| Public health |
|---|
 |
Reproductive health, sexual health, or sexual and reproductive health (SRH) denotes the health of an individual's reproductive system and sexual well-being during all stages of their life.
The term can also be further defined more broadly within the framework of the World Health Organization's (WHO) definition of health―as "a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity"― to denote sexual well-being, encompassing the ability of an individual to have responsible, satisfying and safe sex and the freedom to decide if, when and how often to do so. UN agencies in particular define sexual and reproductive health as including both physical and psychological well-being vis-à-vis sexuality. A further interpretation includes access to sex education, access to safe, effective, affordable and acceptable methods of birth control, as well as access to appropriate health care services, as the ability of women to go safely through pregnancy and childbirth could provide couples with the best chance of having a healthy infant.
Individuals face inequalities in reproductive health services. Inequalities vary based on socioeconomic status, education level, age, ethnicity, religion, and resources available in their environment. Low income individuals may lack access to appropriate health services and/or knowledge of how to maintain reproductive health.
Overview
The WHO assessed in 2008 that "Reproductive and sexual ill-health accounts for 20% of the global burden of ill-health for women, and 14% for men." Reproductive health is a part of sexual and reproductive health and rights. According to the United Nations Population Fund (UNFPA), unmet needs for sexual and reproductive health deprive women of the right to make "crucial choices about their own bodies and futures", affecting family welfare. Women bear and usually nurture children, so their reproductive health is inseparable from gender equality. Denial of such rights also worsens poverty.
According to the American College of Obstetricians and Gynecologists, fertility starts to drop considerably around the age of 32, and around 37, it has a particularly deep nose dive. By age 44, chances of spontaneous pregnancy approach zero. As such, women are often told to have children before the age of 35, and pregnancy after 40 is considered a high risk. If pregnancy occurs after the age of 40 (geriatric pregnancy), the woman and baby will be monitored closely for:
- high blood pressure
- gestational diabetes
- birth defects (i.e. Down syndrome)
- miscarriage
- low birth weight
- ectopic pregnancy
Adolescent health
Adolescent health creates a major global burden and has a great deal of additional and diverse complications compared to adult reproductive health such as early pregnancy and parenting issues, difficulties accessing contraception and safe abortions, lack of healthcare access, and high rates of HIV, sexually transmitted infections and mental health issues. Each of those can be affected by outside political, economic and socio-cultural influences. For most adolescent females, they have yet to complete their body growth trajectories, therefore adding a pregnancy exposes them to a predisposition to complications. These complications range from anemia, malaria, HIV and other STIs, postpartum bleeding and other postpartum complications, mental health disorders such as depression and suicidal thoughts or attempts. In 2016, adolescent birth rates between the ages of 15-19 was 45 per 1000. In 2014, 1 in 3 experienced sexual violence, and there more than 1.2 million deaths. The top three leading causes of death in females between the ages of 15-19 are maternal conditions 10.1%, self-harm 9.6%, and road conditions 6.1%.
The causes for teenage pregnancy are vast and diverse. In developing countries, young women are pressured to marry for different reasons. One reason is to bear children to help with work, another on a dowry system to increase the families income, another is due to prearranged marriages. These reasons tie back to financial needs of girls' family, cultural norms, religious beliefs and external conflicts.
Adolescent pregnancy, especially in developing countries, carries increased health risks, and contributes to maintaining the cycle of poverty. The availability and type of sex education for teenagers varies in different parts of the world. LGBT teens may suffer additional problems if they live in places where homosexual activity is socially disapproved and/or illegal; in extreme cases there can be depression, social isolation and even suicide among LGBT youth.
