| Hypercholesterolemia | |
|---|---|
| Synonyms | Hypercholesterolaemia, high cholesterol |
 | |
| Xanthelasma palpebrarum, yellowish patches consisting of cholesterol deposits above the eyelids. These are more common in people with familial hypercholesterolemia. | |
| Specialty | Cardiology |
Hypercholesterolemia, also called high cholesterol, is the presence of high levels of cholesterol in the blood. It is a form of hyperlipidemia, high blood lipids, and hyperlipoproteinemia (elevated levels of lipoproteins in the blood).
Elevated levels of non-HDL cholesterol and LDL in the blood may be a consequence of diet, obesity, inherited (genetic) diseases (such as LDL receptor mutations in familial hypercholesterolemia), or the presence of other diseases such as type 2 diabetes and an underactive thyroid.
Cholesterol is one of three major classes of lipids which all animal cells use to construct their membranes and is thus manufactured by all animal cells. Plant cells do not manufacture cholesterol. It is also the precursor of the steroid hormones and bile acids. Since cholesterol is insoluble in water, it is transported in the blood plasma within protein particles (lipoproteins). Lipoproteins are classified by their density: very low density lipoprotein (VLDL), intermediate density lipoprotein (IDL), low density lipoprotein (LDL) and high density lipoprotein (HDL). All the lipoproteins carry cholesterol, but elevated levels of the lipoproteins other than HDL (termed non-HDL cholesterol), particularly LDL-cholesterol, are associated with an increased risk of atherosclerosis and coronary heart disease. In contrast, higher levels of HDL cholesterol are protective.
Avoiding trans fats and replacing saturated fats in adult diets with polyunsaturated fats are recommended dietary measures to reduce total blood cholesterol and LDL in adults. In people with very high cholesterol (e.g., familial hypercholesterolemia), diet is often not sufficient to achieve the desired lowering of LDL, and lipid-lowering medications are usually required. If necessary, other treatments such as LDL apheresis or even surgery (for particularly severe subtypes of familial hypercholesterolemia) are performed. About 34 million adults in the United States have high blood cholesterol.
Signs and symptoms
Although hypercholesterolemia itself is asymptomatic, longstanding elevation of serum cholesterol can lead to atherosclerosis (hardening of arteries). Over a period of decades, elevated serum cholesterol contributes to formation of atheromatous plaques in the arteries. This can lead to progressive narrowing of the involved arteries. Alternatively smaller plaques may rupture and cause a clot to form and obstruct blood flow. A sudden blockage of a coronary artery may result in a heart attack. A blockage of an artery supplying the brain can cause a stroke.
If the development of the stenosis or occlusion is gradual, blood
supply to the tissues and organs slowly diminishes until organ function
becomes impaired. At this point tissue ischemia (restriction in blood supply) may manifest as specific symptoms. For example, temporary ischemia of the brain (commonly referred to as a transient ischemic attack) may manifest as temporary loss of vision, dizziness and impairment of balance, difficulty speaking, weakness or numbness or tingling, usually on one side of the body. Insufficient blood supply to the heart may cause chest pain, and ischemia of the eye may manifest as transient visual loss in one eye. Insufficient blood supply to the legs may manifest as calf pain when walking, while in the intestines it may present as abdominal pain after eating a meal.
Some types of hypercholesterolemia lead to specific physical
findings. For example, familial hypercholesterolemia (Type IIa
hyperlipoproteinemia) may be associated with xanthelasma palpebrarum (yellowish patches underneath the skin around the eyelids), arcus senilis (white or gray discoloration of the peripheral cornea), and xanthomata (deposition of yellowish cholesterol-rich material) of the tendons, especially of the fingers. Type III hyperlipidemia may be associated with xanthomata of the palms, knees and elbows.
Causes
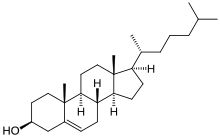
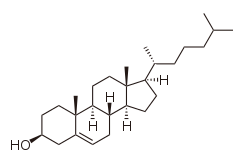
Formula structure of cholesterol
Hypercholesterolemia is typically due to a combination of environmental and genetic factors. Environmental factors include weight, diet, and stress.
