From Wikipedia, the free encyclopedia
Apoptosis
begins when the nucleus of the cell begins to shrink. After the
shrinking, the plasma membrane blebs and folds around different
organelles. The blebs continue to form and the organelles fragment and
move away from one another.
Apoptosis (from Ancient Greek ἀπόπτωσις, apóptōsis, "falling off") is a form of programmed cell death that occurs in multicellular organisms. Biochemical events lead to characteristic cell changes (morphology) and death. These changes include blebbing, cell shrinkage, nuclear fragmentation, chromatin condensation, chromosomal DNA fragmentation, and global mRNA decay. The average adult human loses between 50 and 70 billion cells each day due to apoptosis. For an average human child between the ages of 8 and 14, approximately 20–30 billion cells die per day.
In contrast to necrosis,
which is a form of traumatic cell death that results from acute
cellular injury, apoptosis is a highly regulated and controlled process
that confers advantages during an organism's life cycle. For example,
the separation of fingers and toes in a developing human embryo occurs because cells between the digits undergo apoptosis. Unlike necrosis, apoptosis produces cell fragments called apoptotic bodies that phagocytic cells are able to engulf and remove before the contents of the cell can spill out onto surrounding cells and cause damage to them.
Because apoptosis cannot stop once it has begun, it is a highly
regulated process. Apoptosis can be initiated through one of two
pathways. In the intrinsic pathway the cell kills itself because it senses cell stress, while in the extrinsic pathway
the cell kills itself because of signals from other cells. Weak
external signals may also activate the intrinsic pathway of apoptosis. Both pathways induce cell death by activating caspases, which are proteases,
or enzymes that degrade proteins. The two pathways both activate
initiator caspases, which then activate executioner caspases, which then
kill the cell by degrading proteins indiscriminately.
In addition to its importance as a biological phenomenon,
defective apoptotic processes have been implicated in a wide variety of
diseases. Excessive apoptosis causes atrophy, whereas an insufficient amount results in uncontrolled cell proliferation, such as cancer. Some factors like Fas receptors and caspases promote apoptosis, while some members of the Bcl-2 family of proteins inhibit apoptosis.
Discovery and etymology
German scientist Carl Vogt was first to describe the principle of apoptosis in 1842. In 1885, anatomist Walther Flemming
delivered a more precise description of the process of programmed cell
death. However, it was not until 1965 that the topic was resurrected.
While studying tissues using electron microscopy, John Foxton Ross Kerr at the University of Queensland was able to distinguish apoptosis from traumatic cell death. Following the publication of a paper describing the phenomenon, Kerr was invited to join Alastair R. Currie, as well as Andrew Wyllie, who was Currie's graduate student, at University of Aberdeen. In 1972, the trio published a seminal article in the British Journal of Cancer. Kerr had initially used the term programmed cell necrosis, but in the article, the process of natural cell death was called apoptosis. Kerr, Wyllie and Currie credited James Cormack, a professor of Greek language at University of Aberdeen, with suggesting the term apoptosis. Kerr received the Paul Ehrlich and Ludwig Darmstaedter Prize on March 14, 2000, for his description of apoptosis. He shared the prize with Boston biologist H. Robert Horvitz.
For many years, neither "apoptosis" nor "programmed cell death"
was a highly cited term. Two discoveries brought cell death from
obscurity to a major field of research: identification of components of
the cell death control and effector mechanisms, and linkage of
abnormalities in cell death to human disease, in particular cancer.
The 2002 Nobel Prize in Medicine was awarded to Sydney Brenner, Horvitz and John E. Sulston for their work identifying genes that control apoptosis. The genes were identified by studies in the nematode C. elegans and homologues of these genes function in humans to regulate apoptosis.
John E. Sulston won the Nobel Prize in Medicine in 2002, for his pioneering research on apoptosis.
In Greek, apoptosis translates to the "falling off" of leaves from a tree.
Cormack, professor of Greek language, reintroduced the term for medical
use as it had a medical meaning for the Greeks over two thousand years
before. Hippocrates used the term to mean "the falling off of the bones". Galen
extended its meaning to "the dropping of the scabs". Cormack was no
doubt aware of this usage when he suggested the name. Debate continues
over the correct pronunciation, with opinion divided between a
pronunciation with the second p silent ( ap-ə-TOH-sis) and the second p pronounced (), as in the original Greek. In English, the p of the Greek -pt- consonant cluster is typically silent at the beginning of a word (e.g. pterodactyl, Ptolemy), but articulated when used in combining forms preceded by a vowel, as in helicopter or the orders of insects: diptera, lepidoptera, etc.
