| Heart failure | |
|---|---|
| Other names | Chronic heart failure (CHF), congestive cardiac failure (CCF) |
 | |
| Signs and symptoms of severe heart failure | |
| Specialty | Cardiology |
| Symptoms | Shortness of breath, feeling tired, leg swelling |
| Duration | Usually lifelong |
| Causes | Heart attack, high blood pressure, abnormal heart rhythm, excessive alcohol use, infection, heart damage |
| Risk factors | Smoking, sedentary lifestyle |
| Diagnostic method | Echocardiogram |
| Differential diagnosis | Kidney failure, thyroid disease, liver disease, anemia, obesity |
| Medication | Diuretics, cardiac medications |
| Frequency | 40 million (2015), 1–2% of adults (developed countries) |
| Deaths | 35% risk of death in first year |
Heart failure (HF), also known as congestive heart failure (CHF) and congestive cardiac failure (CCF), is when the heart is unable to pump sufficiently to maintain blood flow to meet the body's needs. Signs and symptoms of heart failure commonly include shortness of breath, excessive tiredness, and leg swelling. The shortness of breath is usually worse with exercise or while lying down, and may wake the person at night. A limited ability to exercise is also a common feature. Chest pain, including angina, does not typically occur due to heart failure.
Common causes of heart failure include coronary artery disease, including a previous myocardial infarction (heart attack), high blood pressure, atrial fibrillation, valvular heart disease, excess alcohol use, infection, and cardiomyopathy of an unknown cause. These cause heart failure by changing either the structure or the function of the heart. The two types of left ventricular heart failure – heart failure with reduced ejection fraction (HFrEF), and heart failure with preserved ejection fraction (HFpEF) – are based on whether the ability of the left ventricle to contract, or to relax, is affected. The severity of the heart failure is graded by the severity of symptoms with exercise. Heart failure is not the same as heart attack (in which part of the heart muscle dies) or cardiac arrest (in which blood flow stops altogether). Other diseases that may have symptoms similar to heart failure include obesity, kidney failure, liver problems, anemia, and thyroid disease. Diagnosis is based on symptoms, physical findings, and echocardiography. Blood tests, electrocardiography, and chest radiography may be useful to determine the underlying cause.
Treatment depends on the severity and cause of the disease. In people with chronic stable mild heart failure, treatment commonly consists of lifestyle modifications such as stopping smoking, physical exercise, and dietary changes, as well as medications. In those with heart failure due to left ventricular dysfunction, angiotensin converting enzyme inhibitors, angiotensin receptor blockers, or valsartan/sacubitril along with beta blockers are recommended. For those with severe disease, aldosterone antagonists, or hydralazine with a nitrate may be used. Diuretics are useful for preventing fluid retention and the resulting shortness of breath. Sometimes, depending on the cause, an implanted device such as a pacemaker or an implantable cardiac defibrillator (ICD) may be recommended. In some moderate or severe cases, cardiac resynchronization therapy (CRT) or cardiac contractility modulation may be of benefit. A ventricular assist device (for the left, right, or both ventricles), or occasionally a heart transplant may be recommended in those with severe disease that persists despite all other measures.
Heart failure is a common, costly, and potentially fatal condition. In 2015, it affected about 40 million people globally. Overall around 2% of adults have heart failure and in those over the age of 65, this increases to 6–10%. Rates are predicted to increase. The risk of death is about 35% the first year after diagnosis, while by the second year the risk of death is less than 10% for those who remain alive. This degree of risk of death is similar to some cancers. In the United Kingdom, the disease is the reason for 5% of emergency hospital admissions. Heart failure has been known since ancient times, with the Ebers papyrus commenting on it around 1550 BCE.
Signs and symptoms
A man with congestive heart failure and marked jugular venous distension. External jugular vein marked by an arrow.
Heart failure is a pathophysiological state in which cardiac output is insufficient to meet the needs of the body and lungs. The term "congestive heart failure" is often used, as one of the common symptoms is congestion, or build-up of fluid in a person's tissues and veins in the lungs or other parts of the body.[4] Specifically, congestion takes the form of water retention and swelling (edema), both as peripheral edema (causing swollen limbs and feet) and as pulmonary edema (causing breathing difficulty), as well as ascites (swollen abdomen).
Heart failure symptoms are traditionally and somewhat arbitrarily
divided into "left" and "right" sided, recognizing that the left and
right ventricles of the heart supply different portions of the
circulation, however people commonly have both sets of signs and
symptoms.
Left-sided failure
The left side of the heart receives oxygen-rich blood from the lungs and pumps it forward to the systemic circulation (the rest of the body except for the pulmonary circulation).
Failure of the left side of the heart causes blood to back up (be
congested) into the lungs, causing respiratory symptoms as well as
fatigue due to insufficient supply of oxygenated blood. Common
respiratory signs are increased rate of breathing and increased work of breathing (non-specific signs of respiratory distress). Rales or crackles, heard initially in the lung bases, and when severe, throughout the lung fields suggest the development of pulmonary edema (fluid in the alveoli). Cyanosis which suggests severe low blood oxygen, is a late sign of extremely severe pulmonary edema.
Additional signs indicating left ventricular failure include a laterally displaced apex beat (which occurs if the heart is enlarged) and a gallop rhythm (additional heart sounds) may be heard as a marker of increased blood flow or increased intra-cardiac pressure. Heart murmurs may indicate the presence of valvular heart disease, either as a cause (e.g. aortic stenosis) or as a result (e.g. mitral regurgitation) of the heart failure.