Maternal health
99% of maternal deaths occur in developing countries, and in 25 years, the maternal mortality globally dropped to 44%. Statistically, a woman's chance of survival during childbirth is closely tied to her social economic status, access to healthcare, where she lives geographically, and cultural norms. To compare, a woman dies of complications from childbirth every minute in developing countries versus a total of 1% of total maternal mortality deaths in developed countries. Women in developing countries have little access to family planning services, different cultural practices, have lack of information, birthing attendants, prenatal care, birth control, postnatal care, lack of access to health care and are typically in poverty. In 2015, those in low-income countries had access to antenatal care visits averaged to 40% and were preventable. All these reasons led to an increase in the maternal mortality ratio (MMR).
One of the international Sustainable Development Goals developed by United Nations is to improve maternal health by a targeted 70 deaths per 100,000 live births by 2030. Most models of maternal health encompass family planning, preconception, prenatal, and postnatal care. All care after childbirth recovery is typically excluded, which includes pre-menopause and aging into old age. During childbirth, women typically die from severe bleeding, infections, high blood pressure during pregnancy, delivery complications, or an unsafe abortion. Other reasons can be regional such as complications related to diseases such as malaria and AIDS during pregnancy. The younger the women is when she gives birth, the more at risk her and her baby is for complications and possibly mortality.
There is a significant relationship between the quality of maternal services made available and the greater financial standings of a country. Sub-Saharan Africa and South Asia exemplify this as these regions are significantly deprived of medical staff and affordable health opportunities. Most countries provide for their health services through a combination of funding from government tax revenue and local households. Poorer nations or regions with extremely concentrated wealth can leave citizens on the margins uncared for or overlooked. However, the lack of proper leadership can result in a nation's public sectors being mishandled or poorly performing despite said nation's resources and standing. In addition, poorer nations funding their medical services through taxes places a greater financial burden on the public and effectively the mothers themselves. Responsibility and accountability on the part of mental health sectors are strongly emphasized as to what will remedy the poor quality of maternal health globally. The impact of different maternal health interventions across the globe stagger variously and are vastly uneven. This is the result of a lack of political and financial commitment to the issue as most safe motherhood programs internationally have to compete for significant funding. Some resolve that if global survival initiatives were promoted and properly funded it would prove to be mutually beneficial for the international community. Investing in maternal health would ultimately advance several issues such as: gender inequality, poverty and general global health standards. As it currently stands, pregnant women are subjugated to high financial costs throughout the duration of their term internationally that are highly taxing and strenuous.
In addition, if the woman and/or the man has a genetic disease, there is risk of these being passed on to the children. Birth control or technical solutions (assisted reproductive technology) can be an option then.
LGBT+ health
The sexual and reproductive health of LGBT+ people faces challenges through issues like the ongoing HIV pandemic, binary organisation of "men" and "women"'s reproductive health, alongside stigma and repression that limits LGBT+ people from accessing the heatlhcare they need.
Contraception
Access to reproductive health services is very poor in many countries. Women are often unable to access maternal health services due to lack of knowledge about the existence of such services or lack of freedom of movement. Some women are subjected to forced pregnancy and banned from leaving the home. In many countries, women are not allowed to leave home without a male relative or husband, and therefore their ability to access medical services is limited. Therefore, increasing women's autonomy is needed in order to improve reproductive health, however doing may require a cultural shift. According to the WHO, "All women need access to antenatal care in pregnancy, skilled care during childbirth, and care and support in the weeks after childbirth".
The fact that the law allows certain reproductive health services, it does not necessary ensure that such services are actually in use by the people. The availability of contraception, sterilization and abortion is dependent on laws, as well as social, cultural and religious norms. Some countries have liberal laws regarding these issues, but in practice it is very difficult to access such services due to doctors, pharmacists and other social and medical workers being conscientious objectors.
In developing regions of the world, there are about 214 million women who want to avoid pregnancy but are unable to use safe and effective family planning methods. When taken correctly, the combined oral contraceptive pill is over 99% effective at preventing pregnancy. However, it does not protect from sexually transmitted infections (STIs). Some methods, such as using condoms, achieve both protection from STIs and unwanted pregnancies. There are also natural family planning methods, which may be preferred by religious people, but some very conservative religious groups, such as the Quiverfull movement, oppose these methods too, because they advocate the maximization of procreation. One of the oldest ways to reduce unwanted pregnancy is coitus interruptus - still widely used in the developing world.
