The gut–brain axis is the biochemical signaling that takes place between the gastrointestinal tract (GI tract) and the central nervous system (CNS). The term "gut–brain axis" is occasionally used to refer to the role of the gut flora in the interplay as well, whereas the term "microbiota–gut–brain (MGB or BGM) axis" explicitly includes the role of gut flora in the biochemical signaling events that take place between the GI tract and CNS.
Broadly defined, the gut–brain axis includes the central nervous system, neuroendocrine and neuroimmune systems, including the hypothalamic–pituitary–adrenal axis (HPA axis), sympathetic and parasympathetic arms of the autonomic nervous system, including the enteric nervous system and the vagus nerve, and the gut microbiota. The first of the brain–gut interactions shown, was the cephalic phase of digestion, in the release of gastric and pancreatic secretions in response to sensory signals, such as the smell and sight of food. This was first demonstrated by Pavlov.
Interest in the field was sparked by a 2004 study showing that germ-free (GF) mice showed an exaggerated HPA axis response to stress compared to non-GF laboratory mice.
As of October 2016, most of the work done on the role of gut flora in the gut–brain axis had been conducted in animals, or on characterizing the various neuroactive compounds that gut flora can produce. Studies with humans – measuring variations in gut flora between people with various psychiatric and neurological conditions or when stressed, or measuring effects of various probiotics (dubbed "psychobiotics" in this context) – had generally been small and were just beginning to be generalized. Whether changes to gut flora are a result of disease, a cause of disease, or both in any number of possible feedback loops in the gut–brain axis, remained unclear.
Gut flora
The gut flora is the complex community of microorganisms that live in the digestive tracts of humans and other animals. The gut metagenome is the aggregate of all the genomes of gut microbiota. The gut is one niche that human microbiota inhabit.
In humans, the gut microbiota has the largest quantity of bacteria and the greatest number of species, compared to other areas of the body. In humans, the gut flora is established at one to two years after birth; by that time, the intestinal epithelium and the intestinal mucosal barrier that it secretes have co-developed in a way that is tolerant to, and even supportive of, the gut flora and that also provides a barrier to pathogenic organisms.
The relationship between gut flora and humans is not merely commensal (a non-harmful coexistence), but rather a mutualistic relationship. Human gut microorganisms benefit the host by collecting the energy from the fermentation of undigested carbohydrates and the subsequent absorption of short-chain fatty acids (SCFAs), acetate, butyrate, and propionate. Intestinal bacteria also play a role in synthesizing vitamin B and vitamin K as well as metabolizing bile acids, sterols, and xenobiotics. The systemic importance of the SCFAs and other compounds they produce are like hormones and the gut flora itself appears to function like an endocrine organ; dysregulation of the gut flora has been correlated with a host of inflammatory and autoimmune conditions.
The composition of human gut flora changes over time, when the diet changes, and as overall health changes.
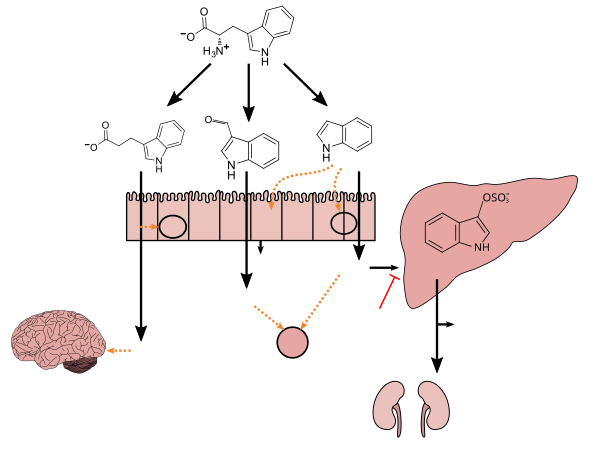
Tryptophan metabolism by human gastrointestinal microbiota
This diagram shows the biosynthesis of bioactive compounds (indole and certain other derivatives) from tryptophan by bacteria in the gut. Indole is produced from tryptophan by bacteria that express tryptophanase. Clostridium sporogenes metabolizes tryptophan into indole and subsequently 3-indolepropionic acid (IPA), a highly potent neuroprotective antioxidant that scavenges hydroxyl radicals. IPA binds to the pregnane X receptor (PXR) in intestinal cells, thereby facilitating mucosal homeostasis and barrier function. Following absorption from the intestine and distribution to the brain, IPA confers a neuroprotective effect against cerebral ischemia and Alzheimer's disease. Lactobacillus species metabolize tryptophan into indole-3-aldehyde (I3A) which acts on the aryl hydrocarbon receptor (AhR) in intestinal immune cells, in turn increasing interleukin-22 (IL-22) production. Indole itself triggers the secretion of glucagon-like peptide-1 (GLP-1) in intestinal L cells and acts as a ligand for AhR. Indole can also be metabolized by the liver into indoxyl sulfate, a compound that is toxic in high concentrations and associated with vascular disease and renal dysfunction. AST-120 (activated charcoal), an intestinal sorbent that is taken by mouth, adsorbs indole, in turn decreasing the concentration of indoxyl sulfate in blood plasma. |
Enteric nervous system
The enteric nervous system is one of the main divisions of the nervous system and consists of a mesh-like system of neurons that governs the function of the gastrointestinal system; it has been described as a "second brain" for several reasons. The enteric nervous system can operate autonomously. It normally communicates with the central nervous system (CNS) through the parasympathetic (e.g., via the vagus nerve) and sympathetic (e.g., via the prevertebral ganglia) nervous systems. However, vertebrate studies show that when the vagus nerve is severed, the enteric nervous system continues to function.