Backward failure of the left ventricle causes congestion
of the lungs' blood vessels, and so the symptoms are predominantly
respiratory in nature. Backward failure can be subdivided into the
failure of the left atrium, the left ventricle or both within the left
circuit. The person will have dyspnea (shortness of breath) on exertion and in severe cases, dyspnea at rest. Increasing breathlessness on lying flat, called orthopnea,
occurs. It is often measured in the number of pillows required to lie
comfortably, and in orthopnea, the person may resort to sleeping while
sitting up. Another symptom of heart failure is paroxysmal nocturnal dyspnea: a sudden nighttime attack of severe breathlessness, usually several hours after going to sleep. Easy fatigability and exercise intolerance are also common complaints related to respiratory compromise.
"Cardiac asthma" or wheezing may occur.
Compromise of left ventricular forward function may result in symptoms of poor systemic circulation such as dizziness, confusion and cool extremities at rest.
Right-sided failure
Severe peripheral (pitting) edema
Right-sided heart failure is often caused by pulmonary heart disease (cor pulmonale), which is typically caused by difficulties of the pulmonary circulation, such as pulmonary hypertension or pulmonic stenosis.
Physical examination may reveal pitting peripheral edema, ascites, liver enlargement, and spleen enlargement. Jugular venous pressure is frequently assessed as a marker of fluid status, which can be accentuated by eliciting hepatojugular reflux. If the right ventricular pressure is increased, a parasternal heave may be present, signifying the compensatory increase in contraction strength.
Backward failure of the right ventricle leads to
congestion of systemic capillaries. This generates excess fluid
accumulation in the body. This causes swelling under the skin (termed peripheral edema or anasarca) and usually affects the dependent parts of the body first (causing foot and ankle swelling in people who are standing up, and sacral edema in people who are predominantly lying down). Nocturia
(frequent nighttime urination) may occur when fluid from the legs is
returned to the bloodstream while lying down at night. In progressively
severe cases, ascites
(fluid accumulation in the abdominal cavity causing swelling) and liver
enlargement may develop. Significant liver congestion may result in
impaired liver function (congestive hepatopathy), and jaundice and even coagulopathy (problems of decreased or increased blood clotting) may occur.
Biventricular failure
Dullness of the lung fields to finger percussion and reduced breath sounds at the bases of the lung may suggest the development of a pleural effusion (fluid collection between the lung and the chest wall).
Though it can occur in isolated left- or right-sided heart failure, it
is more common in biventricular failure because pleural veins drain into
both the systemic and pulmonary venous systems. When unilateral,
effusions are often right-sided.
If a person with a failure of one ventricle lives long enough, it
will tend to progress to failure of both ventricles. For example, left
ventricular failure allows pulmonary edema and pulmonary hypertension to
occur, which increase stress on the right ventricle. Right ventricular
failure is not as deleterious to the other side, but neither is it
harmless.
Causes
Viral infections of the heart can lead to inflammation of the muscular layer of the heart and subsequently contribute to the development of heart failure. Heart damage can predispose a person to develop heart failure later in life and has many causes including systemic viral infections (e.g., HIV), chemotherapeutic agents such as daunorubicin, cyclophosphamide, trastuzumab and abuse of drugs such as alcohol, cocaine, and methamphetamine. An uncommon cause is exposure to certain toxins such as lead and cobalt. Additionally, infiltrative disorders such as amyloidosis and connective tissue diseases such as systemic lupus erythematosus have similar consequences. Obstructive sleep apnea
(a condition of sleep wherein disordered breathing overlaps with
obesity, hypertension, and/or diabetes) is regarded as an independent
cause of heart failure.
High output heart failure
Heart failure may also occur in situations of "high output" (termed "high-output heart failure"), where the amount of blood pumped is more than typical and the heart is unable to keep up. This can occur in overload situations (blood or serum infusions), kidney diseases, chronic severe anemia, beriberi (vitamin B1/thiamine deficiency), hyperthyroidism, cirrhosis, Paget's disease, multiple myeloma, arteriovenous fistulae, or arteriovenous malformations.
Acute decompensation
Kerley B lines in acute cardiac decompensation. The short, horizontal lines can be found everywhere in the right lung.
Chronic stable heart failure may easily decompensate. This most commonly results from an concurrent illness (such as myocardial infarction (a heart attack) or pneumonia), abnormal heart rhythms, uncontrolled hypertension, or a person's failure to maintain a fluid restriction, diet, or medication. Other factors that may worsen CHF include: anemia, hyperthyroidism, excessive fluid or salt intake, and medication such as NSAIDs and thiazolidinediones. NSAIDs increase the risk twofold.
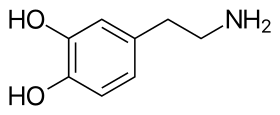
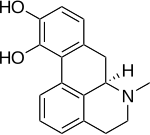
Medications
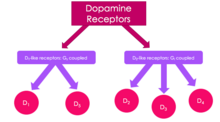
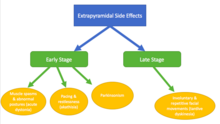
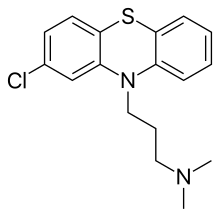
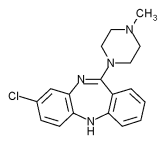
A number of medications may cause or worsen the disease. This includes NSAIDS, COX-2 inhibitors, a number of anesthetic agents such as ketamine, thiazolidinediones, some cancer medications, several antiarrhythmic medications, pregabalin, alpha-2 adrenergic receptor agonists, minoxidil, itraconazole, cilostazol, anagrelide, stimulants (e.g., methylphenidate), tricyclic antidepressants, lithium, antipsychotics, dopamine agonists, TNF inhibitors, calcium channel blockers, salbutamol, and tamsulosin.