In the original Kerr, Wyllie & Currie paper, there is a footnote regarding the pronunciation:
"We are most grateful to Professor James Cormack of the
Department of Greek, University of Aberdeen, for suggesting this term.
The word "apoptosis" (ἀπόπτωσις)
is used in Greek to describe the "dropping off" or "falling off" of
petals from flowers, or leaves from trees. To show the derivation
clearly, we propose that the stress should be on the penultimate
syllable, the second half of the word being pronounced like "ptosis"
(with the "p" silent), which comes from the same root "to fall", and is
already used to describe the drooping of the upper eyelid."
Activation mechanisms
Control Of The Apoptotic Mechanisms
The initiation of apoptosis is tightly regulated by activation
mechanisms, because once apoptosis has begun, it inevitably leads to the
death of the cell. The two best-understood activation mechanisms are the intrinsic pathway (also called the mitochondrial pathway) and the extrinsic pathway. The intrinsic pathway
is activated by intracellular signals generated when cells are stressed
and depends on the release of proteins from the intermembrane space of
mitochondria. The extrinsic pathway is activated by extracellular ligands binding to cell-surface death receptors, which leads to the formation of the death-inducing signaling complex (DISC).
A cell initiates intracellular apoptotic signaling in response to a stress, which may bring about cell suicide. The binding of nuclear receptors by glucocorticoids, heat, radiation, nutrient deprivation, viral infection, hypoxia, increased intracellular concentration of free fatty acids and increased intracellular calcium concentration,
for example, by damage to the membrane, can all trigger the release of
intracellular apoptotic signals by a damaged cell. A number of cellular
components, such as poly ADP ribose polymerase, may also help regulate apoptosis. Single cell fluctuations have been observed in experimental studies of stress induced apoptosis.
Before the actual process of cell death is precipitated by
enzymes, apoptotic signals must cause regulatory proteins to initiate
the apoptosis pathway. This step allows those signals to cause cell
death, or the process to be stopped, should the cell no longer need to
die. Several proteins are involved, but two main methods of regulation
have been identified: the targeting of mitochondria functionality, or directly transducing the signal via adaptor proteins
to the apoptotic mechanisms. An extrinsic pathway for initiation
identified in several toxin studies is an increase in calcium
concentration within a cell caused by drug activity, which also can
cause apoptosis via a calcium binding protease calpain.
Intrinsic pathway
The intrinsic pathway is also known as the mitochondrial pathway. Mitochondria are essential to multicellular life. Without them, a cell ceases to respire aerobically
and quickly dies. This fact forms the basis for some apoptotic
pathways. Apoptotic proteins that target mitochondria affect them in
different ways. They may cause mitochondrial swelling through the
formation of membrane pores, or they may increase the permeability of
the mitochondrial membrane and cause apoptotic effectors to leak out. They are very closely related to intrinsic pathway, and tumors arise more frequently through intrinsic pathway than the extrinsic pathway because of sensitivity. There is also a growing body of evidence indicating that nitric oxide is able to induce apoptosis by helping to dissipate the membrane potential of mitochondria and therefore make it more permeable.
Nitric oxide has been implicated in initiating and inhibiting apoptosis
through its possible action as a signal molecule of subsequent pathways
that activate apoptosis.
During apoptosis, cytochrome c is released from mitochondria through the actions of the proteins Bax and Bak.
The mechanism of this release is enigmatic, but appears to stem from a
multitude of Bax/Bak homo- and hetero-dimers of Bax/Bak inserted into
the outer membrane. Once cytochrome c is released it binds with Apoptotic protease activating factor – 1 (Apaf-1) and ATP, which then bind to pro-caspase-9 to create a protein complex known as an apoptosome. The apoptosome cleaves the pro-caspase to its active form of caspase-9, which in turn cleaves and activates pro-caspase into the effector caspase-3.
Mitochondria also release proteins known as SMACs (second mitochondria-derived activator of caspases) into the cell's cytosol following the increase in permeability of the mitochondria membranes. SMAC binds to proteins that inhibit apoptosis
(IAPs) thereby deactivating them, and preventing the IAPs from
arresting the process and therefore allowing apoptosis to proceed. IAP
also normally suppresses the activity of a group of cysteine proteases called caspases,
which carry out the degradation of the cell. Therefore, the actual
degradation enzymes can be seen to be indirectly regulated by
mitochondrial permeability.
Extrinsic pathway
Overview of signal transduction pathways.
