| Locus coeruleus | |
|---|---|
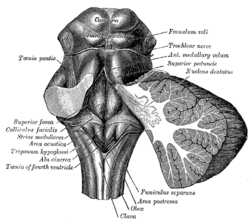
Rhomboid fossa. (Locus coeruleus not labeled, but is very near [just lateral to] the facial colliculus, which is labeled at center left.)
| |

Micrograph showing the locus coeruleus. HE-LFB stain.
| |
| Details | |
| Identifiers | |
| Latin | locus caeruleus ("blue place") |
| MeSH | D008125 |
| NeuroNames | 583 |
| NeuroLex ID | birnlex_905 |
| TA | A14.1.05.436 A14.1.05.706 |
| FMA | 72478 |
The locus coeruleus (\-si-ˈrü-lē-əs\, also spelled locus caeruleus or locus ceruleus) is a nucleus in the pons of the brainstem involved with physiological responses to stress and panic. It is a part of the reticular activating system.
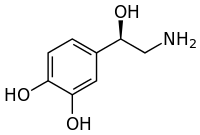
The locus coeruleus is the principal site for brain synthesis of norepinephrine (noradrenaline). The locus coeruleus and the areas of the body affected by the norepinephrine it produces are described collectively as the locus coeruleus-noradrenergic system or LC-NA system. Norepinephrine may also be released directly into the blood from the adrenal medulla.
Anatomy
Micrograph showing the locus coeruleus (upper-right of image) in an axial section of the pons. The fourth ventricle
(quasi-triangular white area) is in the upper-left of the image. The
midline is seen on the left. The large white area in the upper-left
corner is where the cerebellum would be. HE-LFB stain.
The locus coeruleus (LC) is located in the posterior area of the rostral pons in the lateral floor of the fourth ventricle. It is composed of mostly medium-size neurons. Melanin
granules inside the neurons of the LC contribute to its blue colour.
Thus, it is also known as the nucleus pigmentosus pontis, meaning
"heavily pigmented nucleus of the pons." The neuromelanin is formed by the polymerization of noradrenaline and is analogous to the black dopamine-based neuromelanin in the substantia nigra.
In adult humans (19-78) the locus coeruleus has 22,000 to 51,000
total pigmented neurons that range in size between 31,000 and 60,000 μm3.
Connections
The projections of this nucleus reach far and wide. For example, they innervate the spinal cord, the brain stem, cerebellum, hypothalamus, the thalamic relay nuclei, the amygdala, the basal telencephalon, and the cortex. The norepinephrine from the LC has an excitatory effect on most of the brain, mediating arousal and priming the brain’s neurons to be activated by stimuli.
As an important homeostatic control center of the body, the locus coeruleus receives afferents from the hypothalamus. The cingulate gyrus
and the amygdala also innervate the LC, allowing emotional pain and
stressors to trigger noradrenergic responses. The cerebellum and
afferents from the raphe nuclei also project to the LC, in particular the pontine raphe nucleus and dorsal raphe nucleus.
Inputs
The locus coeruleus receives inputs from a number of other brain regions, primarily:
- Medial prefrontal cortex, whose connection is constant, excitatory, and increases in strength with raised activity levels in the subject
- Nucleus paragigantocellularis, which integrates autonomic and environmental stimuli
- Nucleus prepositus, which is involved in gaze
- Lateral hypothalamus, which releases orexin, which, as well as its other functions, is excitatory in the locus coeruleus.
Outputs
The projections from the locus coeruleus consist of neurons that utilize norepinephrine as their primary neurotransmitter. These projections include the following connections:
- LC → Amygdala & Hippocampus
- LC → Brain stem & Spinal cord
- LC → Cerebellum
- LC → Cerebral cortex
- LC → Hypothalamus
- LC → Tectum
- LC → Thalamus
- LC → Ventral tegmental area
Function
It is
related to many functions via its widespread projections. The LC-NA
system modulates cortical, subcortical, cerebellar, brainstem, and
spinal cord circuits. Some of the most important functions influenced by
this system are:
- Arousal and sleep-wake cycle
- Attention and memory
- Behavioral flexibility, behavioral inhibition and stress (psychological)
- Cognitive control
- Emotions
- Neuroplasticity
- Posture and balance
The locus coeruleus is a part of the reticular activating system, and is almost completely inactivated in rapid eye movement sleep.