By inhibiting the formation of prostaglandins, NSAIDs may exacerbate heart failure through several mechanisms including promotion of fluid retention, increasing blood pressure, and decreasing a person's response to diuretic medications. Similarly, the ACC/AHA recommends against the use of COX-2 inhibitor medications in people with heart failure.
Thiazolidinediones have been strongly linked to new cases of heart
failure and worsening of pre-existing congestive heart failure due to
their association with weight gain and fluid retention. Certain calcium channel blockers such as diltiazem and verapamil are known to decrease the force with which the heart ejects blood and are thus not recommended in people with heart failure with a reduced ejection fraction.
Supplements
Certain alternative medicines carry a risk of exacerbating existing heart failure, and are not recommended. This includes aconite, ginseng, gossypol, gynura, licorice, Lily of the valley, tetrandrine, and yohimbine. Aconite can cause abnormally slow heart rates and abnormal heart rhythms such as ventricular tachycardia. Ginseng can cause abnormally low or high blood pressure, and may interfere with the effects of diuretic medications. Gossypol can increase the effects of diuretics, leading to toxicity. Gynura can cause low blood pressure. Licorice can worsen heart failure by increasing blood pressure and promoting fluid retention. Lily of the valley can cause abnormally slow heart rates with mechanisms similar to those of digoxin. Tetrandrine can lead to low blood pressure through inhibition of L-type calcium channels. Yohimbine can exacerbate heart failure by increasing blood pressure through alpha-2 adrenergic receptor antagonism.
Pathophysiology
Model of a normal heart, with contracted muscle (left); and a weakened heart, with over-stretched muscle (right).
Heart failure is caused by any condition which reduces the efficiency
of the heart muscle, through damage or overloading. Over time these
increases in workload, which are mediated by long-term activation of
neurohormonal systems such as the renin–angiotensin system, leads to fibrosis, dilation, and structural changes in the shape of the left ventricle from elliptical to spherical.
The heart of a person with heart failure may have a reduced force of contraction due to overloading of the ventricle. In a normal heart, increased filling of the ventricle results in increased contraction force by the Frank–Starling law of the heart, and thus a rise in cardiac output.
In heart failure, this mechanism fails, as the ventricle is loaded with
blood to the point where heart muscle contraction becomes less
efficient. This is due to reduced ability to cross-link actin and myosin filaments in over-stretched heart muscle.
Diagnosis
No system of diagnostic criteria has been agreed on as the gold standard for heart failure. The National Institute for Health and Care Excellence recommends measuring brain natriuretic peptide (BNP) followed by an ultrasound of the heart if positive. This is recommended in those with shortness of breath. In those with worsening heart failure, both a BNP and a troponin are recommended to help determine likely outcomes.
Classification
One
historical method of categorizing heart failure is by the side of the
heart involved (left heart failure versus right heart failure). Right
heart failure was thought to compromise blood flow to the lungs compared
to left heart failure compromising blood flow to the aorta
and consequently to the brain and the remainder of the body's systemic
circulation. However, mixed presentations are common and left heart
failure is a common cause of right heart failure.
More accurate classification of heart failure type is made by measuring ejection fraction, or the proportion of blood pumped out of the heart during a single contraction. Ejection fraction is given as a percentage with the normal range being between 50 and 75%. The two types are:
1) Heart failure due to reduced ejection fraction (HFrEF).
Synonyms no longer recommended are "heart failure due to left
ventricular systolic dysfunction" and "systolic heart failure". HFrEF is
associated with an ejection fraction of less than 40%.
2) Heart failure with preserved ejection fraction (HFpEF). Synonyms no longer recommended include "diastolic heart failure" and "heart failure with normal ejection fraction."[4][18]
HFpEF occurs when the left ventricle contracts normally during systole,
but the ventricle is stiff and does not relax normally during diastole,
which impairs filling.
Heart failure may also be classified as acute or chronic. Chronic
heart failure is a long-term condition, usually kept stable by the
treatment of symptoms. Acute decompensated heart failure is a worsening of chronic heart failure symptoms which can result in acute respiratory distress. High-output heart failure
can occur when there is increased cardiac demand that results in
increased left ventricular diastolic pressure which can develop into
pulmonary congestion (pulmonary edema).
There are several terms which are closely related to heart
failure and may be the cause of heart failure, but should not be
confused with it. Cardiac arrest and asystole refer to situations in which there is no cardiac output at all. Without urgent treatment, these result in sudden death. Myocardial infarction ("Heart attack") refers to heart muscle damage due to insufficient blood supply, usually as a result of a blocked coronary artery. Cardiomyopathy
refers specifically to problems within the heart muscle, and these
problems can result in heart failure. Ischemic cardiomyopathy implies
that the cause of muscle damage is coronary artery disease. Dilated cardiomyopathy implies that the muscle damage has resulted in enlargement of the heart. Hypertrophic cardiomyopathy involves enlargement and thickening of the heart muscle.
