| Sleep disorder | |
|---|---|
 | |
| Pediatric polysomnography | |
Disruptions in sleep can be caused by a variety of issues, including teeth grinding (bruxism) and night terrors. When a person suffers from difficulty falling asleep and/or staying asleep with no obvious cause, it is referred to as insomnia.
Sleep disorders are broadly classified into dyssomnias, parasomnias, circadian rhythm sleep disorders involving the timing of sleep, and other disorders including ones caused by medical or psychological conditions.
The most common sleep disorder is insomnia. Others are sleep apnea, narcolepsy and hypersomnia (excessive sleepiness at inappropriate times), sleeping sickness (disruption of sleep cycle due to infection), sleepwalking, and night terrors. Management of sleep disturbances that are secondary to mental, medical, or substance abuse disorders should focus on the underlying conditions.
Primary sleep disorders are common in both children and adults. However, there is a significant lack of awareness in children with sleep disorders, due to most cases being unidentified. Several common factors involved in the onset of a sleep disorder include increased medication use, age-related changes in circadian rhythms, environmental and lifestyle changes and pre diagnosed physiological problems and stress. The risk of developing sleep disorders in the elderly is especially increased for sleep disordered breathing, periodic limb movements, restless legs syndrome, REM sleep behavior disorders, insomnia and circadian rhythm disturbances.
List of conditions
There are a number of sleep disorders, the following list includes some of them:
- Bruxism, involuntarily grinding or clenching of the teeth while sleeping.
- Catathrenia, nocturnal groaning during prolonged exhalation.
- Delayed sleep phase disorder (DSPD), inability to awaken and fall asleep at socially acceptable times but no problem with sleep maintenance, a disorder of circadian rhythms. Other such disorders are advanced sleep phase disorder (ASPD), non-24-hour sleep–wake disorder (non-24) in the sighted or in the blind, and irregular sleep wake rhythm, all much less common than DSPD, as well as the situational shift work sleep disorder.
- Fatal familial insomnia, an extremely rare genetic disorder that causes a complete cessation of sleep, leading quickly to death by sleep deprivation.
- Hypopnea syndrome, abnormally shallow breathing or slow respiratory rate while sleeping.
- Idiopathic hypersomnia, a primary, neurologic cause of long-sleeping, sharing many similarities with narcolepsy.
- Insomnia disorder (primary insomnia), chronic difficulty in falling asleep and/or maintaining sleep when no other cause is found for these symptoms. Insomnia can also be comorbid with or secondary to other disorders.
- Kleine–Levin syndrome, a rare disorder characterized by persistent episodic hypersomnia and cognitive or mood changes.
- Narcolepsy, including excessive daytime sleepiness (EDS), often culminating in falling asleep spontaneously but unwillingly at inappropriate times. About 70% of those who have narcolepsy also have cataplexy, a sudden weakness in the motor muscles that can result in collapse to the floor while retaining full conscious awareness.
- Night terror, Pavor nocturnus, sleep terror disorder, an abrupt awakening from sleep with behavior consistent with terror.
- Nocturia, a frequent need to get up and urinate at night. It differs from enuresis, or bed-wetting, in which the person does not arouse from sleep, but the bladder nevertheless empties.
- Parasomnias, disruptive sleep-related events involving inappropriate actions during sleep, for example sleep walking, night-terrors and catathrenia.
- Periodic limb movement disorder (PLMD), sudden involuntary movement of arms and/or legs during sleep, for example kicking the legs. Also known as nocturnal myoclonus. See also Hypnic jerk, which is not a disorder.
- Rapid eye movement sleep behavior disorder (RBD), acting out violent or dramatic dreams while in REM sleep, sometimes injuring bed partner or self (REM sleep disorder or RSD).
- Restless legs syndrome (RLS), an irresistible urge to move legs. RLS sufferers often also have PLMD.
- Shift work sleep disorder (SWSD), a situational circadian rhythm sleep disorder. (Jet lag was previously included as a situational circadian rhythm sleep disorder, but it doesn't appear in DSM-5 (see Diagnostic and Statistical Manual of Mental Disorders)).
