From Wikipedia, the free encyclopedia
Clinical psychology is an integration of science, theory, and
clinical knowledge for the purpose of understanding, preventing, and
relieving psychologically-based distress or
dysfunction and to promote subjective
well-being and personal development. Central to its practice are
psychological assessment,
clinical formulation, and
psychotherapy,
although clinical psychologists also engage in research, teaching,
consultation, forensic testimony, and program development and
administration. In many countries, clinical psychology is a regulated
mental health profession.
The field is generally considered to have begun in 1896 with the opening of the first psychological
clinic at the
University of Pennsylvania by
Lightner Witmer.
In the first half of the 20th century, clinical psychology was focused
on psychological assessment, with little attention given to treatment.
This changed after the 1940s when World War II resulted in the need for a
large increase in the number of trained clinicians. Since that time,
three main educational models have developed in the USA—the Ph.D.
Clinical Science model (heavily focused on research), the
Ph.D. science-practitioner model (integrating research and practice), and the
Psy.D. practitioner-scholar model (focusing on clinical practice). In the UK and the Republic of Ireland, the
Clinical Psychology Doctorate
falls between the latter two of these models, whilst in much of
mainland Europe, the training is at the masters level and predominantly
psychotherapeutic. Clinical psychologists are expert in providing
psychotherapy, and generally train within four primary theoretical
orientations—
psychodynamic,
humanistic,
cognitive behavioral therapy (CBT), and
systems or family therapy.
History
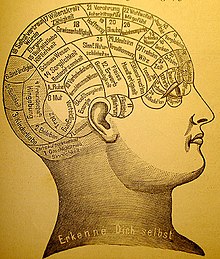
Many 18th c. treatments for psychological distress were based on pseudo-scientific ideas, such as Phrenology.
The earliest recorded approaches to assess and treat mental distress
were a combination of religious, magical and/or medical perspectives. Early examples of such physicians included
Patañjali,
Padmasambhava,
Rhazes,
Avicenna, and
Rumi. In the early 19th century, one approach to study mental conditions and behavior was using
phrenology,
the study of personality by examining the shape of the skull. Other
popular treatments at that time included the study of the shape of the
face (
physiognomy) and
Mesmer's treatment for mental conditions using magnets (
mesmerism).
Spiritualism and
Phineas Quimby's "mental healing" were also popular.
While the scientific community eventually came to reject all of
these methods for treating mental illness, academic psychologists also
were not concerned with serious forms of mental illness. The study of
mental illness was already being done in the developing fields of
psychiatry and
neurology within the
asylum movement. It was not until the end of the 19th century, around the time when
Sigmund Freud was first developing his "
talking cure" in
Vienna, that the first scientific application of clinical psychology began.
Early clinical psychology
Cover of The Psychological Clinic, the first journal of clinical psychology, published in 1907 by Lightner Witmer
By the second half of the 1800s, the scientific study of psychology
was becoming well established in university laboratories. Although there
were a few scattered voices calling for applied psychology, the general
field looked down upon this idea and insisted on "pure" science as the
only respectable practice.
[5] This changed when
Lightner Witmer (1867–1956), a past student of
Wundt and head of the psychology department at the
University of Pennsylvania,
agreed to treat a young boy who had trouble with spelling. His
successful treatment was soon to lead to Witmer's opening of the first
psychological clinic at Penn in 1896, dedicated to helping children with
learning disabilities. Ten years later in 1907, Witmer was to found the first journal of this new field,
The Psychological Clinic,
where he coined the term "clinical psychology", defined as "the study
of individuals, by observation or experimentation, with the intention of
promoting change". The field was slow to follow Witmer's example, but by 1914, there were 26 similar clinics in the U.S.
Even as clinical psychology was growing, working with issues of serious mental distress remained the domain of
psychiatrists and
neurologists. However, clinical psychologists continued to make inroads into this area due to their increasing skill at
psychological assessment. Psychologists' reputation as assessment experts became solidified during
World War I with the development of two intelligence tests,
Army Alpha and
Army Beta (testing verbal and nonverbal skills, respectively), which could be used with large groups of recruits.