There are many types of contraceptives. One type of contraceptive includes barrier methods. One barrier method includes condoms for males and females. Both types stop sperm from entering the woman's uterus, thereby preventing pregnancy from occurring. Another type of contraception is the birth control pill, which stops ovulation from occurring by combining the chemicals progestin and estrogen. Many women use this method of contraception, however they discontinue using it equally as much as they use it. One reason for this is because of the side effects that may occur from using the pill, and because some health care providers do not take women's concerns about negative side effects seriously. The use of the birth control pill is common in western countries, and two forms of combined oral contraceptives are on the World Health Organization's List of Essential Medicines, the most important medications needed in a basic health system.
There are many objections to the use of birth control, both historically and in the present day. One argument against birth control usage states that there is no need for birth control to begin with. This argument was levied in 1968 when Richard Nixon was elected president, and the argument stated that since birth rates were at their lowest point since World War II ended, birth control was not necessary. Demographic planning arguments were also the basis of the population policy of Nicolae Ceaușescu in communist Romania, who adopted a very aggressive natalist policy which included outlawing abortion and contraception, routine pregnancy tests for women, taxes on childlessness, and legal discrimination against childless people. Such policies consider that coercion is an acceptable means of reaching demographic targets. Religious objections are based on the view that premarital sex should not happen, while married couples should have as many children as possible. As such, the Catholic Church encourages premarital abstinence from sex. This argument was written out in Humanae Vitae, a papal encyclical released in 1968. The Catholic Church bases its argument against birth control pills on the basis that birth control pills undermine the natural law of God. The Catholic Church also argues against birth control on the basis of family size, with Cardinal Mercier of Belgium arguing, "...the duties of conscience are above worldly considerations, and besides, it is the large families who are the best" (Reiterman, 216). Another argument states that women should use natural methods of contraception in place of artificial ones, such as having sexual intercourse when one is infertile.
Support for contraception is based on views such as reproductive rights, women's rights, and the necessity to prevent child abandonment and child poverty. The World Health Organization states that "By preventing unintended pregnancy, family planning /contraception prevents deaths of mothers and children".
Sexually transmitted infection
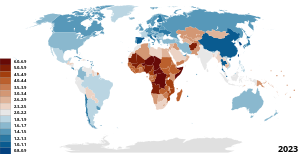
| No data <0.10 0.10–0.5 0.5–1 | 1–5 5–15 15–50 |
A sexually transmitted infection (STI) --previously known as a sexually transmitted disease (STD) or venereal disease (VD)-- is an infection that has a significant likelihood of transmission between humans by means of sexual activity. The CDC analyses the eight most common STIs: chlamydia, gonorrhea, hepatitis B virus (HBV), herpes simplex virus type 2 (HSV-2), human immunodeficiency virus (HIV), human papillomavirus (HPV), syphilis, and trichomoniasis.
There are more than 600 million cases of STIs worldwide and more than 20 million new cases within the United States. Numbers of such high magnitude weigh a heavy burden on the local and global economy. A study conducted at Oxford University in 2015 concluded that despite giving participants early antiviral medications (ART), they still cost an estimated $256 billion over 2 decades. HIV testing done at modest rates could reduce HIV infections by 21%, HIV retention by 54% and HIV mortality rates by 64%, with a cost-effectiveness ration of $45,300 per quality-adjusted life year. However, the study concluded that the United States has led to an excess in infections, treatment costs, and deaths, even when interventions do not improve over all survival rates.
There is a profound reduction on STI rates once those who are sexually active are educated about transmissions, condom promotion, interventions targeted at key and vulnerable populations through a comprehensive sex education courses or programs. South Africa's policy addresses the needs of women at risk for HIV and who are HIV positive as well as their partners and children. The policy also promotes screening activities related to sexual health such as HIV counseling and testing as well as testing for other STIs, tuberculosis, cervical cancer, and breast cancer.