A number of other conditions can also increase cholesterol levels including diabetes mellitus type 2, obesity, alcohol use, monoclonal gammopathy, dialysis, nephrotic syndrome, hypothyroidism, Cushing’s syndrome, anorexia nervosa, medications (e.g., thiazide diuretics, ciclosporin, glucocorticoids, beta blockers, retinoic acid, antipsychotics).
Genetic contributions are usually due to the additive effects of
multiple genes, though occasionally may be due to a single gene defect
such as in the case of familial hypercholesterolaemia. and Acute Intermittent Porphyria, a mutation of the HMBS gene.
Genetic abnormalities are in some cases completely responsible
for hypercholesterolemia, such as in familial hypercholesterolemia,
where one or more genetic mutations in the autosomal dominant APOB gene exist, the autosomal recessive LDLRAP1 gene, autosomal dominant familial hypercholesterolemia (HCHOLA3) variant of the PCSK9 gene, or the LDL receptor gene. Familial hypercholesterolemia affects about one in five hundred people.
Diet
Diet has an effect on blood cholesterol, but the size of this effect varies between individuals. Moreover, when dietary cholesterol intake goes down, production (principally by the liver) typically increases, so that blood cholesterol changes can be modest
or even elevated. This compensatory response may explain
hypercholesterolemia in anorexia nervosa. A 2016 review found tentative
evidence that dietary cholesterol is associated with higher blood
cholesterol. Trans fats have been shown to reduce levels of HDL while increasing levels of LDL. LDL and total cholesterol also increases by very high fructose intake.
Hormonal effects
Glucocorticoids increase cholesterol LDL production by increasing production and activity of HMG-CoA reductase. These include the physiologic stress hormone cortisol and commonly used medicines for asthma, rheumatoid arthritis, or connective tissue disorders. Other steroid hormones and drugs are also implicated. In contrast, the thyroid hormone decreases cholesterol production. Hence, hypothyroidism (lack of thyroid hormone) causes hypercholesterolemia.
Medications
Hypercholesterolemia
may be a side effect of a number of medications, including blood
pressure medication, antipsychotics, anticonvulsants,
immunosuppressives, human immunodeficiency virus therapy, and
interferons.
Diagnosis
| Interpretation of cholesterol levels | |||
|---|---|---|---|
| cholesterol type | mg/dL | mmol/L | interpretation |
| total cholesterol | <200 span=""> | <5 .2="" span=""> | desirable |
| 200–239 | 5.2–6.2 | borderline | |
| >240 | >6.2 | high | |
| LDL cholesterol | <100 span=""> | <2 .6="" span=""> | most desirable |
| 100–129 | 2.6–3.3 | good | |
| 130–159 | 3.4–4.1 | borderline high | |
| 160–189 | 4.1–4.9 | high and undesirable | |
| >190 | >4.9 | very high | |
| HDL cholesterol | <40 span=""> | <1 .0="" span=""> | undesirable; risk increased |
| 41–59 | 1.0–1.5 | okay, but not optimal | |
| >60 | >1.55 | good; risk lowered | |
| Indications to lower LDL cholesterol | |||
|---|---|---|---|
| Coronary risk | because they have... | should consider | reduction indicated |
| high | >20% risk of MI in 10 years, or risk factor such as coronary heart disease, diabetes, peripheral-artery disease, carotid-artery disease, or aortic aneurysm | >70 mg/dL, 3.88 mmol/L especially if there are risk factors | >100 mg/dL, 5.55 mmol/L |
| moderately high | 10–20% risk of MI in 10 years and > 1 risk factors | >100 mg/dL, 5.55 mmol/L | >130 mg/dL, 7.21 mmol/L |
| moderate | <10 10="" in="" mi="" of="" risk="" years=""> 1 risk factors | >130 mg/dL, 7.21 mmol/L | >160 mg/dL, 8.88 mmol/L |
| low | No or one risk factor | >160 mg/dL, 8.88 mmol/L | >190 mg/dL, 10.5 mmol/L |
Cholesterol is measured in milligrams per deciliter (mg/dL) of blood
in the United States and some other countries. In the United Kingdom,
most European countries and Canada, millimoles per liter of blood
(mmol/Ll) is the measure.
For healthy adults, the UK National Health Service recommends
upper limits of total cholesterol of 5 mmol/L, and low-density
lipoprotein cholesterol (LDL) of 3 mmol/L. For people at high risk of
cardiovascular disease, the recommended limit for total cholesterol is
4 mmol/L, and 2 mmol/L for LDL.