Ultrasound
Echocardiography is commonly used to support a clinical diagnosis of heart failure. This modality uses ultrasound to determine the stroke volume (SV, the amount of blood in the heart that exits the ventricles with each beat), the end-diastolic volume (EDV, the total amount of blood at the end of diastole), and the SV in proportion to the EDV, a value known as the ejection fraction (EF). In pediatrics, the shortening fraction
is the preferred measure of systolic function. Normally, the EF should
be between 50% and 70%; in systolic heart failure, it drops below 40%.
Echocardiography can also identify valvular heart disease and assess the
state of the pericardium
(the connective tissue sac surrounding the heart). Echocardiography may
also aid in deciding what treatments will help the person, such as
medication, insertion of an implantable cardioverter-defibrillator or cardiac resynchronization therapy.
Echocardiography can also help determine if acute myocardial ischemia
is the precipitating cause, and may manifest as regional wall motion
abnormalities on echo.
- Ultrasound showing severe systolic heart failure
- Ultrasound showing severe systolic heart failure
- Ultrasound of the lungs showing edema due to severe systolic heart failure
- Ultrasound showing severe systolic heart failure
Chest X-ray
Chest radiograph of a lung with distinct Kerley B lines, as well as an enlarged heart (as shown by an increased cardiothoracic ratio, cephalization of pulmonary veins, and minor pleural effusion as seen for example in the right horizontal fissure. Yet, there is no obvious lung edema. Overall, this indicates intermediate severity (stage II) heart failure.
Chest X-rays are frequently used to aid in the diagnosis of CHF. In a person who is compensated, this may show cardiomegaly (visible enlargement of the heart), quantified as the cardiothoracic ratio
(proportion of the heart size to the chest). In left ventricular
failure, there may be evidence of vascular redistribution ("upper lobe
blood diversion" or "cephalization"), Kerley lines, cuffing of the areas around the bronchi, and interstitial edema. Ultrasound of the lung may also be able to detect Kerley lines.
Electrophysiology
An electrocardiogram (ECG/EKG) may be used to identify arrhythmias, ischemic heart disease, right and left ventricular hypertrophy, and presence of conduction delay or abnormalities (e.g. left bundle branch block).
Although these findings are not specific to the diagnosis of heart
failure a normal ECG virtually excludes left ventricular systolic
dysfunction.
Blood tests
Blood tests routinely performed include electrolytes (sodium, potassium), measures of kidney function, liver function tests, thyroid function tests, a complete blood count, and often C-reactive protein if infection is suspected. An elevated B-type natriuretic peptide
(BNP) is a specific test indicative of heart failure. Additionally, BNP
can be used to differentiate between causes of dyspnea due to heart
failure from other causes of dyspnea. If myocardial infarction is
suspected, various cardiac markers may be used.
BNP is a better indicator than N-terminal pro-BNP (NTproBNP) for
the diagnosis of symptomatic heart failure and left ventricular systolic
dysfunction. In symptomatic people, BNP had a sensitivity of 85% and specificity of 84% in detecting heart failure; performance declined with increasing age.
Hyponatremia (low serum sodium concentration) is common in heart failure. Vasopressin
levels are usually increased, along with renin, angiotensin II, and
catecholamines in order to compensate for reduced circulating volume due
to inadequate cardiac output. This leads to increased fluid and sodium
retention in the body; the rate of fluid retention is higher than the
rate of sodium retention in the body, this phenomenon causes
"hypervolemic hyponatremia" (low sodium concentration due to high body
fluid retention). This phenomenon is more common in older women with low
body mass. Severe hyponatremia can result in accumulation of fluid in
the brain, causing cerebral edema and intracranial hemorrhage.
Angiography
Angiography is the X-ray imaging of blood vessels which is done by injecting contrast agents into the bloodstream through a thin plastic tube (catheter) which is placed directly in the blood vessel. X-ray images are called angiograms. Heart failure may be the result of coronary artery disease, and its prognosis depends in part on the ability of the coronary arteries to supply blood to the myocardium (heart muscle). As a result, coronary catheterization may be used to identify possibilities for revascularisation through percutaneous coronary intervention or bypass surgery.
Algorithms
There are various algorithms for the diagnosis of heart failure. For example, the algorithm used by the Framingham Heart Study adds together criteria mainly from physical examination. In contrast, the more extensive algorithm by the European Society of Cardiology (ESC) weights the difference between supporting and opposing parameters from the medical history, physical examination, further medical tests as well as response to therapy.
Framingham criteria
By the Framingham criteria, diagnosis of congestive heart failure (heart failure with impaired pumping capability)
requires the simultaneous presence of at least 2 of the following major
criteria or 1 major criterion in conjunction with 2 of the following
minor criteria. Major criteria include an enlarged heart on a chest x-ray, an S3 gallop (a third heart sound), acute pulmonary edema, episodes of waking up from sleep gasping for air, crackles on lung auscultation, central venous pressure of more than 16 cm H
2O at the right atrium, jugular vein distension, positive abdominojugular test, and weight loss of more than 4.5 kg in 5 days in response to treatment (sometimes classified as a minor criterion). Minor criteria include an abnormally fast heart rate of more than 120 beats per minute, nocturnal cough, difficulty breathing with physical activity, pleural effusion, a decrease in the vital capacity by one third from maximum recorded, liver enlargement, and bilateral ankle swelling.