Overview of TNF (left) and Fas (right) signalling in apoptosis, an example of direct signal transduction.
Two theories of the direct initiation of apoptotic mechanisms in mammals have been suggested: the TNF-induced (tumor necrosis factor) model and the Fas-Fas ligand-mediated model, both involving receptors of the TNF receptor (TNFR) family coupled to extrinsic signals.
TNF path
TNF-alpha is a cytokine produced mainly by activated macrophages, and is the major extrinsic mediator of apoptosis. Most cells in the human body have two receptors for TNF-alpha: TNFR1 and TNFR2.
The binding of TNF-alpha to TNFR1 has been shown to initiate the
pathway that leads to caspase activation via the intermediate membrane
proteins TNF receptor-associated death domain (TRADD) and Fas-associated death domain protein (FADD). cIAP1/2 can inhibit TNF-α signaling by binding to TRAF2. FLIP inhibits the activation of caspase-8. Binding of this receptor can also indirectly lead to the activation of transcription factors involved in cell survival and inflammatory responses. However, signalling through TNFR1 might also induce apoptosis in a caspase-independent manner.
The link between TNF-alpha and apoptosis shows why an abnormal
production of TNF-alpha plays a fundamental role in several human
diseases, especially in autoimmune diseases. The TNF-alpha receptor superfamily also includes death receptors (DRs), such as DR4 and DR5. These receptors bind to the proteinTRAIL and mediate apoptosis. Apoptosis is known to be one of the primary mechanisms of targeted cancer therapy.
Luminescent iridium complex-peptide hybrids (IPHs) have recently been
designed, which mimic TRAIL and bind to death receptors on cancer cells,
thereby inducing their apoptosis.
- Fas path
The fas receptor (First apoptosis signal) – (also known as Apo-1 or CD95) is a transmembrane protein of the TNF family which binds the Fas ligand (FasL). The interaction between Fas and FasL results in the formation of the death-inducing signaling complex
(DISC), which contains the FADD, caspase-8 and caspase-10. In some
types of cells (type I), processed caspase-8 directly activates other
members of the caspase family, and triggers the execution of apoptosis
of the cell. In other types of cells (type II), the Fas-DISC
starts a feedback loop that spirals into increasing release of
proapoptotic factors from mitochondria and the amplified activation of
caspase-8.
- Common components
Following TNF-R1 and Fas activation in mammalian cells a balance between proapoptotic (BAX, BID, BAK, or BAD) and anti-apoptotic (Bcl-Xl and Bcl-2) members of the Bcl-2 family are established. This balance is the proportion of proapoptotic homodimers
that form in the outer-membrane of the mitochondrion. The proapoptotic
homodimers are required to make the mitochondrial membrane permeable for
the release of caspase activators such as cytochrome c and SMAC.
Control of proapoptotic proteins under normal cell conditions of
nonapoptotic cells is incompletely understood, but in general, Bax or
Bak are activated by the activation of BH3-only proteins, part of the Bcl-2 family.
- Caspases
Caspases
play the central role in the transduction of ER apoptotic signals.
Caspases are proteins that are highly conserved, cysteine-dependent
aspartate-specific proteases. There are two types of caspases: initiator
caspases, caspase 2,8,9,10,11,12, and effector caspases, caspase 3,6,7.
The activation of initiator caspases requires binding to specific
oligomeric activator protein. Effector caspases are then activated by these active initiator caspases through proteolytic
cleavage. The active effector caspases then proteolytically degrade a
host of intracellular proteins to carry out the cell death program.
- Caspase-independent apoptotic pathway
There also exists a caspase-independent apoptotic pathway that is mediated by AIF (apoptosis-inducing factor).
Apoptosis model in amphibians
Amphibian frog Xenopus laevis
serves as an ideal model system for the study of the mechanisms of
apoptosis. In fact, iodine and thyroxine also stimulate the spectacular
apoptosis of the cells of the larval gills, tail and fins in amphibians
metamorphosis, and stimulate the evolution of their nervous system
transforming the aquatic, vegetarian tadpole into the terrestrial,
carnivorous frog.
Negative regulators of apoptosis
Negative regulation of apoptosis inhibits cell death signaling pathways, helping tumors to evade cell death and developing drug resistance. The ratio between anti-apoptotic (Bcl-2) and pro-apoptotic (Bax) proteins determines whether a cell lives or dies. Many families of proteins act as negative regulators categorized into either antiapoptotic factors, such as IAPs and Bcl-2 proteins or prosurvival factors like cFLIP, BNIP3, FADD, Akt, and NF-κB.[49]
Proteolytic caspase cascade: Killing the cell
Many
pathways and signals lead to apoptosis, but these converge on a single
mechanism that actually causes the death of the cell. After a cell
receives stimulus, it undergoes organized degradation of cellular
organelles by activated proteolytic caspases. In addition to the destruction of cellular organelles, mRNA is rapidly and globally degraded by a mechanism that is not yet fully characterized. mRNA decay is triggered very early in apoptosis.