In the United States, the National Heart, Lung, and Blood
Institute within the National Institutes of Health classifies total
cholesterol of less than 200 mg/dL as “desirable,” 200 to 239 mg/dL as
“borderline high,” and 240 mg/dL or more as “high”.
No absolute cutoff between normal and abnormal cholesterol levels
exists, and interpretation of values must be made in relation to other
health conditions and risk factors.
Higher levels of total cholesterol increase the risk of cardiovascular disease, particularly coronary heart disease. Levels of LDL or non-HDL cholesterol both predict future coronary heart disease; which is the better predictor is disputed.
High levels of small dense LDL may be particularly adverse, although
measurement of small dense LDL is not advocated for risk prediction. In the past, LDL and VLDL levels were rarely measured directly due to cost. Levels of fasting triglycerides were taken as an indicator of VLDL levels (generally about 45% of
fasting triglycerides is composed of VLDL), while LDL was usually
estimated by the Friedewald formula:
LDL total cholesterol - HDL - (0.2 x fasting triglycerides).
However, this equation is not valid on nonfasting blood samples
or if fasting triglycerides are elevated more than 4.5 mmol/L (more than
∼400 mg/dL). Recent guidelines have, therefore, advocated the use of
direct methods for measurement of LDL wherever possible.
It may be useful to measure all lipoprotein subfractions ( VLDL, IDL, LDL, and HDL) when assessing hypercholesterolemia and measurement of apolipoproteins and lipoprotein (a) can also be of value. Genetic screening is now advised if a form of familial hypercholesterolemia is suspected.
Classification
Classically, hypercholesterolemia was categorized by lipoprotein electrophoresis and the Fredrickson classification.
Newer methods, such as "lipoprotein subclass analysis", have offered
significant improvements in understanding the connection with
atherosclerosis progression and clinical consequences. If the
hypercholesterolemia is hereditary (familial hypercholesterolemia), more often a family history of premature, earlier onset atherosclerosis is found.
Screening
Two bags of fresh frozen plasma: The bag on the left was obtained from a donor with hyperlipidemia, while the other bag was obtained from a donor with normal serum lipid levels.
The U.S. Preventive Services Task Force
in 2008 strongly recommends routine screening for men 35 years and
older and women 45 years and older for lipid disorders and the treatment
of abnormal lipids in people who are at increased risk of coronary
heart disease. They also recommend routinely screening men aged 20 to 35
years and women aged 20 to 45 years if they have other risk factors for
coronary heart disease. In 2016 they concluded that testing the general population under the age of 40 without symptoms is of unclear benefit.
In Canada, screening is recommended for men 40 and older and women 50 and older. In those with normal cholesterol levels, screening is recommended once every five years. Once people are on a statin further testing provides little benefit except to possibly determine compliance with treatment.
Treatment
For those at high risk, a combination of lifestyle modification and statins has been shown to decrease mortality.
Lifestyle
Lifestyle
changes recommended for those with high cholesterol include: smoking
cessation, limiting alcohol consumption, increasing physical activity,
and maintaining a healthy weight.
Overweight or obese individuals can lower blood cholesterol by
losing weight – on average a kilogram of weight loss can reduce LDL
cholesterol by 0.8 mg/dl.
Diet
Eating a
diet with a high proportion of vegetables, fruit, dietary fiber, and low
in fats results in a modest decrease in total cholesterol.
Eating dietary cholesterol causes a small but significant rise in serum cholesterol. Dietary limits for cholesterol were proposed in United States, but not in Canada, United Kingdom, and Australia. Consequently, in 2015 the Dietary Guidelines Advisory Committee in the United States removed its recommendation of limiting cholesterol intake.
A 2015 Cochrane review found replacing saturated fat with polyunsaturated fat resulted in a small decrease in cardiovascular disease by decreasing blood cholesterol. Other reviews have not found an effect from saturated fats on cardiovascular disease. Trans fats
are recognized as a potential risk factor for cholesterol-related
cardiovascular disease, and avoiding them in an adult diet is
recommended.
The National Lipid Association recommends that people with familial hypercholesterolemia
restrict intakes of total fat to 25–35% of energy intake, saturated fat
to less than 7% of energy intake, and cholesterol to less than 200 mg
per day. Changes in total fat intake in low calorie diets do not appear to affect blood cholesterol.