Pathophysiology
The locus coeruleus may figure in clinical depression, panic disorder, Parkinson's disease, Alzheimer's disease and anxiety. Some medications including norepinephrine reuptake inhibitors (reboxetine, atomoxetine), serotonin-norepinephrine reuptake inhibitors (venlafaxine, duloxetine), and norepinephrine-dopamine reuptake inhibitors (bupropion) are believed to show efficacy by acting upon neurons in this area.
Research continues to reveal that norepinephrine (NE) is a
critical regulator of numerous activities from stress response, the
formation of memory to attention and arousal. Many neuropsychiatric
disorders precipitate from alterations to NE modulated neurocircuitry:
disorders of affect, anxiety disorders, PTSD, ADHD and Alzheimer’s
disease. Alterations in the locus coeruleus (LC) accompany
dysregulation of NE function and likely play a key role in the
pathophysiology of these neuropsychiatric disorders.
In stress
The
locus coeruleus is responsible for mediating many of the sympathetic
effects during stress. The locus coeruleus is activated by stress, and
will respond by increasing norepinephrine secretion, which in turn will
alter cognitive function (through the prefrontal cortex), increase
motivation (through nucleus accumbens), activate the hypothalamic-pituitary-adrenal axis, and increase the sympathetic discharge/inhibit parasympathetic tone (through the brainstem). Specific to the activation of the hypothalamo-pituitary adrenal axis, norepinephrine will stimulate the secretion of corticotropin-releasing factor from the hypothalamus, that induces adrenocorticotropic hormone release from the anterior pituitary and subsequent cortisol synthesis in the adrenal glands.
Norepinephrine released from locus coeruleus will feedback to inhibit
its production, and corticotropin-releasing hormone will feedback to
inhibit its production, while positively feeding to the locus coeruleus
to increase norepinephrine production.
The LC's role in cognitive function in relation to stress is
complex and multi-modal. Norepinephrine released from the LC can act on
α2 receptors to increase working memory, or an excess of NE may decrease
working memory by binding to the lower-affinity α1 receptors.
Psychiatric research has documented that enhanced noradrenergic
postsynaptic responsiveness in the neuronal pathway (brain circuit) that
originates in the locus coeruleus and ends in the basolateral nucleus
of the amygdala is a major factor in the pathophysiology of most
stress-induced fear-circuitry disorders and especially in posttraumatic stress disorder
(PTSD). The LC neurons are probably the origin of the first or second
“leg” of the "PTSD circuit." An important 2005 study of deceased
American army veterans from World War II has shown combat-related PTSD
to be associated with a postmortem-diminished number of neurons in the
locus coeruleus (LC) on the right side of the brain.
In opiate withdrawal
Opioids
inhibit the firing of neurons in the locus coeruleus. When opioid
consumption is stopped, the increased activity of the locus coeruleus
contributes to the symptoms of opiate withdrawal. The alpha2
adrenoceptor agonist clonidine is used to counteract this withdrawal effect by decreasing adrenergic neurotransmission from the locus coeruleus.
Rett syndrome
The genetic defect of the transcriptional regulator MECP2 is responsible for Rett syndrome.
A MECP2 deficiency has been associated to catecholaminergic
dysfunctions related to autonomic and sympathoadrenergic system in mouse
models of Rett Syndrome (RTT). The Locus Coeruleus is the major source
of noradrenergic innervation in the brain and sends widespread
connections to rostral (cerebral cortex, hippocampus, hypothalamus) and
caudal (cerebellum, brainstem nuclei) brain areas. Indeed, an alteration of this structure could contribute to several
symptoms observed in MECP2-deficient mice. Changes in the
electrophysiological properties of cells in the locus ceruleus
were shown. These Locus Coeruleus cell changes include
hyperexcitability and decreased functioning of its noradrenergic
innervation.
A reduction of the tyrosine hydroxylase (TH) mRNA level, the
rate-limiting enzyme in catecholamine synthesis, was detected in the
whole pons of MECP2-null male as well as in adult heterozygous female
mice. Using immunoquantification techniques, a decrease of TH protein
staining level, number of locus coeruleus TH-expressing neurons and
density of dendritic arborization surrounding the structure was shown in
symptomatic MECP2-deficient mice.
However, locus coeruleus cells are not dying but are more likely losing
their fully mature phenotype, since no apoptotic neurons in the pons
were detected.