Young African American women are at a higher risk for STIs, including HIV. A recent study published outside of Atlanta, Georgia collected data (demographic, psychological, and behavioral measures) with a vaginal swab to confirm the presence of STIs. They found a profound difference that those women who had graduated from college were far less likely to have STIs, potentially be benefiting from a reduction in vulnerability to acquiring STIs/HIV as they gain in education status and potentially move up in demographic areas and/or status.
Abortion
Globally, an estimated 25 million unsafe abortions occur each year. The vast majority of such unsafe abortions occur in developing countries in Africa, Asia and Latin America.
The abortion debate is the ongoing controversy surrounding the moral, legal, and religious status of induced abortion. The sides involved in the debate are the self-described "pro-choice" and "pro-life" movements. "Pro-choice" emphasizes the right of women to decide whether to terminate a pregnancy. "Pro-life" emphasizes the right of the embryo or fetus to gestate to term and be born. Both terms are considered loaded in mainstream media, where terms such as "abortion rights" or "anti-abortion" are generally preferred. Each movement has, with varying results, sought to influence public opinion and to attain legal support for its position, with small numbers of anti-abortion advocates using violence, such as murder and arson.
Articles from the World Health Organization call legal abortion a fundamental right of women regardless of where they live, and argue that unsafe abortion is a silent pandemic. In 2005, it was estimated that 19-20 million abortions had complications, some complications are permanent, while another estimated 68,000 women died from unsafe abortions. Having access to safe abortion can have positive impacts on women's health and life, and vice versa. "Legislation of abortion on request is necessary but an insufficient step towards improving women's health. In some countries where it abortion is legal, and has been for decades, there has been no improvement in access to adequate services making abortion unsafe due to lack of healthcare services. It is hard to get an abortion due to legal and policy barriers, social and cultural barriers (gender discrimination, poverty, religious restrictions, lack of support), health system barriers (lack of facilities or trained personnel). However, safe abortions with trained personnel, good social support, and access to facilities, can improve maternal health and increase reproductive health later in life.
The Maputo Protocol, which was adopted by the African Union in the form of a protocol to the African Charter on Human and Peoples' Rights, states at Article 14 (Health and Reproductive Rights) that: "(2). States Parties shall take all appropriate measures to: [...] c) protect the reproductive rights of women by authorising medical abortion in cases of sexual assault, rape, incest, and where the continued pregnancy endangers the mental and physical health of the mother or the life of the mother or the foetus." The Maputo Protocol is the first international treaty to recognize abortion, under certain conditions, as a woman's human right.
The General comment No. 36 (2018) on article 6 of the International Covenant on Civil and Political Rights, on the right to life, adopted by the Human Rights Committee in 2018, defines, for the first time ever, a human right to abortion - in certain circumstances (however these UN general comments are considered soft law, and, as such, not legally binding).
"Although States parties may adopt measures designed to regulate voluntary terminations of pregnancy, such measures must not result in violation of the right to life of a pregnant woman or girl, or her other rights under the Covenant. Thus, restrictions on the ability of women or girls to seek abortion must not, inter alia, jeopardize their lives, subject them to physical or mental pain or suffering which violates article 7, discriminate against them or arbitrarily interfere with their privacy. States parties must provide safe, legal and effective access to abortion where the life and health of the pregnant woman or girl is at risk, and where carrying a pregnancy to term would cause the pregnant woman or girl substantial pain or suffering, most notably where the pregnancy is the result of rape or incest or is not viable. In addition, States parties may not regulate pregnancy or abortion in all other cases in a manner that runs contrary to their duty to ensure that women and girls do not have to undertake unsafe abortions, and they should revise their abortion laws accordingly. For example, they should not take measures such as criminalizing pregnancies by unmarried women or apply criminal sanctions against women and girls undergoing abortion or against medical service providers assisting them in doing so, since taking such measures compel women and girls to resort to unsafe abortion. States parties should not introduce new barriers and should remove existing barriers that deny effective access by women and girls to safe and legal abortion, including barriers caused as a result of the exercise of conscientious objection by individual medical providers."