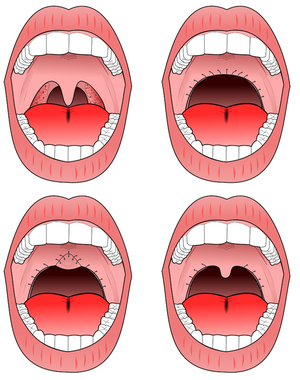
- Sleep apnea, obstructive sleep apnea, obstruction of the airway during sleep, causing lack of sufficient deep sleep, often accompanied by snoring. Other forms of sleep apnea are less common. Obstructive sleep apnea (OSA) is a medical disorder that is caused by repetitive collapse of the upper airway (back of the throat) during sleep. For the purposes of sleep studies, episodes of full upper airway collapse for at least ten seconds are called apneas
- Sleep paralysis, characterized by temporary paralysis of the body shortly before or after sleep. Sleep paralysis may be accompanied by visual, auditory or tactile hallucinations. Not a disorder unless severe. Often seen as part of narcolepsy.
- Sleepwalking or somnambulism, engaging in activities normally associated with wakefulness (such as eating or dressing), which may include walking, without the conscious knowledge of the subject.
- Somniphobia, one cause of sleep deprivation, a dread/ fear of falling asleep or going to bed. Signs of the illness include anxiety and panic attacks before and during attempts to sleep.
Types
- Dyssomnias – A broad category of sleep disorders characterized by either hypersomnia or insomnia.
The three major subcategories include intrinsic (i.e., arising from
within the body), extrinsic (secondary to environmental conditions or
various pathologic conditions), and disturbances of circadian rhythm.
- Insomnia: Insomnia may be primary or it may be comorbid with or secondary to another disorder such as a mood disorder (i.e., emotional stress, anxiety, depression) or underlying health condition (i.e., asthma, diabetes, heart disease, pregnancy or neurological conditions).
- Primary hypersomnia. Hypersomnia of central or brain origin.
- Narcolepsy: A chronic neurological disorder (or dyssomnia), which is caused by the brain's inability to control sleep and wakefulness.
- Idiopathic hypersomnia: a chronic neurological disease similar to narcolepsy in which there is an increased amount of fatigue and sleep during the day. Patients who suffer from idiopathic hypersomnia cannot obtain a healthy amount of sleep for a regular day of activities. This hinders the patients' ability to perform well, and patients have to deal with this for the rest of their lives.
- Recurrent hypersomnia – including Kleine–Levin syndrome
- Posttraumatic hypersomnia
- Menstrual-related hypersomnia
- Sleep disordered breathing (SDB), including (non exhaustive):
- Several types of Sleep apnea
- Snoring
- Upper airway resistance syndrome
- Restless leg syndrome
- Periodic limb movement disorder
- Circadian rhythm sleep disorders
- Parasomnias
– A category of sleep disorders that involve abnormal and unnatural
movements, behaviors, emotions, perceptions, and dreams in connection
with sleep.
- Bedwetting or sleep enuresis
- Bruxism (Tooth-grinding)
- Catathrenia – nocturnal groaning
- Exploding head syndrome – Waking up in the night hearing loud noises.
- Sleep terror (or Pavor nocturnus)- Characterized by a sudden arousal from deep sleep with a scream or cry, accompanied by some behavioral manifestations of intense fear.
- REM sleep behaviour disorder
- Sleepwalking (or somnambulism)
- Sleep talking (or somniloquy)
- Sleep sex (or sexsomnia)
- Medical or psychiatric conditions that may produce sleep disorders
- Sleeping sickness – a parasitic disease which can be transmitted by the Tsetse fly.
Causes
A systematic review found that traumatic childhood experiences (such as family conflict or sexual trauma) significantly increases the risk for a number of sleep disorders in adulthood, including sleep apnea, narcolepsy, and insomnia. It is currently unclear whether or not moderate alcohol consumption increases the risk of obstructive sleep apnea.
In addition, an evidence-based synopses suggests that the sleep disorder, idiopathic REM sleep behavior disorder (iRBD), may have a hereditary component to it. A total of 632 participants, half with iRBD and half without, completed self-report questionnaires. The results of the study suggest that people with iRBD are more likely to report having a first-degree relative with the same sleep disorder than people of the same age and sex that do not have the disorder. More research needs to be conducted to gain further information about the hereditary nature of sleep disorders.