A cell undergoing apoptosis shows a series of characteristic morphological changes. Early alterations include:
- Cell shrinkage and rounding occur because of the retraction lamellipodia and the breakdown of the proteinaceous cytoskeleton by caspases.
- The cytoplasm appears dense, and the organelles appear tightly packed.
- Chromatin undergoes condensation into compact patches against the nuclear envelope (also known as the perinuclear envelope) in a process known as pyknosis, a hallmark of apoptosis.
- The nuclear envelope becomes discontinuous and the DNA inside it is fragmented in a process referred to as karyorrhexis. The nucleus breaks into several discrete chromatin bodies or nucleosomal units due to the degradation of DNA.
Apoptosis progresses quickly and its products are quickly removed,
making it difficult to detect or visualize on classical histology
sections. During karyorrhexis, endonuclease activation leaves short DNA fragments, regularly spaced in size. These give a characteristic "laddered" appearance on agar gel after electrophoresis. Tests for DNA laddering differentiate apoptosis from ischemic or toxic cell death.
Apoptotic cell disassembly
Different steps in apoptotic cell disassembly.
Before the apoptotic cell is disposed of, there is a process of
disassembly. There are three recognized steps in apoptotic cell
disassembly:
- Membrane blebbing: The cell membrane shows irregular buds known as blebs. Initially these are smaller surface blebs. Later these can grow into larger so-called dynamic membrane blebs.[58] An important regulator of apoptotic cell membrane blebbing is ROCK1 (rho associated coiled-coil-containing protein kinase 1).
- Formation of membrane protrusions: Some cell types, under specific
conditions, may develop different types of long, thin extensions of the
cell membrane called membrane protrusions. Three types have been
described: microtubule spikes, apoptopodia (feet of death), and beaded apoptopodia (the latter having a beads-on-a-string appearance). Pannexin 1 is an important component of membrane channels involved in the formation of apoptopodia and beaded apoptopodia.
- Fragmentation: The cell breaks apart into multiple vesicles called apoptotic bodies, which undergo phagocytosis. The plasma membrane protrusions may help bring apoptotic bodies closer to phagocytes.
Removal of dead cells
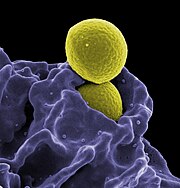
The removal of dead cells by neighboring phagocytic cells has been termed efferocytosis.
Dying cells that undergo the final stages of apoptosis display phagocytotic molecules, such as phosphatidylserine, on their cell surface.
Phosphatidylserine is normally found on the inner leaflet surface of
the plasma membrane, but is redistributed during apoptosis to the
extracellular surface by a protein known as scramblase. These molecules mark the cell for phagocytosis by cells possessing the appropriate receptors, such as macrophages. The removal of dying cells by phagocytes occurs in an orderly manner without eliciting an inflammatory response.
During apoptosis cellular RNA and DNA are separated from each other and
sorted to different apoptotic bodies; separation of RNA is initiated as
nucleolar segregation.
Pathway knock-outs
Many knock-outs have been made in the apoptosis pathways to test the function of each of the proteins. Several caspases, in addition to APAF1 and FADD,
have been mutated to determine the new phenotype. In order to create a
tumor necrosis factor (TNF) knockout, an exon containing the
nucleotides 3704–5364 was removed from the gene. This exon encodes a
portion of the mature TNF domain, as well as the leader sequence, which
is a highly conserved region necessary for proper intracellular
processing. TNF-/- mice develop normally and have no gross structural
or morphological abnormalities. However, upon immunization with SRBC
(sheep red blood cells), these mice demonstrated a deficiency in the
maturation of an antibody response; they were able to generate normal
levels of IgM, but could not develop specific IgG levels. Apaf-1 is the
protein that turns on caspase 9 by cleavage to begin the caspase
cascade that leads to apoptosis. Since a -/- mutation in the APAF-1
gene is embryonic lethal, a gene trap strategy was used in order to
generate an APAF-1 -/- mouse. This assay is used to disrupt gene
function by creating an intragenic gene fusion. When an APAF-1 gene
trap is introduced into cells, many morphological changes occur, such as
spina bifida, the persistence of interdigital webs, and open brain. In
addition, after embryonic day 12.5, the brain of the embryos showed
several structural changes. APAF-1 cells are protected from apoptosis
stimuli such as irradiation. A BAX-1 knock-out mouse exhibits normal
forebrain formation and a decreased programmed cell death in some
neuronal populations and in the spinal cord, leading to an increase in
motor neurons.