In vertebrates, the enteric nervous system includes efferent neurons, afferent neurons, and interneurons, all of which make the enteric nervous system capable of carrying reflexes in the absence of CNS input. The sensory neurons report on mechanical and chemical conditions. Through intestinal muscles, the motor neurons control peristalsis and churning of intestinal contents. Other neurons control the secretion of enzymes. The enteric nervous system also makes use of more than 30 neurotransmitters, most of which are identical to the ones found in CNS, such as acetylcholine, dopamine, and serotonin. More than 90% of the body's serotonin lies in the gut, as well as about 50% of the body's dopamine; the dual function of these neurotransmitters is an active part of gut–brain research.
The first of the gut–brain interactions was shown to be between the sight and smell of food and the release of gastric secretions, known as the cephalic phase, or cephalic response of digestion.
Gut–brain integration
The gut–brain axis, a bidirectional neurohumoral communication system, is important for maintaining homeostasis and is regulated through the central and enteric nervous systems and the neural, endocrine, immune, and metabolic pathways, and especially including the hypothalamic–pituitary–adrenal axis (HPA axis). That term has been expanded to include the role of the gut flora as part of the "microbiome-gut-brain axis", a linkage of functions including the gut flora.
Interest in the field was sparked by a 2004 study (Nobuyuki Sudo and Yoichi Chida) showing that germ-free mice (genetically homogeneous laboratory mice, birthed and raised in an antiseptic environment) showed an exaggerated HPA axis response to stress, compared to non-GF laboratory mice.
The gut flora can produce a range of neuroactive molecules, such as acetylcholine, catecholamines, γ-aminobutyric acid, histamine, melatonin, and serotonin, which are essential for regulating peristalsis and sensation in the gut. Changes in the composition of the gut flora due to diet, drugs, or disease correlate with changes in levels of circulating cytokines, some of which can affect brain function. The gut flora also release molecules that can directly activate the vagus nerve, which transmits information about the state of the intestines to the brain.
Likewise, chronic or acutely stressful situations activate the hypothalamic–pituitary–adrenal axis, causing changes in the gut flora and intestinal epithelium, and possibly having systemic effects. Additionally, the cholinergic anti-inflammatory pathway, signaling through the vagus nerve, affects the gut epithelium and flora. Hunger and satiety are integrated in the brain, and the presence or absence of food in the gut and types of food present also affect the composition and activity of gut flora.
That said, most of the work that has been done on the role of gut flora in the gut–brain axis has been conducted in animals, including the highly artificial germ-free mice. As of 2016, studies with humans measuring changes to gut flora in response to stress, or measuring effects of various probiotics, have generally been small and cannot be generalized; whether changes to gut flora are a result of disease, a cause of disease, or both in any number of possible feedback loops in the gut–brain axis, remains unclear.
The history of ideas about a relationship between the gut and the mind dates from the nineteenth century. The concepts of dyspepsia and neurasthenia gastrica referred to the influence of the gut on human emotions and thoughts.
Gut-brain-skin axis
A unifying theory that tied gastrointestinal mechanisms to anxiety, depression, and skin conditions such as acne was proposed as early as 1930. In a paper in 1930, it was proposed that emotional states might alter normal intestinal flora which could lead to increased intestinal permeability and therefore contribute to systemic inflammation. Many aspects of this theory have been validated since then. Gut microbiota and oral probiotics have been found to influence systemic inflammation, oxidative stress, glycemic control, tissue lipid content, and mood.