A population susceptible to the development of sleep disorders is people who have experienced a traumatic brain injury (TBI). Because many researchers have focused on this issue, a systematic review was conducted to synthesize their findings. According to their results, TBI individuals are most disproportionately at risk for developing narcolepsy, obstructive sleep apnea, excessive daytime sleepiness, and insomnia.
Sleep disorders and neurodegenerative diseases
Neurodegenerative diseases have been often associated with sleep disorders, mainly when they are characterized by abnormal accumulation of alpha-synuclein, such as multiple system atrophy (MSA), Parkinson's disease (PD) and Lewy body disease (LBD). For instance, people diagnosed with PD have often presented different kinds of sleep concerns, commonly regard to insomnia (around 70% of the PD population), hypersomnia (more than 50% of the PD population), and REM sleep behavior disorder (RBD) - that may affect around 40% of the PD population and it is associated with increased motor symptoms. Furthermore, RBD has been also highlighted as a strong precursor of future development of those neurodegenerative diseases over several years in prior, which seems to be a great opportunity for improving the treatments of the disease.
Sleep disturbances have been also observed in Alzheimer's disease (AD), affecting about 45% of its population. Moreover, when it is based on caregiver reports this percentage is even higher, about 70%. As well as in PD population, insomnia and hypersomnia are frequently recognized in AD patients, which have been associated with accumulation of Beta-amyloid, circadian rhythm sleep disorders (CRSD) and melatonin alteration. Additionally, changes in sleep architecture are observed in AD too. Even though with ageing the sleep architecture seems to change naturally, in AD patients it is aggravated. SWS is potentially decreased (sometimes totally absent), spindles and the time spent in REM sleep are also reduced, while its latency is increased. The poorly sleep onset in AD has been also associated with dream-related hallucination, increased restlessness, wandering and agitation, that seem to be related with sundowning - a typical chronobiological phenomenon presented in the disease.
The neurodegenerative conditions are commonly related to brain structures impairment, which might disrupt the states of sleep and wakefulness, circadian rhythm, motor or non motor functioning. On the other hand, sleep disturbances are also frequently related to worsening patient's cognitive functioning, emotional state and quality of life. Furthermore, these abnormal behavioural symptoms negatively contribute to overwhelming their relatives and caregivers. Therefore, a deeper understanding of the relationship between sleep disorders and neurodegenerative diseases seems to be extremely important, mainly considering the limited research related to it and the increasing expectancy of life.
Sleep disturbances and Alzheimer’s Disease
More than 70% of people with dementia are affected by Alzheimer's disease (AD). Despite this high number, our understanding of the mechanisms underlying the progression of this disease remains very limited. However, recent studies have highlighted a link between sleep disturbances and Alzheimer's disease.
Sleep changes with normal aging. Indeed, with age, we find a decrease in time sleeping and also a decrease in the quantity of NREM sleep, more precisely in NREM SWS (less than 10% of the SWS is maintained). Older people also are more prone to insomnia or sleep apnea.
In Alzheimer's disease, in addition to cognitive decline and memory impairment, there is also significant sleep disturbances with a modified sleep architecture. The latter may consist in sleep fragmentation, a reduction in sleep duration, insomnia, an increase in daytime napping, a decreased quantity of some sleep stages, and a resemblance between some sleep stages (N1 and N2). More than 65% of people with Alzheimer's disease suffer from this type of sleep disturbance.
One factors that could explain this change in sleep architecture is a change in circadian rhythm, which regulates sleep. A disruption of the circadian rhythm would therefore generate sleep disturbances. Some studies show that people with AD have a delayed circadian rhythm, whereas in normal aging we will find an advanced circadian rhythm.
In addition to these psychological symptoms, at a neurological level there are two main symptoms of Alzheimer's disease. The first is an accumulation of beta-amyloid waste forming aggregate “plaques”. The second is an accumulation of tau protein.
It has been shown that the sleep-wake cycle acts on the beta-amyloid burden which is a central component found in AD. Indeed, during waking, the production of beta-amyloid protein will be more consistent than during sleep. This is explained by two phenomena. The first is that the metabolic activity will be higher during waking and thus will secrete more beta-amyloid protein. The second is that oxidative stress will also be higher and lead to increased AB production.