The caspase proteins are integral parts of the apoptosis pathway,
so it follows that knock-outs made have varying damaging results. A
caspase 9 knock-out leads to a severe brain malformation. A caspase 8
knock-out leads to cardiac failure and thus embryonic lethality.
However, with the use of cre-lox technology, a caspase 8 knock-out has
been created that exhibits an increase in peripheral T cells, an
impaired T cell response, and a defect in neural tube closure. These
mice were found to be resistant to apoptosis mediated by CD95, TNFR,
etc. but not resistant to apoptosis caused by UV irradiation,
chemotherapeutic drugs, and other stimuli. Finally, a caspase 3
knock-out was characterized by ectopic cell masses in the brain and
abnormal apoptotic features such as membrane blebbing or nuclear
fragmentation. A remarkable feature of these KO mice is that they have a
very restricted phenotype: Casp3, 9, APAF-1 KO mice have deformations
of neural tissue and FADD and Casp 8 KO showed defective heart
development, however, in both types of KO other organs developed
normally and some cell types were still sensitive to apoptotic stimuli
suggesting that unknown proapoptotic pathways exist.
Methods for distinguishing apoptotic from necrotic (necroptotic) cells
Long-term
live cell imaging (12h) of multinucleated mouse pre-Adipocyte trying to
undergo mitosis. Due to the excess of genetic material the cell fails
to replicate and dies by apoptosis.
In order to perform analysis of apoptotic versus necrotic (necroptotic) cells, one can do analysis of morphology by label-free live cell imaging, time-lapse microscopy, flow fluorocytometry, and transmission electron microscopy.
There are also various biochemical techniques for analysis of cell
surface markers (phosphatidylserine exposure versus cell permeability by
flow cytometry), cellular markers such as DNA fragmentation (flow cytometry), caspase activation, Bid cleavage, and cytochrome c release (Western blotting). It is important to know how primary and secondary necrotic cells can be distinguished by analysis of supernatant
for caspases, HMGB1, and release of cytokeratin 18. However, no
distinct surface or biochemical markers of necrotic cell death have been
identified yet, and only negative markers are available. These include
absence of apoptotic markers (caspase activation, cytochrome c release,
and oligonucleosomal DNA fragmentation) and differential kinetics of
cell death markers (phosphatidylserine exposure and cell membrane
permeabilization). A selection of techniques that can be used to
distinguish apoptosis from necroptotic cells could be found in these
references.
Implication in disease
A section of mouse liver showing several apoptotic cells, indicated by arrows
A section of mouse liver
stained to show cells undergoing apoptosis (orange)
Neonatal cardiomyocytes ultrastructure after anoxia-reoxygenation.
Defective pathways
The
many different types of apoptotic pathways contain a multitude of
different biochemical components, many of them not yet understood.
As a pathway is more or less sequential in nature, removing or
modifying one component leads to an effect in another. In a living
organism, this can have disastrous effects, often in the form of disease
or disorder. A discussion of every disease caused by modification of
the various apoptotic pathways would be impractical, but the concept
overlying each one is the same: The normal functioning of the pathway
has been disrupted in such a way as to impair the ability of the cell to
undergo normal apoptosis. This results in a cell that lives past its
"use-by date" and is able to replicate and pass on any faulty machinery
to its progeny, increasing the likelihood of the cell's becoming
cancerous or diseased.
A recently described example of this concept in action can be seen in the development of a lung cancer called NCI-H460. The X-linked inhibitor of apoptosis protein (XIAP) is overexpressed in cells of the H460 cell line. XIAPs bind to the processed form of caspase-9, and suppress the activity of apoptotic activator cytochrome c,
therefore overexpression leads to a decrease in the amount of
proapoptotic agonists. As a consequence, the balance of anti-apoptotic
and proapoptotic effectors is upset in favour of the former, and the
damaged cells continue to replicate despite being directed to die.
Defects in regulation of apoptosis in cancer cells occur often at the
level of control of transcription factors. As a particular example,
defects in molecules that control transcription factor NF-κB in cancer
change the mode of transcriptional regulation and the response to
apoptotic signals, to curtail dependence on the tissue that the cell
belongs. This degree of independence from external survival signals, can
enable cancer metastasis.