When negotiating the Cairo Programme of Action at the 1994 International Conference on Population and Development (ICPD), the issue was so contentious that delegates eventually decided to omit any recommendation to legalize abortion, instead advising governments to provide proper post-abortion care and to invest in programs that will decrease the number of unwanted pregnancies.
The Committee on the Elimination of Discrimination against Women considers the criminalization of abortion a "violations of women’s sexual and reproductive health and rights" and a form of "gender based violence"; paragraph 18 of its General recommendation No. 35 on gender based violence against women, updating general recommendation No. 19 states that: "Violations of women’s sexual and reproductive health and rights, such as forced sterilizations, forced abortion, forced pregnancy, criminalisation of abortion, denial or delay of safe abortion and post abortion care, forced continuation of pregnancy, abuse and mistreatment of women and girls seeking sexual and reproductive health information, goods and services, are forms of gender based violence that, depending on the circumstances, may amount to torture or cruel, inhuman or degrading treatment." The same General Recommendation also urges countries at paragraph 31 to [...] In particular, repeal: a) Provisions that allow, tolerate or condone forms of gender based violence against women, including [...] legislation that criminalises abortion".
In 2008, the Parliamentary Assembly of the Council of Europe, a group comprising members from 47 European countries, has adopted a resolution calling for the decriminalization of abortion within reasonable gestational limits and guaranteed access to safe abortion procedures. The nonbinding resolution was passed on April 16 by a vote of 102 to 69.
Accesses to abortion is not only a question of legality, but also an issue of overcoming de facto barriers, such as conscientious objections from medical stuff, high prices, lack of knowledge about the law, lack of access to medical care (especially in rural areas). The de facto inability of women to access abortion even in countries where it is legal is highly controversial because it results in a situation where women have rights only on paper not in practice; the UN in its 2017 resolution on Intensification of efforts to prevent and eliminate all forms of violence against women and girls: domestic violence urged states to guarantee access to "safe abortion where such services are permitted by national law".
There are two primary arguments for maintaining legalized abortion today in the U.S. The first is recognizing the full citizenship of women. The Roe v. Wade court case on abortion compared the citizenship of women and fetuses Because the Constitution defines born people as citizens, Justice Harry Blackmun ruled that fetuses were not citizens. The citizenship of women is emphasized because fetuses are not individual entities that can exist without the woman. Another reason why the full citizenship of women is defined by advocates for abortion is that it recognizes the right of women to manage their own bodies. Fertility affects women's bodies. The argument for abortion prevents others from making decisions that alter a woman's body. Pro-choice advocates also attempt to confirm that state-mandated education or other outside biases do not attempt to influence these decisions. Feminists argue that women throughout history have had to justify their citizenship politically and socially. The right to manage one's own body is a matter of health, safety, and respect. The citizenship of women and the right to manage their own bodies is a societal confirmation that feminists highlight as a pro-choice justification.
The second primary argument to uphold legalized abortion and creating better access to it is the necessity of abortion and the health and safety of pregnant women. There are two events that largely changed the course of public opinion about abortion in the U.S. The first is Sherry Finkbine, who was denied access to an abortion by the board of obstetrician-gynecologists at her local hospital. Although she was privileged enough to afford the trip, Finkbine was forced to travel to Sweden for an abortion to avoid caring for a damaged fetus in addition to four children. The other event that changed public opinion was the outbreak of rubella in the 1950s and 60s. Because rubella disrupted the growth of fetuses and caused deformities during pregnancy, the California Therapeutic Abortion Act was signed in 1967, permitting doctors to legally abort pregnancies that pose a risk to a pregnant woman's physical or mental health. These two events are commonly used to show how the health and safety of pregnant women are contingent upon abortions as well as the ability to give birth to and adequately take care of a child. Another argument in favor of legalized abortion to service necessity are the reasons why an abortion might be necessary. Nearly half of all pregnancies in the United States are unintended, and over half of all unintended pregnancies in the United States are met with abortion. Unintended pregnancy can lead to serious harm to women and children for reasons such as not being able to afford to raise a baby, inaccessibility to time off of work, difficulties facing single motherhood, difficult socio-economic conditions for women. Unintended pregnancies also have a greater potential for putting women of color at risk due to systematically produced environmental hazards from proximity to pollution, access to livable income, and affordable healthy food. These factors as threats to the health and safety of pregnant women run parallel to data that shows the number of abortions in the United States did not decline while laws restricting legal access to abortion were implemented.
