
scalp, and hands. Using chemical-resistant gloves has been shown to reduce contamination by 33–86%.
Treatment
Specific
treatments for acute pesticide poisoning are often dependent on the
pesticide or class of pesticide responsible for the poisoning. However,
there are basic management techniques that are applicable to most acute
poisonings, including skin decontamination, airway protection, gastrointestinal decontamination, and seizure treatment.
Decontamination of the skin is performed while other life-saving
measures are taking place. Clothing is removed, the patient is showered
with soap and water, and the hair is shampooed to remove chemicals from
the skin and hair. The eyes are flushed with water for 10–15 minutes.
The patient is intubated and oxygen administered, if necessary. In
more severe cases, pulmonary ventilation must sometimes be supported
mechanically. Seizures are typically managed with lorazepam, phenytoin and phenobarbitol, or diazepam (particularly for organochlorine poisonings).
Gastric lavage is not recommended to be used routinely in
pesticide poisoning management, as clinical benefit has not been
confirmed in controlled studies; it is indicated only when the patient
has ingested a potentially life-threatening amount of poison and
presents within 60 minutes of ingestion.
An orogastric tube is inserted and the stomach is flushed with saline
to try to remove the poison. If the patient is neurologically
impaired, a cuffed endotracheal tube inserted beforehand for airway protection. Studies of poison recovery at 60 minutes have shown recovery of 8%–32%. However, there is also evidence that lavage may flush the material into the small intestine, increasing absorption. Lavage is contra-indicated in cases of hydrocarbon ingestion.
Activated charcoal is sometimes administered as it has been shown
to be successful with some pesticides. Studies have shown that it can
reduce the amount absorbed if given within 60 minutes, though there is not enough data to determine if it is effective if time from ingestion is prolonged. Syrup of ipecac
is not recommended for most pesticide poisonings because of potential
interference with other antidotes and regurgitation increasing exposure
of the esophagus and oral area to the pesticide.
Urinary alkalinisation has been used in acute poisonings from chlorophenoxy herbicides (such as 2,4-D, MCPA, 2,4,5-T and mecoprop); however, evidence to support its use is poor.
Epidemiology
Acute pesticide poisoning is a large-scale problem, especially in developing countries.
"Most estimates concerning the extent of acute pesticide
poisoning have been based on data from hospital admissions which would
include only the more serious cases. The latest estimate by a WHO task
group indicates that there may be 1 million serious unintentional
poisonings each year and in addition 2 million people hospitalized for
suicide attempts with pesticides. This necessarily reflects only a
fraction of the real problem. On the basis of a survey of self-reported
minor poisoning carried out in the Asian region, it is estimated that
there could be as many as 25 million agricultural workers in the
developing world suffering an episode of poisoning each year." In Canada in 2007 more than 6000 cases of acute pesticide poisoning occurred.
Estimating the numbers of chronic poisonings worldwide is more difficult.
Society and culture
Rachel Carson's Silent Spring brought about the first major wave of public concern over the chronic effects of pesticides.
In other animals
An
obvious side effect of using a chemical meant to kill is that one is
likely to kill more than just the desired organism. Contact with a
sprayed plant or "weed" can have an effect upon local wildlife, most
notably insects. A cause for concern is how pests, the reason for
pesticide use, are building up a resistance. Phytophagous insects are able to build up this resistance because they are easily capable of evolutionary diversification and adaptation.
The problem this presents is that in order to obtain the same desired
effect of the pesticides they have to be made increasingly stronger as
time goes on. Repercussions of the use of stronger pesticides on
vegetation has a negative result on the surrounding environment, but
also would contribute to consumers' long-term low-level exposure.