Dysregulation of p53
The tumor-suppressor protein p53 accumulates when DNA is damaged due to a chain of biochemical factors. Part of this pathway includes alpha-interferon and beta-interferon, which induce transcription of the p53 gene, resulting in the increase of p53 protein level and enhancement of cancer cell-apoptosis. p53 prevents the cell from replicating by stopping the cell cycle
at G1, or interphase, to give the cell time to repair, however it will
induce apoptosis if damage is extensive and repair efforts fail. Any disruption to the regulation of the p53 or interferon genes will result in impaired apoptosis and the possible formation of tumors.
Inhibition
Inhibition
of apoptosis can result in a number of cancers, inflammatory diseases,
and viral infections. It was originally believed that the associated
accumulation of cells was due to an increase in cellular proliferation,
but it is now known that it is also due to a decrease in cell death. The
most common of these diseases is cancer, the disease of excessive
cellular proliferation, which is often characterized by an
overexpression of IAP
family members. As a result, the malignant cells experience an abnormal
response to apoptosis induction: Cycle-regulating genes (such as p53,
ras or c-myc) are mutated or inactivated in diseased cells, and further
genes (such as bcl-2) also modify their expression in tumors. Some
apoptotic factors are vital during mitochondrial respiration e.g.
cytochrome C.
Pathological inactivation of apoptosis in cancer cells is correlated
with frequent respiratory metabolic shifts toward glycolysis (an
observation known as the “Warburg hypothesis”.
HeLa cell
Apoptosis in HeLa
cells is inhibited by proteins produced by the cell; these inhibitory
proteins target retinoblastoma tumor-suppressing proteins. These tumor-suppressing proteins regulate the cell cycle, but are rendered inactive when bound to an inhibitory protein.
HPV E6 and E7 are inhibitory proteins expressed by the human
papillomavirus, HPV being responsible for the formation of the cervical
tumor from which HeLa cells are derived. HPV E6 causes p53, which regulates the cell cycle, to become inactive. HPV E7 binds to retinoblastoma tumor suppressing proteins and limits its ability to control cell division. These two inhibitory proteins are partially responsible for HeLa cells' immortality by inhibiting apoptosis to occur.
CDV (Canine Distemper Virus) is able to induce apoptosis despite the
presence of these inhibitory proteins. This is an important oncolytic
property of CDV: this virus is capable of killing canine lymphoma
cells. Oncoproteins E6 and E7 still leave p53 inactive, but they are not
able to avoid the activation of caspases induced from the stress of
viral infection. These oncolytic properties provided a promising link
between CDV and lymphoma apoptosis, which can lead to development of
alternative treatment methods for both canine lymphoma
and human non-Hodgkin lymphoma. Defects in the cell cycle are thought
to be responsible for the resistance to chemotherapy or radiation by
certain tumor cells, so a virus that can induce apoptosis despite
defects in the cell cycle is useful for cancer treatment.
Treatments
The
main method of treatment for potential death from signaling-related
diseases involves either increasing or decreasing the susceptibility of
apoptosis in diseased cells, depending on whether the disease is caused
by either the inhibition of or excess apoptosis. For instance,
treatments aim to restore apoptosis to treat diseases with deficient
cell death, and to increase the apoptotic threshold to treat diseases
involved with excessive cell death. To stimulate apoptosis, one can
increase the number of death receptor ligands (such as TNF or TRAIL),
antagonize the anti-apoptotic Bcl-2 pathway, or introduce Smac mimetics
to inhibit the inhibitor (IAPs).
The addition of agents such as Herceptin, Iressa, or Gleevec works to
stop cells from cycling and causes apoptosis activation by blocking
growth and survival signaling further upstream. Finally, adding p53-MDM2
complexes displaces p53 and activates the p53 pathway, leading to cell
cycle arrest and apoptosis. Many different methods can be used either to
stimulate or to inhibit apoptosis in various places along the death
signaling pathway.
Apoptosis is a multi-step, multi-pathway cell-death programme
that is inherent in every cell of the body. In cancer, the apoptosis
cell-division ratio is altered. Cancer treatment by chemotherapy and
irradiation kills target cells primarily by inducing apoptosis.