At a global level, the region with the strictest abortion laws is considered to be Latin America (see Reproductive rights in Latin America), a region strongly influenced by the Catholic Church in Latin America.
Female genital mutilation
Female genital mutilation (FGM), also known as female genital circumcision or cutting, is the traditional, non-medical practice of altering or injuring the female reproductive organs, often by removing all or parts of the external genitalia. It is mostly practiced in 30 countries in Africa, the Middle East, and Asia, and affects over 200 million women and girls worldwide. More severe forms of FGM are highly concentrated in Djibouti, Eritrea, Ethiopia, Somalia, and Sudan.
The WHO categorizes FGM into four types:
- Type I (Clitoridectomy) is the removal of all or part of the clitoris. This may or may not include removing the prepuce along with the clitoral glans.
- Type II (Excision) is the removal of the clitoris along with all or part of the labia minora. This may or may not include removing all or part of the labia majora.
- Type III (Infibulation) is the act of removing the inner or outer labia and sealing the wound, leaving only a narrow opening.
- Type IV refers to "all other harmful procedures to the female genitalia for non-medical purposes (piercing, scraping, cauterizing of the genital area)."
FGM often takes the form of a traditional celebration conducted by an elder or community leader. The age that women undergo the procedure varies depending on the culture, although it is most commonly performed on prepubescent girls. Certain cultures value FGM as coming of age ritual for girls, and use it to preserve a woman's virginity and faithfulness to the husband after marriage. It is also closely connected with some traditional ideals of female beauty and hygiene. FGM may or may not have religious connotations depending on the circumstances.
There are no health benefits of FGM, as it interferes with the natural functions of a woman's and girls' bodies, such as causing severe pain, shock, hemorrhage, tetanus or sepsis (bacterial infection), urine retention, open sores in the genital region and injury to nearby genital tissue, recurrent bladder and urinary tract infections, cysts, increased risk of infertility, childbirth complications and newborn deaths. Sexual problems are 1.5 more likely to occur in women who have undergone FGM, they may experience painful intercourse, have less sexual satisfaction, and be two times more likely to report lack of sexual desire. In addition, the maternal and fetal death rate is significantly higher due to childbirth complications.
FGM can have severe negative psychological effects on women, both during and after the procedure. These can include long-term symptoms of depression, anxiety, post-traumatic stress disorder, and low self-esteem. Some women report that the procedure was carried out without their consent and knowledge, and describe feelings of fear and helplessness while it was taking place. A 2018 study found that larger quantities of the hormone cortisol were secreted in women who had undergone FGM, especially those who had experienced more severe forms of the procedure and at an early age. This marks the body's chemical response to trauma and stress, and can indicate a greater risk for developing symptoms of PTSD and other trauma disorders, although there are limited studies showing a direct correlation.
Legislation has been introduced in certain countries to prevent FGM. A 2016 survey of 30 countries showed 24 had policies to manage and prevent FGM, although the process to provide funding, education, and resources were often inconsistent and lacking. Some countries have seen a slight decline in FGM rates, while others show little to no change.
The Istanbul Convention prohibits FGM (Article 38).