Increasing soluble fiber consumption has been shown to reduce
levels of LDL cholesterol, with each additional gram of soluble fiber
reducing LDL by an average of 2.2 mg/dL (0.057 mmol/L). Increasing consumption of whole grains also reduces LDL cholesterol, with whole grain oats being particularly effective. Inclusion of 2 g per day of phytosterols and phytostanols and 10 to 20 g per day of soluble fiber decreases dietary cholesterol absorption. A diet high in fructose can raise LDL cholesterol levels in the blood.
Medication
Statins are the typically used medications, in addition to healthy lifestyle interventions. Statins can reduce total cholesterol by about 50% in the majority of people, and are effective in reducing the risk of cardiovascular disease in both people with and without pre-existing cardiovascular disease.
In people without cardiovascular disease, statins have been shown to
reduce all-cause mortality, fatal and non-fatal coronary heat disease,
and strokes. Greater benefit is observed with the use of high-intensity statin therapy. Statins may improve quality of life when used in people without existing cardiovascular disease (i.e. for primary prevention). Statins decrease cholesterol in children with hypercholesterolemia, but no studies as of 2010 show improved outcomes and diet is the mainstay of therapy in childhood.
Other agents that may be used include fibrates, nicotinic acid, and cholestyramine. These, however, are only recommended if statins are not tolerated or in pregnant women. Injectable antibodies against the protein PCSK9 (evolocumab, bococizumab, alirocumab) can reduce LDL cholesterol and have been shown to reduce mortality.
Alternative medicine
According to a survey in 2002, alternative medicine
was used in an attempt to treat cholesterol by 1.1% of U.S. adults.
Consistent with previous surveys, this one found the majority of
individuals (55%) used it in conjunction with conventional medicine.
A review of trials of phytosterols and/or phytostanols, average dose 2.15 g/day, reported an average of 9% lowering of LDL-cholesterol.
In 2000, the Food and Drug Administration approved the labeling of
foods containing specified amounts of phytosterol esters or phytostanol
esters as cholesterol-lowering; in 2003, an FDA Interim Health Claim
Rule extended that label claim to foods or dietary supplements
delivering more than 0.8 g/day of phytosterols or phytostanols. Some
researchers, however, are concerned about diet supplementation with
plant sterol esters and draw attention to lack of long-term safety data.
Epidemiology
Rates of high total cholesterol in the United States in 2010 are just over 13%, down from 17% in 2000.
Average total cholesterol in the United Kingdom is 5.9 mmol/L,
while in rural China and Japan, average total cholesterol is 4 mmol/L. Rates of coronary artery disease are high in Great Britain, but low in rural China and Japan.
Research
Various clinical practice guidelines have addressed the treatment of hypercholesterolemia.
The National Cholesterol Education Program revised their guidelines; however, their 2004 revisions have been criticized for use of nonrandomized, observational data.
In the UK, the National Institute for Health and Clinical Excellence has made recommendations for the treatment of elevated cholesterol levels, published in 2008.
The Task Force for the management of dyslipidaemias of the
European Society of Cardiology and the European Atherosclerosis Society
published guidelines for the management of dyslipidaemias in 2011.
Gene therapy is being studied as a potential treatment.
Special populations
Among people whose life expectancy is relatively short, hypercholesterolemia is not a risk factor for death by any cause including coronary heart disease. Among people older than 70, hypercholesterolemia is not a risk factor for being hospitalized with myocardial infarction or angina. There are also increased risks in people older than 85 in the use of statin drugs. Because of this, medications which lower lipid levels should not be routinely used among people with limited life expectancy.
The American College of Physicians recommends for hypercholesterolemia in people with diabetes:
- Lipid-lowering therapy should be used for secondary prevention of cardiovascular mortality and morbidity for all adults with known coronary artery disease and type 2 diabetes.
- Statins should be used for primary prevention against macrovascular complications in adults with type 2 diabetes and other cardiovascular risk factors.
- Once lipid-lowering therapy is initiated, people with type 2 diabetes mellitus should be taking at least moderate doses of a statin.
- For those people with type 2 diabetes who are taking statins, routine monitoring of liver function tests or muscle enzymes is not recommended except in specific circumstances.