Hyperactive apoptosis
On
the other hand, loss of control of cell death (resulting in excess
apoptosis) can lead to neurodegenerative diseases, hematologic diseases,
and tissue damage. It is of interest to note that neurons that rely on
mitochondrial respiration undergo apoptosis in neurodegenerative
diseases such as Alzheimer's and Parkinson's. (an observation known as the “Inverse Warburg hypothesis”). Moreover, there is an inverse epidemiological comorbidity between neurodegenerative diseases and cancer.
The progression of HIV is directly linked to excess, unregulated
apoptosis. In a healthy individual, the number of CD4+ lymphocytes is
in balance with the cells generated by the bone marrow; however, in
HIV-positive patients, this balance is lost due to an inability of the
bone marrow to regenerate CD4+ cells. In the case of HIV, CD4+
lymphocytes die at an accelerated rate through uncontrolled apoptosis,
when stimulated.
At the molecular level, hyperactive apoptosis can be caused by defects
in signaling pathways that regulate the Bcl-2 family proteins. Increased
expression of apoptotic proteins such as BIM, or their decreased
proteolysis, leads to cell death, and can cause a number of pathologies,
depending on the cells where excessive activity of BIM occurs. Cancer
cells can escape apoptosis through mechanisms that suppress BIM
expression or by increased proteolysis of BIM.
Treatments
Treatments
aiming to inhibit works to block specific caspases. Finally, the Akt
protein kinase promotes cell survival through two pathways. Akt
phosphorylates and inhibits Bad (a Bcl-2 family member), causing Bad to
interact with the 14-3-3
scaffold, resulting in Bcl dissociation and thus cell survival. Akt
also activates IKKα, which leads to NF-κB activation and cell survival.
Active NF-κB induces the expression of anti-apoptotic genes such as
Bcl-2, resulting in inhibition of apoptosis. NF-κB has been found to
play both an antiapoptotic role and a proapoptotic role depending on the
stimuli utilized and the cell type.
HIV progression
The progression of the human immunodeficiency virus infection into AIDS is due primarily to the depletion of CD4+ T-helper lymphocytes
in a manner that is too rapid for the body's bone marrow to replenish
the cells, leading to a compromised immune system. One of the mechanisms
by which T-helper cells are depleted is apoptosis, which results from a
series of biochemical pathways:
- HIV enzymes deactivate anti-apoptotic Bcl-2. This does
not directly cause cell death but primes the cell for apoptosis should
the appropriate signal be received. In parallel, these enzymes activate
proapoptotic procaspase-8, which does directly activate the mitochondrial events of apoptosis.
- HIV may increase the level of cellular proteins that prompt Fas-mediated apoptosis.
- HIV proteins decrease the amount of CD4 glycoprotein marker present on the cell membrane.
- Released viral particles and proteins present in extracellular fluid
are able to induce apoptosis in nearby "bystander" T helper cells.
- HIV decreases the production of molecules involved in marking the
cell for apoptosis, giving the virus time to replicate and continue
releasing apoptotic agents and virions into the surrounding tissue.
- The infected CD4+ cell may also receive the death signal from a cytotoxic T cell.
Cells may also die as direct consequences of viral infections. HIV-1 expression induces tubular cell G2/M arrest and apoptosis.
The progression from HIV to AIDS is not immediate or even necessarily
rapid; HIV's cytotoxic activity toward CD4+ lymphocytes is classified as
AIDS once a given patient's CD4+ cell count falls below 200.
Researchers from Kumamoto University in Japan have developed a
new method to eradicate HIV in viral reservoir cells, named "Lock-in and
apoptosis." Using the synthesized compound Heptanoylphosphatidyl
L-Inositol Pentakisphophate (or L-Hippo) to bind strongly to the HIV
protein PR55Gag, they were able to suppress viral budding. By
suppressing viral budding, the researchers were able to trap the HIV
virus in the cell and allow for the cell to undergo apoptosis (natural
cell death). Associate Professor Mikako Fujita has stated that the
approach is not yet available to HIV patients because the research team
has to conduct further research on combining the drug therapy that
currently exists with this "Lock-in and apoptosis" approach to lead to
complete recovery from HIV.
Viral infection
Viral induction of apoptosis occurs when one or several cells of a living organism are infected with a virus, leading to cell death. Cell death in organisms is necessary for the normal development of cells and the cell cycle maturation. It is also important in maintaining the regular functions and activities of cells.
Viruses can trigger apoptosis of infected cells via a range of mechanisms including:
- Receptor binding
- Activation of protein kinase R (PKR)
- Interaction with p53
- Expression of viral proteins coupled to MHC proteins on the surface
of the infected cell, allowing recognition by cells of the immune system
(such as Natural Killer and cytotoxic T cells) that then induce the infected cell to undergo apoptosis.