Researchers have concluded that, "Because these neurons are a pivotal
source of norepinephrine throughout the brainstem and forebrain and are
involved in the regulation of diverse functions disrupted in Rett
Syndrome, such as respiration and cognition, we hypothesize that the
locus ceruleus is a critical site at which loss of MECP2 results in CNS
dysfunction. Restoration of normal locus ceruleus function may therefore
be of potential therapeutic value in the treatment of Rett Syndrome."
This could explain why a norepinephrine reuptake inhibitor
(desipramine, DMI), which enhances the extracellular NE levels at all
noradrenergic synapses, ameliorated some Rett syndrome symptoms in a
mouse model of Rett syndrome.
Neurodegenerative diseases
The locus ceruleus is affected in many forms of neurodegenerative diseases: genetic and idiopathic Parkinson's disease, progressive supranuclear palsy, Pick's disease or Alzheimer's disease. It is also affected in Down syndrome. For example, there is up to 80% loss of locus ceruleus neurons in Alzheimer's disease. Mouse models of Alzheimer's disease show accelerated progression after chemical destruction of the locus ceruleus
The norepinephrine from locus ceruleus cells in addition to its
neurotransmitter role locally diffuses from "varicosities". As such it
provides an endogenous anti-inflammatory agent in the microenvironment around the neurons, glial cells, and blood vessels in the neocortex and hippocampus. It has been shown that norepinephrine stimulates mouse microglia to suppress Aβ-induced production of cytokines and promotes phagocytosis of Aβ. This suggests that degeneration of the locus ceruleus might be responsible for increased Aβ deposition in AD brains.
Degeneration of pigmented neurons in this region in Alzheimer's and
Parkinson's disease can be visualized in vivo with Neuromelanin MRI.
History
It was discovered in 1784 by Félix Vicq-d'Azyr, redescribed later by Johann Christian Reil in 1809 and named by Joseph Wenzel and Karl Wenzel brothers in 1812. High monoamine oxidase activity in the rodent LC was found in 1959, monoamines were found in 1964 and noradrenergic ubiquitous projections in the 1970s.
Etymology
Coeruleus or caeruleus
The 'English' name locus coeruleus is actually a Latin expression consisting of the noun, locus, place or spot and the adjective coeruleus, dark blue or sky-blue. This was aptly translated into English as blue place in 1907 in the English translation of the official Latin anatomic nomenclature of 1895, Nomina Anatomica. The name of the locus coeruleus is derived from its azure appearance in unstained brain tissue. The color is due to light scattering from neuromelanin in noradrenergic (producing or activated by norepinephrine) nerve cell bodies.
The phenomenon is magnified by the Falck-Hillarp technique°, which
combines freeze-dried tissue and formaldehyde to fluoresce the
catecholamines and serotonin contained in the tissue.
The spelling coeruleus is actually considered incorrect with dictionaries of classical Latin preferring caeruleus instead. Caeruleus is derived from caelum, hence the spelling with -ae, like caeluleus → caeruleus. Caelum in classical Latin could refer to the sky, the heaven or the vault of heaven.
In mediaeval Latin, orthographic variants like coelum for classical Latin caelum and cerulans for classical Latin caerulans can be spotted.
In English, the color adjective cerulean is derived from Latin caeruleus. In addition, ceiling is ultimately derived from Latin caelum as well.
Official Latin nomenclature
The official Latin nomenclature, Nomina Anatomica as ratified in Basel in 1895 and in Jena in 1935 contained the orthographic correct form locus caeruleus. The Nomina Anatomica published in 1955 inadvertently introduced the incorrect spelling locus coeruleus, without any further explanation. The subsequent edition monophthongized the diphthong, resulting in locus ceruleus, as they proclaimed that: "All diphthongs should be eliminated". This form was retained in the subsequent edition. The following two editions from 1977
and 1983 reverted the orthography back to the incorrect spelling locus coeruleus, while the subsequent edition from 1989 eventually returned to the correct spelling locus caeruleus. The current edition of the Nomina Anatomica, rebaptized as Terminologia Anatomica, dictates locus caeruleus in its list of Latin expressions and correspondingly mentions locus caeruleus in its list of English equivalents. This is in line with the statement made by the chairman of the Terminologia Anatomica that "the committee decided that Latin terms when used in English should be in correct Latin".