On the other hand, it is during sleep that beta-amyloid residues are degraded to prevent plaque formation. It is the glymphatic system that is responsible for this and this phenomenon is called glymphatic clearance. Thus, during wakefulness, the AB burden is greater because the metabolic activity and oxidative stress are higher and there is no degradation of the protein by the glymphatic clearance whereas during sleep, the burden will be smaller as there will be less metabolic activity and oxidative stress in addition to the glymphatic clearance that occurs at this time.
The glymphatic clearance occurs during the NREM sleep, and more specifically the NREM SWS sleep. As seen previously, it is a sleep stage that decreases in normal aging. So there is less glymphatic clearance and an increase in AB burden that will form the AB plaques. Therefore, in AD sleep disturbances will amplify this phenomenon.
The decrease in the quantity and quality of the NREM SWS as well as the disturbances of sleep will therefore increase the AB plaques. This will first take place at the hippocampus level, from which memory is dependent. This will result in cell death at this level and will contribute to diminished memory performances and cognitive decline found in AD disease.
Although we do not know the causal relationship, we know that the more the AD progresses, the more we find sleep disorders. In the same way, the more sleep disorders there are, the more the disease progresses, forming a vicious circle. Taken this into account, sleep disturbances are no longer a symptom of AD and relationship between sleep disturbances and AD is bidirectional.
At the same time, it has been shown that memory consolidation in long-term memory (which depends on the hippocampus) occurs during NREM sleep. This indicates that a decrease in the NREM sleep will result in less consolidation and therefore poorer memory performances in hippocampal-dependent long-term memory. This drop in performance is one of the central symptoms of AD.
Recent studies have also linked sleep disturbances, neurogenesis and AD. Indeed, it is now known that neurogenesis exists and that the subgranular zone and the subventricular zone keep on creating new neurons even in an adult brain. These new cells are then incorporated into neuronal circuits and the supragranular zone is found in the hippocampus. These new cells will contribute to learning and memory and will play a role in the hippocampal-dependent memory.
Recent studies, however, have shown that several factors can interrupt this neurogenesis. These include stress and prolonged sleep deprivation (more than one day). The sleep disturbances encountered in AD could therefore suppress neurogenesis and thus impairing hippocampal functions. This would therefore contribute to diminished memory performances and the progression of AD. And progression of AD would aggravate sleep disturbances. It is a second vicious circle.
The changes in sleep architecture found in patients with AD occur during the preclinical phase of AD. These changes could be used to detect those most at risk of developing AD. However, this is still only theoretical.
Although the exact mechanisms and the causal relationship between sleep disturbances and AD are not yet clear, these findings already provide a better understanding. In addition, they open up ideas for the implementation of treatments to curb the cognitive decline of patients suffering from this disease. In the same way, it also makes it possible to better target at risk population.
Sleep disorder symptoms in psychiatric illnesses
Schizophrenia
In individuals with psychiatric illnesses, sleep disorders may include a variety of clinical symptoms such as excessive daytime sleepiness, difficulty falling asleep, difficulty staying asleep, nightmares, sleep talking, sleep walking, and poor quality sleep, among various others. Sleep disturbances - insomnia, hypersomnia and delayed sleep-phase disorder - are quite prevalent in severe mental illnesses such as psychotic disorders. In those with schizophrenia sleep disorders contribute to cognitive deficits in learning and memory. Sleep disturbances often occur before the onset of psychosis. Sleep deprivation can also produce hallucinations, delusions and depression. A 2019 study investigated the three above-mentioned sleep disturbances in schizophrenia-spectrum (SCZ) and bipolar (BP) disorders in 617 SCZ individuals, 440 BP individuals, and 173 healthy controls (HC), sleep disturbances being identified using the Inventory for Depressive Symptoms - clinician rated scale (IDS-C). Results suggested that at least one type of sleep disturbance was reported in 78% of the SCZ population, in 69% individuals with BD, and only in 39% of the healthy controls. The SCZ group reported the most number of sleep disturbances, compared to the BD and HC group, specifically hypersomnia was more frequent among individuals with SCZ and delayed sleep phase disorder was 3 times more common in the SCZ group compared to the BD group. Finally, insomnias were the most frequently reported sleep disturbance across all three groups.