2O at the right atrium, jugular vein distension, positive abdominojugular test, and weight loss of more than 4.5 kg in 5 days in response to treatment (sometimes classified as a minor criterion). Minor criteria include an abnormally fast heart rate of more than 120 beats per minute, nocturnal cough, difficulty breathing with physical activity, pleural effusion, a decrease in the vital capacity by one third from maximum recorded, liver enlargement, and bilateral ankle swelling.
Minor criteria are acceptable only if they can not be attributed to another medical condition such as pulmonary hypertension, chronic lung disease, cirrhosis, ascites, or the nephrotic syndrome.
The Framingham Heart Study criteria are 100% sensitive and 78% specific
for identifying persons with definite congestive heart failure.
ESC algorithm
The ESC algorithm weights the following parameters in establishing the diagnosis of heart failure:
| Assessment | Diagnosis of heart failure | |
|---|---|---|
| Supports if present | Opposes if normal or absent | |
| Compatible symptoms | ++ | ++ |
| Compatible signs | ++ | + |
| Cardiac dysfunction on echocardiography | +++ | +++ |
| Response of symptoms or signs to therapy | +++ | ++ |
| ECG | ||
| Normal | ++ | |
| Abnormal | ++ | + |
| Dysrhythmia | +++ | + |
| Laboratory | ||
| Elevated BNP/NT-proBNP | +++ | + |
| Low/normal BNP/NT-proBNP | + | +++ |
| Low blood sodium | + | + |
| Kidney dysfunction | + | + |
| Mild elevations of troponin | + | + |
| Chest X-ray | ||
| Pulmonary congestion | +++ | + |
| Reduced exercise capacity | +++ | ++ |
| Abnormal pulmonary function tests | + | + |
| Abnormal hemodynamics at rest | +++ | ++ |
| + = some importance; ++ = intermediate importance; +++ = great importance. | ||
Staging
Heart
failure is commonly stratified by the degree of functional impairment
conferred by the severity of the heart failure (as reflected in the New York Heart Association (NYHA) Functional Classification.)
The NYHA functional classes (I-IV) begin with class I, which is defined
as a person who experiences no limitation in any activities and has no
symptoms from ordinary activities. People with NYHA class II heart
failure have slight, mild limitation with everyday activities; the
person is comfortable at rest or with mild exertion. With NYHA class III
heart failure, there is marked limitation with any activity; the person
is comfortable only at rest. A person with NYHA class IV heart failure
is symptomatic at rest and becomes quite uncomfortable with any physical
activity.
This score documents the severity of symptoms and can be used to assess
response to treatment. While its use is widespread, the NYHA score is
not very reproducible and does not reliably predict the walking distance
or exercise tolerance on formal testing.
In its 2001 guidelines, the American College of Cardiology/American Heart Association working group introduced four stages of heart failure:
- Stage A: People at high risk for developing HF in the future but no functional or structural heart disorder.
- Stage B: a structural heart disorder but no symptoms at any stage.
- Stage C: previous or current symptoms of heart failure in the context of an underlying structural heart problem, but managed with medical treatment.
- Stage D: advanced disease requiring hospital-based support, a heart transplant or palliative care.
The ACC staging system is useful since Stage A encompasses "pre-heart
failure" – a stage where intervention with treatment can presumably
prevent progression to overt symptoms. ACC Stage A does not have a
corresponding NYHA class. ACC Stage B would correspond to NYHA Class I.
ACC Stage C corresponds to NYHA Class II and III, while ACC Stage D
overlaps with NYHA Class IV.
- the degree of coexisting illness: i.e. heart failure/systemic hypertension, heart failure/pulmonary hypertension, heart failure/diabetes, heart failure/kidney failure, etc.
- whether the problem is primarily increased venous back pressure (preload), or failure to supply adequate arterial perfusion (afterload).
- whether the abnormality is due to low cardiac output with high systemic vascular resistance or high cardiac output with low vascular resistance (low-output heart failure vs. high-output heart failure).
Histopathology
Siderophages (one indicated by white arrow) and pulmonary congestion, indicating left congestive heart failure.
Histopathology can diagnose heart failure in autopsies. The presence of siderophages indicates chronic left-sided heart failure, but is not specific for it.It is also indicated by congestion of the pulmonary circulation.
Prevention
A person's risk of developing heart failure is inversely related to their level of physical activity. Those who achieved at least 500 MET-minutes/week
(the recommended minimum by U.S. guidelines) had lower heart failure
risk than individuals who did not report exercising during their free
time; the reduction in heart failure risk was even greater in those who
engaged in higher levels of physical activity than the recommended
minimum.
Heart failure can also be prevented by lowering high blood pressure and
high blood cholesterol, and by controlling diabetes. Maintaining a
healthy weight as well as decreasing sodium, alcohol, and sugar intake may help. Additionally, avoiding tobacco use has been shown to lower the risk of heart failure.
Management
Treatment focuses on improving the symptoms and preventing the
progression of the disease. Reversible causes of the heart failure also
need to be addressed (e.g. infection, alcohol ingestion, anemia, thyrotoxicosis, arrhythmia,
hypertension). Treatments include lifestyle and pharmacological
modalities, and occasionally various forms of device therapy and rarely
cardiac transplantation.