Child and forced marriage
The practice of forcing young girls into early marriage, common in many parts of the world, is threatening their reproductive health. According to the World Health Organization:
The sexual and reproductive health of the female in a child marriage is likely to be jeopardized, as these young girls are often forced into sexual intercourse with an older male spouse with more sexual experience. The female spouse often lacks the status and the knowledge to negotiate for safe sex and contraceptive practices, increasing the risk of acquiring HIV or other sexually transmitted infections, as well as the probability of pregnancy at an early age.
Niger has the highest prevalence of child marriage under 18 in the world, while Bangladesh has the highest rate of marriage of girls under age 15. Practices such as bride price and dowry can contribute to child and forced marriages.
International Conference on Population and Development, 1994
The International Conference on Population and Development (ICPD) was held in Cairo, Egypt, from 5 to 13 September 1994. Delegations from 179 States took part in negotiations to finalize a Programme of Action on population and development for the next 20 years. Some 20,000 delegates from various governments, UN agencies, NGOs, and the media gathered for a discussion of a variety of population issues, including immigration, infant mortality, birth control, family planning, and the education of women.
In the ICPD Program of Action, 'reproductive health' is defined as:
a state of complete physical, mental and social well-being and...not merely the absence of disease or infirmity, in all matters relating to the reproductive system and its functions and processes. Reproductive health therefore implies that people are able to have a satisfying and safe sex life and that they have the capability to reproduce and the freedom to decide if, when and how often to do so. Implicit in this last condition are the right of men and women to be informed [about] and to have access to safe, effective, affordable and acceptable methods of family planning of their choice, as well as other methods of birth control which are not against the law, and the right of access to appropriate health-care services that will enable women to go safely through pregnancy and childbirth and provide couples with the best chance of having a healthy infant.
This definition of the term is also echoed in the United Nations Fourth World Conference on Women, or the so-called Beijing Declaration of 1995. However, the ICPD Program of Action, even though it received the support of a large majority of UN Member States, does not enjoy the status of an international legal instrument; it is therefore not legally binding.
The Program of Action endorses a new strategy which emphasizes the numerous linkages between population and development and focuses on meeting the needs of individual women and men rather than on achieving demographic targets. The ICPD achieved consensus on four qualitative and quantitative goals for the international community, the final two of which have particular relevance for reproductive health:
- Reduction of maternal mortality: A reduction of maternal mortality rates and a narrowing of disparities in maternal mortality within countries and between geographical regions, socio-economic and ethnic groups.
- Access to reproductive and sexual health services including family planning: Family planning counseling, pre-natal care, safe delivery and post-natal care, prevention and appropriate treatment of infertility, prevention of abortion and the management of the consequences of abortion, treatment of reproductive tract infections, sexually transmitted diseases and other reproductive health conditions; and education, counseling, as appropriate, on human sexuality, reproductive health and responsible parenthood. Services regarding HIV/AIDS, breast cancer, infertility, delivery, hormone therapy, sex reassignment therapy, and abortion should be made available. Active discouragement of female genital mutilation (FGM).
The keys to this new approach are empowering women, providing them with more choices through expanded access to education and health services, and promoting skill development and employment. The programme advocates making family planning universally available by 2015 or sooner, as part of a broadened approach to reproductive health and rights, provides estimates of the levels of national resources and international assistance that will be required, and calls on governments to make these resources available.
Sustainable Development Goals
Half of the development goals put on by the United Nations started in 2000 to 2015 with the Millennium Development Goals (MDGs). Reproductive health was Goal 5 out of 8. To monitor the progress, the UN agreed to four indicators:
- Contraceptive prevalence rates
- Adolescent birth rate
- Antenatal care coverage
- Unmet need for family planning
Progress was slow, and according to the WHO in 2005, about 55% of women did not have sufficient antenatal care and 24% had no access to family planning services. The MDGs expired in 2015 and were replaced with a more comprehensive set of goals to cover a span of 2016–2030 with a total of 17 goals, called the Sustainable Development Goals. All 17 goals are comprehensive in nature and build off one another, but goal 3 is "To ensure health lives and promote wellbeing for all at all ages". Specific goals are to reduce global maternal mortality ratio to less than 70 per 100,000 live births, end preventable deaths of newborns and children, reduce the number by 50% of accidental deaths globally, strengthen the treatment and prevention programs of substance abuse and alcohol. In addition, one of the targets of the Sustainable Development Goal 5 is to ensure universal access to sexual and reproductive health.