Bipolar disorder
One of the main behavioral symptoms of bipolar disorder is abnormal sleep, and studies have suggested that 23-78% of individuals with bipolar disorders consistently report symptoms of excessive time spent sleeping, or hypersomnia. The pathogenesis of bipolar disorder, including the higher risk of suicidal ideation, could possibly be linked to circadian rhythm variability, and sleep disturbances are a good predictor of mood swings. The most common sleep-related symptom of bipolar disorder is insomnia, in addition to hypersomnia, nightmares, poor sleep quality, OSA, extreme daytime sleepiness, etc. Moreover, animal models have shown that sleep debt can induce episodes of bipolar mania in laboratory mice, but these rodent models are still restricted in their potential to explain bipolar disease in humans with all its multifaceted symptoms, including those related to sleep disturbances.
Major depressive disorder (MDD)
Sleep disturbances (insomnia or hypersomnia) are not a necessary diagnostic criterion but one of the most frequent symptoms of individuals with major depressive disorder (MDD). Insomnia and hypersomnia have prevalence rates of 88% and 27%, respectively, among individuals with MDD whereas individuals with insomnia have a threefold increased risk of developing MDD. Depressed mood and sleep efficiency strongly co-vary, and while sleep regulation problems may precede depressive episodes, such depressive episodes may also precipitate sleep deprivation. Fatigue as well as sleep disturbances such as irregular and excessive sleepiness are linked to symptoms of depression.
Treatment
Treatments for sleep disorders generally can be grouped into four categories:
- Behavioral and psychotherapeutic treatment
- Rehabilitation and management
- Medication
- Other somatic treatment
None of these general approaches is sufficient for all patients with sleep disorders. Rather, the choice of a specific treatment depends on the patient's diagnosis, medical and psychiatric history, and preferences, as well as the expertise of the treating clinician. Often, behavioral/psychotherapeutic and pharmacological approaches are not incompatible and can effectively be combined to maximize therapeutic benefits. Management of sleep disturbances that are secondary to mental, medical, or substance abuse disorders should focus on the underlying conditions.
Medications and somatic treatments may provide the most rapid symptomatic relief from some sleep disturbances. Certain disorders like narcolepsy, are best treated with prescription drugs such as modafinil. Others, such as chronic and primary insomnia, may be more amenable to behavioral interventions, with more durable results.
Chronic sleep disorders in childhood, which affect some 70% of children with developmental or psychological disorders, are under-reported and under-treated. Sleep-phase disruption is also common among adolescents, whose school schedules are often incompatible with their natural circadian rhythm. Effective treatment begins with careful diagnosis using sleep diaries and perhaps sleep studies. Modifications in sleep hygiene may resolve the problem, but medical treatment is often warranted.
Special equipment may be required for treatment of several disorders such as obstructive apnea, the circadian rhythm disorders and bruxism. In these cases, when severe, an acceptance of living with the disorder, however well managed, is often necessary.
Some sleep disorders have been found to compromise glucose metabolism.
Allergy treatment
Histamine plays a role in wakefulness in the brain. An allergic reaction over produces histamine causing wakefulness and inhibiting sleep Sleep problems are common in people with allergic rhinitis. A study from the N.I.H. found that sleep is dramatically impaired by allergic symptoms and that the degree of impairment is related to the severity of those symptoms Treatment of allergies has also been shown to help sleep apnea.
Acupuncture
A review of the evidence in 2012 concluded that current research is not rigorous enough to make recommendations around the use of acupuncture for insomnia. The pooled results of two trials on acupuncture showed a moderate likelihood that there may be some improvement to sleep quality for individuals with a diagnosis insomnia. This form of treatment for sleep disorders is generally studied in adults, rather than children. Further research would be needed to study the effects of acupuncture on sleep disorders in children.
Hypnosis
Research suggests that hypnosis may be helpful in alleviating some types and manifestations of sleep disorders in some patients. "Acute and chronic insomnia often respond to relaxation and hypnotherapy approaches, along with sleep hygiene instructions." Hypnotherapy has also helped with nightmares and sleep terrors. There are several reports of successful use of hypnotherapy for parasomnias specifically for head and body rocking, bedwetting and sleepwalking.
Hypnotherapy has been studied in the treatment of sleep disorders in both adults and children.