Acute decompensation
In acute decompensated heart failure (ADHF), the immediate goal is to re-establish adequate perfusion and oxygen delivery to end organs. This entails ensuring that airway, breathing, and circulation are adequate. Immediate treatments usually involve some combination of vasodilators such as nitroglycerin, diuretics such as furosemide, and possibly noninvasive positive pressure ventilation (NIPPV). Supplemental oxygen
is indicated in those with oxygen saturation levels below 90% but is
not recommended in those with normal oxygen levels on room air.
Chronic management
The
goals of treatment for people with chronic heart failure are the
prolongation of life, the prevention of acute decompensation and the
reduction of symptoms, allowing for greater activity.
Heart failure can result from a variety of conditions. In
considering therapeutic options, it is important to first exclude
reversible causes, including thyroid disease, anemia, chronic tachycardia, alcohol abuse, hypertension and dysfunction of one or more heart valves.
Treatment of the underlying cause is usually the first approach to
treating heart failure. However, in the majority of cases, either no
primary cause is found or treatment of the primary cause does not
restore normal heart function. In these cases, behavioral, medical and device
treatment strategies exist which can provide a significant improvement
in outcomes, including the relief of symptoms, exercise tolerance, and a
decrease in the likelihood of hospitalization or death. Breathlessness rehabilitation for chronic obstructive pulmonary disease
(COPD) and heart failure has been proposed with exercise training as a
core component. Rehabilitation should also include other interventions
to address shortness of breath including psychological and education
needs of people and needs of careers. Iron supplementation appears useful in those with iron deficiency anemia and heart failure.
Monitoring
Various measures are often used to assess the progress of people being treated for heart failure. These include fluid balance (calculation of fluid intake and excretion), monitoring body weight (which in the shorter term reflects fluid shifts). Remote monitoring can be effective to reduce complications for people with heart failure.
Lifestyle
Behavior modification is a primary consideration in chronic heart failure management program, with dietary guidelines regarding fluid and salt intake. Fluid restriction is important to reduce fluid retention in the body and to correct the hyponatremic status of the body. The evidence of benefit of reducing salt however is poor as of 2018.
Exercise should be encouraged and tailored to suit individual
capabilities. The inclusion of regular physical conditioning as part of a
cardiac rehabilitation program can significantly improve quality of life
and reduce the risk of hospital admission for worsening symptoms;
however, there is no evidence for a reduction in mortality rates as a
result of exercise. Furthermore, it is not clear whether this evidence
can be extended to people with heart failure with preserved ejection fraction (HFpEF) or to those whose exercise regimen takes place entirely at home.
Home visits and regular monitoring at heart failure clinics reduce the need for hospitalization and improve life expectancy.
Medication
First-line therapy for people with heart failure due to reduced systolic function should include angiotensin-converting enzyme (ACE) inhibitors (ACE-I) or angiotensin receptor blockers (ARBs) if the person develops a long term cough as a side effect of the ACE-I.
Use of medicines from this class is associated with improved survival,
fewer hospitalizations for heart failure exacerbations, and improved
quality of life in people with heart failure.
Beta-adrenergic blocking agents (beta blockers) also form part of the first line of treatment, adding to the improvement in symptoms and mortality provided by ACE-I/ARB. The mortality benefits of beta blockers in people with systolic dysfunction who also have atrial fibrillation (AF) is more limited than in those who do not have AF.
If the ejection fraction is not diminished (HFpEF), the benefits of
beta blockers are more modest; a decrease in mortality has been observed
but reduction in hospital admission for uncontrolled symptoms has not
been observed.
In people who are intolerant of ACE-I and ARBs or who have significant kidney dysfunction, the use of combined hydralazine and a long-acting nitrate, such as isosorbide dinitrate, is an effective alternate strategy. This regimen has been shown to reduce mortality in people with moderate heart failure. It is especially beneficial in African-Americans (AA). In AAs who are symptomatic, hydralazine and isosorbide dinitrate (H+I) can be added to ACE-I or ARBs.
In people with symptomatic heart failure with markedly reduced
ejection fraction (anyone with an ejection fraction of 35% or lower or
less than 40% if following a heart attack), the use of an aldosterone
antagonist, in addition to beta blockers and ACE-I (once titrated to the
target dose or maximum tolerated dose), can improve symptoms and reduce
mortality.
Second-line medications for CHF do not confer a mortality benefit. Digoxin
is one such medication. Its narrow therapeutic window, a high degree of
toxicity, and the failure of multiple trials to show a mortality
benefit have reduced its role in clinical practice. It is now used in
only a small number of people with refractory symptoms, who are in
atrial fibrillation and/or who have chronic low blood pressure.
Diuretics have been a mainstay of treatment for treatment of
fluid accumulation, and include diuretics classes such as loop
diuretics, thiazide-like diuretics, and potassium-sparing diuretics. Although widely used, evidence on their efficacy and safety is limited, with the exception of mineralocorticoid antagonists such as spironolactone. Mineralocorticoid antagonists in those under 75 years old appear to decrease the risk of death.
A recent Cochrane review found that in small studies, the use of
diuretics appeared to have improved mortality in individuals with heart
failure.
However, the extent to which these results can be extrapolated to a
general population is unclear due to the small number of participants in
the cited studies.
Anemia
is an independent factor in mortality in people with chronic heart
failure. The treatment of anemia significantly improves quality of life
for those with heart failure, often with a reduction in severity of the
NYHA classification, and also improves mortality rates. The European Society of Cardiology guideline in 2016 recommend screening for iron-deficiency anemia and treating with intravenous iron if deficiency is found.