Canine distemper virus (CDV) is known to cause apoptosis in central nervous system and lymphoid tissue of infected dogs in vivo and in vitro.
Apoptosis caused by CDV is typically induced via the extrinsic pathway, which activates caspases that disrupt cellular function and eventually leads to the cells death.
In normal cells, CDV activates caspase-8 first, which works as the
initiator protein followed by the executioner protein caspase-3.
However, apoptosis induced by CDV in HeLa cells does not involve the
initiator protein caspase-8. HeLa cell apoptosis caused by CDV follows a
different mechanism than that in vero cell lines. This change in the caspase cascade suggests CDV induces apoptosis via the intrinsic pathway,
excluding the need for the initiator caspase-8. The executioner protein
is instead activated by the internal stimuli caused by viral infection
not a caspase cascade.
The Oropouche virus (OROV) is found in the family Bunyaviridae. The study of apoptosis brought on by Bunyaviridae
was initiated in 1996, when it was observed that apoptosis was induced
by the La Crosse virus into the kidney cells of baby hamsters and into
the brains of baby mice.
OROV is a disease that is transmitted between humans by the biting midge (Culicoides paraensis). It is referred to as a zoonotic arbovirus and causes febrile illness, characterized by the onset of a sudden fever known as Oropouche fever.
The Oropouche virus also causes disruption in cultured cells –
cells that are cultivated in distinct and specific conditions. An
example of this can be seen in HeLa cells, whereby the cells begin to degenerate shortly after they are infected.
With the use of gel electrophoresis, it can be observed that OROV causes DNA
fragmentation in HeLa cells. It can be interpreted by counting,
measuring, and analyzing the cells of the Sub/G1 cell population. When HeLA cells are infected with OROV, the cytochrome C
is released from the membrane of the mitochondria, into the cytosol of
the cells. This type of interaction shows that apoptosis is activated
via an intrinsic pathway.
In order for apoptosis to occur within OROV, viral uncoating,
viral internalization, along with the replication of cells is necessary.
Apoptosis in some viruses is activated by extracellular stimuli.
However, studies have demonstrated that the OROV infection causes
apoptosis to be activated through intracellular stimuli and involves the
mitochondria.
Many viruses encode proteins that can inhibit apoptosis.
Several viruses encode viral homologs of Bcl-2. These homologs can
inhibit proapoptotic proteins such as BAX and BAK, which are essential
for the activation of apoptosis. Examples of viral Bcl-2 proteins
include the Epstein-Barr virus BHRF1 protein and the adenovirus E1B 19K protein.
Some viruses express caspase inhibitors that inhibit caspase activity
and an example is the CrmA protein of cowpox viruses. Whilst a number of
viruses can block the effects of TNF and Fas. For example, the M-T2
protein of myxoma viruses can bind TNF preventing it from binding the
TNF receptor and inducing a response.
Furthermore, many viruses express p53 inhibitors that can bind p53 and
inhibit its transcriptional transactivation activity. As a consequence,
p53 cannot induce apoptosis, since it cannot induce the expression of
proapoptotic proteins. The adenovirus E1B-55K protein and the hepatitis B virus HBx protein are examples of viral proteins that can perform such a function.
Viruses can remain intact from apoptosis in particular in the latter stages of infection. They can be exported in the apoptotic bodies
that pinch off from the surface of the dying cell, and the fact that
they are engulfed by phagocytes prevents the initiation of a host
response. This favours the spread of the virus.
Plants
Programmed cell death
in plants has a number of molecular similarities to that of animal
apoptosis, but it also has differences, notable ones being the presence
of a cell wall and the lack of an immune system
that removes the pieces of the dead cell. Instead of an immune
response, the dying cell synthesizes substances to break itself down and
places them in a vacuole
that ruptures as the cell dies. Whether this whole process resembles
animal apoptosis closely enough to warrant using the name apoptosis (as opposed to the more general programmed cell death) is unclear.
Caspase-independent apoptosis
The
characterization of the caspases allowed the development of caspase
inhibitors, which can be used to determine whether a cellular process
involves active caspases. Using these inhibitors it was discovered that
cells can die while displaying a morphology similar to apoptosis without
caspase activation. Later studies linked this phenomenon to the release of AIF (
apoptosis-inducing factor)
from the mitochondria and its translocation into the nucleus mediated
by its NLS (nuclear localization signal). Inside the mitochondria, AIF
is anchored to the inner membrane. In order to be released, the protein
is cleaved by a calcium-dependent
calpain protease.