Music therapy
Although more research should be done to increase the reliability of this method of treatment, research suggests that music therapy can improve sleep quality in acute and chronic sleep disorders. In one particular study, participants (18 years or older) who had experienced acute or chronic sleep disorders were put in a randomly controlled trial and their sleep efficiency (overall time asleep) was observed. In order to assess sleep quality, researchers used subjective measures (i.e. questionnaires) and objective measures (i.e. polysomnography). The results of the study suggest that music therapy did improve sleep quality in subjects with acute or chronic sleep disorders, however only when tested subjectively. Although these results are not fully conclusive and more research should be conducted, it still provides evidence that music therapy can be an effective treatment for sleep disorders.
In another study, specifically looking to help people with insomnia, similar results were seen. The participants that listened to music experienced better sleep quality than those who did not listen to music. Listening to slower pace music before bed can help decrease the heart rate, making it easier to transition into sleep. Studies have indicated that music helps induce a state of relaxation that shifts an individual's internal clock towards the sleep cycle. This is said to have an effect on children and adults with various cases of sleep disorders. Music is most effective before bed once the brain has been conditioned to it, helping to achieve sleep much faster.
Melatonin
Research suggests that melatonin is useful in helping people fall asleep faster (decreased sleep latency), to stay asleep longer, and to experience improved sleep quality. In order to test this, a study was conducted that compared subjects who had taken melatonin to subjects with primary sleep disorders who had taken a placebo. Researchers assessed sleep onset latency, total minutes slept, and overall sleep quality in the melatonin and placebo groups to note the differences. In the end, researchers found that melatonin decreased sleep onset latency and increased total sleep time but had an insignificant and inconclusive impact on the quality of sleep compared to a placebo group.
Sleep medicine
Due to rapidly increasing knowledge about sleep in the 20th century, including the discovery of REM sleep in the 1950s and circadian rhythm disorders in the 70s and 80s, the medical importance of sleep was recognized. The medical community began paying more attention than previously to primary sleep disorders, such as sleep apnea, as well as the role and quality of sleep in other conditions. By the 1970s in the US, clinics and laboratories devoted to the study of sleep and sleep disorders had been founded, and a need for standards arose.
Specialists in Sleep Medicine were originally certified by the American Board of Sleep Medicine, which still recognizes specialists. Those passing the Sleep Medicine Specialty Exam received the designation "diplomate of the ABSM." Sleep Medicine is now a recognized subspecialty within internal medicine, family medicine, pediatrics, otolaryngology, psychiatry and neurology in the United States. Certification in Sleep Medicine shows that the specialist:
"has demonstrated expertise in the diagnosis and management of clinical conditions that occur during sleep, that disturb sleep, or that are affected by disturbances in the wake-sleep cycle. This specialist is skilled in the analysis and interpretation of comprehensive polysomnography, and well-versed in emerging research and management of a sleep laboratory."
Competence in sleep medicine requires an understanding of a myriad of very diverse disorders, many of which present with similar symptoms such as excessive daytime sleepiness, which, in the absence of volitional sleep deprivation, "is almost inevitably caused by an identifiable and treatable sleep disorder", such as sleep apnea, narcolepsy, idiopathic hypersomnia, Kleine–Levin syndrome, menstrual-related hypersomnia, idiopathic recurrent stupor, or circadian rhythm disturbances. Another common complaint is insomnia, a set of symptoms which can have a great many different causes, physical and mental. Management in the varying situations differs greatly and cannot be undertaken without a correct diagnosis.
Sleep dentistry (bruxism, snoring and sleep apnea), while not recognized as one of the nine dental specialties, qualifies for board-certification by the American Board of Dental Sleep Medicine (ABDSM). The resulting Diplomate status is recognized by the American Academy of Sleep Medicine (AASM), and these dentists are organized in the Academy of Dental Sleep Medicine (USA). The qualified dentists collaborate with sleep physicians at accredited sleep centers and can provide oral appliance therapy and upper airway surgery to treat or manage sleep-related breathing disorders.