The decision to anticoagulate people with HF, typically with left
ventricular ejection fractions <35 a="" amyloidosis="" an="" as="" atrial="" but="" cardiomyopathy="" coexisting="" conditions="" debated="" dilated="" embolic="" event="" familial="" fibrillation="" first-degree="" generally="" in="" increase="" is="" left="" noncompaction="" of="" or="" p="" people="" prior="" relative.="" risk="" such="" the="" thromboembolic="" ventricular="" which="" with="">
Vasopressin receptor antagonists can also be used to treat heart failure. Conivaptan is the first medication approved by US Food and Drug Administration for the treatment of euvolemic hyponatremia in those with heart failure. In rare cases hypertonic 3% saline together with diuretics may be used to correct hyponatremia.
Sacubitril/valsartan may be used in those who still have symptoms well on an ACEI, beta blocker, and a mineralocorticoid receptor antagonist. Ivabradine
is recommended for people with symptomatic heart failure with reduced
left ventricular ejection fraction who are receiving optimized guideline
directed therapy (as above) including the maximum tolerated dose of
beta blocker, have a normal heart rhythm, and continue to have a resting
heart rate above 70 beats per minute.
Ivabradine has been found to reduce the risk of hospitalization for
heart failure exacerbations in this subgroup of people with heart
failure.
Implanted devices
In
people with severe cardiomyopathy (left ventricular ejection fraction
below 35%), or in those with recurrent VT or malignant arrhythmias,
treatment with an automatic implantable cardioverter defibrillator
(AICD) is indicated to reduce the risk of severe life-threatening
arrhythmias. The AICD does not improve symptoms or reduce the incidence
of malignant arrhythmias but does reduce mortality from those
arrhythmias, often in conjunction with antiarrhythmic medications. In
people with left ventricular ejection (LVEF) below 35%, the incidence of
ventricular tachycardia (VT) or sudden cardiac death is high enough to warrant AICD placement. Its use is therefore recommended in AHA/ACC guidelines.
Cardiac contractility modulation (CCM) is a treatment for people with moderate to severe left ventricular systolic heart failure (NYHA class II–IV) which enhances both the strength of ventricular contraction and the heart's pumping capacity. The CCM mechanism is based on stimulation of the cardiac muscle by non-excitatory electrical signals (NES), which are delivered by a pacemaker-like device. CCM is particularly suitable for the treatment of heart failure with normal QRS complex duration (120 ms or less) and has been demonstrated to improve the symptoms, quality of life and exercise tolerance. CCM is approved for use in Europe, but not currently in North America.
About one third of people with LVEF
below 35% have markedly altered conduction to the ventricles, resulting
in dyssynchronous depolarization of the right and left ventricles. This
is especially problematic in people with left bundle branch block
(blockage of one of the two primary conducting fiber bundles that
originate at the base of the heart and carries depolarizing impulses to
the left ventricle). Using a special pacing algorithm, biventricular cardiac resynchronization therapy
(CRT) can initiate a normal sequence of ventricular depolarization. In
people with LVEF below 35% and prolonged QRS duration on ECG (LBBB or
QRS of 150 ms or more) there is an improvement in symptoms and mortality
when CRT is added to standard medical therapy. However, in the two-thirds of people without prolonged QRS duration, CRT may actually be harmful.
Surgical therapies
People with the most severe heart failure may be candidates for ventricular assist devices
(VAD). VADs have commonly been used as a bridge to heart
transplantation, but have been used more recently as a destination
treatment for advanced heart failure.
In select cases, heart transplantation
can be considered. While this may resolve the problems associated with
heart failure, the person must generally remain on an immunosuppressive
regimen to prevent rejection, which has its own significant downsides. A major limitation of this treatment option is the scarcity of hearts available for transplantation.
Palliative care
People with heart failure often have significant symptoms, such as shortness of breath and chest pain. Palliative care should be initiated early in the HF trajectory, and should not be an option of last resort.
Palliative care can not only provide symptom management, but also
assist with advanced care planning, goals of care in the case of a
significant decline, and making sure the person has a medical power of attorney and discussed his or her wishes with this individual.
A 2016 and 2017 review found that palliative care is associated with
improved outcomes, such as quality of life, symptom burden, and
satisfaction with care.
Without transplantation, heart failure may not be reversible and
heart function typically deteriorates with time. The growing number of
people with Stage IV heart failure (intractable symptoms of fatigue,
shortness of breath or chest pain at rest despite optimal medical
therapy) should be considered for palliative care or hospice, according to American College of Cardiology/American Heart Association guidelines.
Prognosis
Prognosis
in heart failure can be assessed in multiple ways including clinical
prediction rules and cardiopulmonary exercise testing. Clinical
prediction rules use a composite of clinical factors such as lab tests
and blood pressure to estimate prognosis. Among several clinical prediction rules
for prognosticating acute heart failure, the 'EFFECT rule' slightly
outperformed other rules in stratifying people and identifying those at
low risk of death during hospitalization or within 30 days. Easy methods for identifying people that are low-risk are:
- ADHERE Tree rule indicates that people with blood urea nitrogen < 43 mg/dl and systolic blood pressure at least 115 mm Hg have less than 10% chance of inpatient death or complications.
- BWH rule indicates that people with systolic blood pressure over 90 mm Hg, respiratory rate of 30 or fewer breaths per minute, serum sodium over 135 mmol/L, no new ST-T wave changes have less than 10% chance of inpatient death or complications.