By region
North America
The CDC estimated that one in five people in the US had a sexually transmitted infection (STI).[82] CDC funding for STI prevention, when accounting for inflation, has reduced by 40% in the period 2003–2020.
Africa
HIV/AIDS in Africa is a major public health problem. Sub-Saharan Africa is the worst affected world region for the prevalence of HIV, especially among young women. 90% of the children in the world living with HIV are in sub-Saharan Africa.
In most African countries, the total fertility rate is very high, often due to lack of access to contraception and family planning, and practices such as forced and child marriage. Niger, Angola, Mali, Burundi, Somalia and Uganda have very high fertility rates. According to the United Nations Department of Economic and Social Affairs, Africa has the lowest rate of contraceptive use (33%) and the highest rate of unmet need for contraceptives (22%).
The updated contraceptive guidelines in South Africa attempt to improve access by providing special service delivery and access considerations for sex workers, lesbian, gay, bisexual, transgender and intersex individuals, migrants, men, adolescents, women who are perimenopausal, have a disability, or chronic condition. They also aim to increase access to long-acting contraceptive methods, particularly the copper IUD, and the introductions of single rod progestogen implant and combined oestrogen and progestogen injectables. The copper IUD has been provided significantly less frequently than other contraceptive methods but signs of an increase in most provinces were reported. The most frequently provided method was injectable progesterone, which the article acknowledged was not ideal and emphasised condom use with this method because it can increase the risk of HIV: The product made up 49% of South Africa's contraceptive use and up to 90% in some provinces.
Tanzanian provider perspectives address the obstacles to consistent contraceptive use in their communities. It was found that the capability of dispensaries to service patients was determined by inconsistent reproductive goals, low educational attainment, misconceptions about the side effects of contraceptives, and social factors such as gender dynamics, spousal dynamics, economic conditions, religious norms, cultural norms, and constraints in supply chains. A provider referenced an example of propaganda spread about the side effects of contraception: "There are influential people, for example, elders and religious leaders. They normally convince people that condoms contain some microorganisms and contraceptive pills cause cancer". Another said that women often had pressure from their spouse or family that caused them to use birth control secretly or to discontinue use and that women frequently preferred undetectable methods for this reason. Access was also hindered as a result of a lack in properly trained medical personnel: "Shortage of the medical attendant...is a challenge, we are not able to attend to a big number of clients, also we do not have enough education which makes us unable to provide women with the methods they want". The majority of medical centers were staffed by people without medical training and few doctors and nurses, despite federal regulations, due to lack of resources. One center had only one person who was able to insert and remove implants, and without her, they were unable to service people who wanted an implant inserted or removed. Another dispensary that carried two methods of birth control shared that they sometimes run out of both materials at the same time. Constraints in supply chains sometimes cause dispensaries to run out of contraceptive materials. Providers also claimed that more male involvement and education would be helpful. Public health officials, researchers, and programs can gain a more comprehensive picture of the barriers they face, and the efficacy of current approaches to family planning, by tracking specific, standardized family planning and reproductive health indicators.
In Mozambique, despite efforts in improving access to modern contraceptive methods, the general fertility rate is still high at 5.3 and the unmet need for contraceptives is also high at 26%. Among young women, the fertility rate has dramatically increased from 167 births per 1000 aged between 15-19 in 2011 to 194 in 2015 with a large increase in rural areas from 183 to 230. Contraceptive prevalence among 15 – 19 remains low at 14% in 2015 when compared to the national prevalence among reproductive age group (15–49 years) at 25% in the same year.