Research
Probiotics
A 2016 systematic review of laboratory animal studies and preliminary human clinical trials using commercially available strains of probiotic bacteria found that certain species of the Bifidobacterium and Lactobacillus genera (i.e., B. longum, B. breve, B. infantis, L. helveticus, L. rhamnosus, L. plantarum, and L. casei) had the most potential to be useful for certain central nervous system disorders.
Anxiety and mood disorders
As of 2018 work on the relationship between gut flora and anxiety disorders and mood disorders, as well as attempts to influence that relationship using probiotics or prebiotics (called "psychobiotics"), was at an early stage, with insufficient evidence to draw conclusions about a causal role for gut flora changes in these conditions, or about the efficacy of any probiotic or prebiotic treatment.
People with anxiety and mood disorders tend to have gastrointestinal problems; small studies have been conducted to compare the gut flora of people with major depressive disorder and healthy people, but those studies have had contradictory results.
Much interest was generated in the potential role of gut flora in anxiety disorders, and more generally in the role of gut flora in the gut–brain axis, by studies published in 2004 showing that germ-free mice have an exaggerated HPA axis response to stress caused by being restrained, which was reversed by colonizing their gut with a Bifidobacterium species. Studies looking at maternal separation for rats shows neonatal stress leads to long-term changes in the gut microbiota such as its diversity and composition, which also led to stress and anxiety-like behavior. Additionally, while much work had been done as of 2016 to characterize various neurotransmitters known to be involved in anxiety and mood disorders that gut flora can produce (for example, Escherichia, Bacillus, and Saccharomyces species can produce noradrenalin; Candida, Streptococcus, and Escherichia species can produce serotonin, etc.) the interrelationships and pathways by which the gut flora might affect anxiety in humans were unclear.
In one study, germ-free mice underwent fecal transplants with microbes from humans with or without major depressive disorder (MDD). Mice with microbes from humans with MDD displayed more behaviors associated with anxiety and depression than mice transplanted with microbes from humans without MDD. The taxonomic composition of microbiota between depressed patients and healthy patients, as well as between the respective mice, also differed. Germ-free mice in another study also displayed behaviors associated with anxiety and depression as compared to mice with normal microbiota, and had higher levels of corticosterone after exposure to behavioral tests. Using rodents in microbiome and mental health studies allows researchers to compare behavior and microbial composition of rodents to humans, ideally to elucidate therapeutic application for mental disorders.
Additionally, there is a link between the gut microbiome, mood disorders and anxiety, and sleep. The microbial composition of the gut microbiome changes depending on the time of day, meaning that throughout the day, the gut is exposed to varying metabolites produced by the microbes active during that time. These time-dependent microbial changes are associated with differences in the transcription of circadian clock genes involved in circadian rhythm. One mouse study showed that altering clock gene transcription by disrupting circadian rhythm, such as through sleep deprivation, potentially has a direct effect on the composition of the gut microbiome. Another study found that mice that could not produce the CLOCK protein, made by a clock gene, were more likely to develop depression. Stress and sleep disturbances can lead to greater gut mucosal permeability via activation of the HPA axis. This in turn causes immune inflammatory responses that contribute to the development of illnesses that cause depression and anxiety.
Autism
Around 70% of people with autism also have gastrointestinal problems, and autism is often diagnosed at the time that the gut flora becomes established, indicating that there may be a connection between autism and gut flora. Some studies have found differences in the gut flora of children with autism compared with children without autism – most notably elevations in the amount of Clostridium in the stools of children with autism compared with the stools of the children without – but these results have not been consistently replicated. Many of the environmental factors thought to be relevant to the development of autism would also affect the gut flora, leaving open the question of whether specific developments in the gut flora drive the development of autism or whether those developments happen concurrently. As of 2016, studies with probiotics had only been conducted with animals; studies of other dietary changes to treat autism have been inconclusive.
Parkinson's disease
As of 2015, one study had been conducted comparing the gut flora of people with Parkinson's disease to healthy controls; in that study people with Parkinson's had lower levels of Prevotellaceae and people with Parkinson's who had higher levels of Enterobacteriaceae had more clinically severe symptoms; the authors of the study drew no conclusions about whether gut flora changes were driving the disease or vice versa.