A very important method for assessing prognosis in people with
advanced heart failure is cardiopulmonary exercise testing (CPX
testing). CPX testing is usually required prior to heart transplantation
as an indicator of prognosis. Cardiopulmonary exercise testing involves
measurement of exhaled oxygen and carbon dioxide during exercise. The
peak oxygen consumption (VO2 max) is used as an indicator of prognosis.
As a general rule, a VO2 max less than 12–14 cc/kg/min indicates a poor
survival and suggests that the person may be a candidate for a heart
transplant. People with a VO2 max<10 a="" advanced="" also="" and="" be="" can="" cc="" clearly="" criterion="" evaluation="" failure="" for="" guidelines="" have="" heart="" in="" international="" kg="" lung="" min="" most="" of="" other="" parameters="" poorer="" prognosis.="" prognosis="" recent="" score="" slope="" society="" suggest="" survival="" that="" the="" transplantation="" two="" use="" used="" ve=""> 35 from the CPX test.
The heart failure survival score is a score calculated using a
combination of clinical predictors and the VO2 max from the
cardiopulmonary exercise test.
Heart failure is associated with significantly reduced physical and mental health, resulting in a markedly decreased quality of life.
With the exception of heart failure caused by reversible conditions,
the condition usually worsens with time. Although some people survive
many years, progressive disease is associated with an overall annual
mortality rate of 10%.
Approximately 18 of every 1000 persons will experience an
ischemic stroke during the first year after diagnosis of HF. As the
duration of follow-up increases, the stroke rate rises to nearly 50
strokes per 1000 cases of HF by 5 years.
Epidemiology
In 2015 heart failure affected about 40 million people globally. Overall around 2% of adults have heart failure and in those over the age of 65, this increases to 6–10%. Above 75 years old rates are greater than 10%.
Rates are predicted to increase.
Increasing rates are mostly because of increasing life span, but also
because of increased risk factors (hypertension, diabetes, dyslipidemia,
and obesity) and improved survival rates from other types of
cardiovascular disease (myocardial infarction, valvular disease, and
arrhythmias). Heart failure is the leading cause of hospitalization in people older than 65.
United States
In the United States, heart failure affects 5.8 million people, and each year 550,000 new cases are diagnosed.
In 2011, heart failure was the most common reason for hospitalization
for adults aged 85 years and older, and the second most common for
adults aged 65–84 years.
It is estimated that one in five adults at age 40 will develop heart
failure during their remaining lifetime and about half of people who
develop heart failure die within 5 years of diagnosis.
Heart failure is much higher in African Americans, Hispanics, Native
Americans and recent immigrants from the eastern bloc countries like
Russia. This high prevalence in these ethnic minority populations has
been linked to high incidence of diabetes and hypertension. In many new
immigrants to the U.S., the high prevalence of heart failure has largely
been attributed to lack of preventive health care or substandard treatment.
Nearly one out of every four people (24.7%) hospitalized in the U.S.
with congestive heart failure are readmitted within 30 days.
Additionally, more than 50% of people seek re-admission within 6 months
after treatment and the average duration of hospital stay is 6 days.
Heart failure is a leading cause of hospital readmissions in the
U.S. People aged 65 and older were readmitted at a rate of 24.5 per 100
admissions in 2011. In the same year, people under Medicaid were
readmitted at a rate of 30.4 per 100 admissions, and uninsured people
were readmitted at a rate of 16.8 per 100 admissions. These are the
highest readmission rates for both categories. Notably, heart failure
was not among the top ten conditions with the most 30-day readmissions
among the privately insured.
United Kingdom
In the UK, despite moderate improvements in prevention, heart failure rates have increased due to population growth and ageing. Overall heart failure rates are similar to the four most common causes of cancer (breast, lung, prostate and colon) combined. People from deprived backgrounds are more likely to be diagnosed with heart failure and at a younger age.
Developing world
In tropical countries, the most common cause of HF is valvular heart disease or some type of cardiomyopathy. As underdeveloped countries have become more affluent, there has also been an increase in the incidence of diabetes, hypertension and obesity, which have in turn raised the incidence of heart failure.
Sex
Men have a
higher incidence of heart failure, but the overall prevalence rate is
similar in both sexes since women survive longer after the onset of
heart failure. Women tend to be older when diagnosed with heart failure (after menopause),
they are more likely than men to have diastolic dysfunction, and seem
to experience a lower overall quality of life than men after diagnosis.
Ethnicity
Some sources state that people of Asian descent are at a higher risk of heart failure than other ethnic groups. Other sources however have found that rates of heart failure are similar to rates found in other ethnic groups.
Economics
In
2011, non-hypertensive heart failure was one of the ten most expensive
conditions seen during inpatient hospitalizations in the U.S., with
aggregate inpatient hospital costs of more than $10.5 billion.
Heart failure is associated with a high health expenditure,
mostly because of the cost of hospitalizations; costs have been
estimated to amount to 2% of the total budget of the National Health Service in the United Kingdom, and more than $35 billion in the United States.
Research directions
There is low-quality evidence that stem cell therapy may help.
Although this evidence positively indicated benefit, the evidence was
of lower quality than other evidence that does not indicate benefit.
A 2016 Cochrane review found tentative evidence of longer life
expectancy and improved left ventricular ejection fraction in persons
treated with bone marrow-derived stem cells.