Occupational Therapy is an area of medicine that can also address a diagnosis of sleep disorder, as Rest and Sleep is listed in the Occupational Therapy Practice Framework (OTPF) as its own occupation of daily living. Rest and Sleep is described as restorative in order to support engagement in other Occupational Therapy occupations. In the OTPF, the occupation of Rest and Sleep is broken down into Rest, Sleep Preparation and Sleep Participation. Occupational Therapists have been shown to help improve restorative sleep through the use of assistive devices/equipment, Cognitive Behavioral Therapy for Insomnia, therapeutic activities, and/or lifestyle interventions.
In the UK, knowledge of sleep medicine and possibilities for diagnosis and treatment seem to lag. Guardian.co.uk quotes the director of the Imperial College Healthcare Sleep Centre: "One problem is that there has been relatively little training in sleep medicine in this country – certainly there is no structured training for sleep physicians." The Imperial College Healthcare site shows attention to obstructive sleep apnea syndrome (OSA) and very few other sleep disorders. Some NHS trusts have specialist clinics for respiratory and/or neurological sleep medicine.
Epidemiology
Children and young adults
According to one meta-analysis, the two most prevalent sleep disorders among children are confusional arousals and sleep walking. An estimated 17.3% of kids between 3 and 13 years old experience confusional arousals. About 17% of children sleep walk, with the disorder being more common among boys than girls. The peak ages of sleep walking are from 8 to 12 years old. A different systematic review offers a high range of prevalence rates of sleep bruxism for children. Between 15.29 and 38.6% of preschoolers grind their teeth at least one night a week. All but one of the included studies reports decreasing bruxist prevalence as age increased as well as a higher prevalence among boys than girls.
Another systematic review noted 7-16% of young adults suffer from delayed sleep phase disorder. This disorder reaches peak prevalence when people are in their 20s. Between 20 and 26% of adolescents report a sleep onset latency of greater than 30 minutes. Also, 7-36% have difficulty initiating sleep. Asian teens tend to have a higher prevalence of all of these adverse sleep outcomes than their North American and European counterparts.
Insomnia
Combining results from 17 studies on insomnia in China, a pooled prevalence of 15.0% is reported for the country. This is considerably lower than a series of Western countries (50.5% in Poland, 37.2% in France and Italy, 27.1% in USA). However, the result is consistent among other East Asian countries. Men and women residing in China experience insomnia at similar rates. A separate meta-analysis focusing on this sleeping disorder in the elderly mentions that those with more than one physical or psychiatric malady experience it at a 60% higher rate than those with one condition or less. It also notes a higher prevalence of insomnia in women over the age of 50 than their male counterparts.
A study that was resulted from a collaboration between Massachusetts General Hospital and Merck describes the development of an algorithm to identify patients will sleep disorders using electronic medical records. The algorithm that incorporated a combination of structured and unstructured variables identified more than 36,000 individuals with physician-documented insomnia.
Obstructive sleep apnea
Obstructive sleep apnea (OSA) affects around 4% of men and 2% of women in the United States. In general, this disorder is more prevalent among men. However, this difference tends to diminish with age. Women experience the highest risk for OSA during pregnancy. Also, they tend to report experiencing depression and insomnia in conjunction with obstructive sleep apnea. In a meta-analysis of the various Asian countries, India and China present the highest prevalence of the disorder. Specifically, about 13.7% of the Indian population and 7% of Hong Kong's population is estimated to have OSA. The two groups experience daytime OSA symptoms such as difficulties concentrating, mood swings, or high blood pressure, at similar rates (prevalence of 3.5% and 3.57%, respectively).
Sleep paralysis
A systematic review states 7.6% of the general population experiences sleep paralysis at least once in their lifetime. Its prevalence among men is 15.9% while 18.9% of women experience it. When considering specific populations, 28.3% of students and 31.9% of psychiatric patients have experienced this phenomenon at least once in their lifetime. Of those psychiatric patients, 34.6% have panic disorder. Sleep paralysis in students is slightly more prevalent for those of Asian descent (39.9%) than other ethnicities (Hispanic: 34.5%, African descent: 31.4%, Caucasian 30.8%).
Restless leg syndrome
According to one meta-analysis, the mean prevalence rate for North America and Western Europe is estimated to be 14.5±8.0%. Specifically in the United States, the prevalence of restless leg syndrome is estimated to be between 5 and 15.7% when using strict diagnostic criteria. RLS is over 35% more prevalent in American women than their male counterparts.
See also