Due in large part to the success of these tests, assessment was to
become the core discipline of clinical psychology for the next quarter
century, when another war would propel the field into treatment.
Early professional organizations
The
field began to organize under the name "clinical psychology" in 1917
with the founding of the American Association of Clinical Psychology.
This only lasted until 1919, after which the
American Psychological Association (founded by
G. Stanley Hall in 1892) developed a section on Clinical Psychology, which offered certification until 1927.
Growth in the field was slow for the next few years when various
unconnected psychological organizations came together as the American
Association of Applied Psychology in 1930, which would act as the
primary forum for psychologists until after World War II when the APA
reorganized.
In 1945, the APA created what is now called Division 12, its division
of clinical psychology, which remains a leading organization in the
field. Psychological societies and associations in other
English-speaking countries developed similar divisions, including in
Britain, Canada, Australia, and New Zealand.
World War II and the integration of treatment
When
World War II
broke out, the military once again called upon clinical psychologists.
As soldiers began to return from combat, psychologists started to notice
symptoms of psychological trauma labeled "shell shock" (eventually to
be termed
posttraumatic stress disorder) that were best treated as soon as possible.
Because physicians (including psychiatrists) were over-extended in
treating bodily injuries, psychologists were called to help treat this
condition.
At the same time, female psychologists (who were excluded from the war
effort) formed the National Council of Women Psychologists with the
purpose of helping communities deal with the stresses of war and giving
young mothers advice on child rearing. After the war, the
Veterans Administration
in the U.S. made an enormous investment to set up programs to train
doctoral-level clinical psychologists to help treat the thousands of
veterans needing care. As a consequence, the U.S. went from having no
formal university programs in clinical psychology in 1946 to over half
of all Ph.D.s in psychology in 1950 being awarded in clinical
psychology.
WWII helped bring dramatic changes to clinical psychology, not
just in America but internationally as well. Graduate education in
psychology began adding psychotherapy to the science and research focus
based on the 1947
scientist-practitioner model, known today as the
Boulder Model, for Ph.D. programs in clinical psychology. Clinical psychology in
Britain developed much like in the U.S. after WWII, specifically within the context of the
National Health Service with qualifications, standards, and salaries managed by the
British Psychological Society.
Development of the Doctor of Psychology degree
By
the 1960s, psychotherapy had become embedded within clinical
psychology, but for many, the Ph.D. educational model did not offer the
necessary training for those interested in practice rather than
research. There was a growing argument that said the field of psychology
in the U.S. had developed to a degree warranting explicit training in
clinical practice. The concept of a practice-oriented degree was debated
in 1965 and narrowly gained approval for a pilot program at the
University of Illinois starting in 1968. Several other similar programs were instituted soon after, and in 1973, at the
Vail Conference on Professional Training in Psychology, the
practitioner–scholar model of clinical psychology—or
Vail Model—resulting in the Doctor of Psychology (
Psy.D.) degree was recognized.
Although training would continue to include research skills and a
scientific understanding of psychology, the intent would be to produce
highly trained professionals, similar to programs in medicine,
dentistry, and law. The first program explicitly based on the Psy.D.
model was instituted at
Rutgers University. Today, about half of all American graduate students in clinical psychology are enrolled in Psy.D. programs.
A changing profession
Since
the 1970s, clinical psychology has continued growing into a robust
profession and academic field of study. Although the exact number of
practicing clinical psychologists is unknown, it is estimated that
between 1974 and 1990, the number in the U.S. grew from 20,000 to
63,000.
Clinical psychologists continue to be experts in assessment and
psychotherapy while expanding their focus to address issues of
gerontology, sports, and the criminal justice system to name a few. One
important field is
health psychology, the fastest-growing employment setting for clinical psychologists in the past decade. Other major changes include the impact of
managed care
on mental health care; an increasing realization of the importance of
knowledge relating to multicultural and diverse populations; and
emerging privileges to prescribe psychotropic medication.
Professional practice
Clinical psychologists engage in a wide range of activities. Some focus solely on
research into the
assessment,
treatment, or cause of
mental illness and related conditions. Some teach, whether in a
medical school or
hospital setting, or in an academic department (e.g., psychology department) at an
institution of higher education.
The majority of clinical psychologists engage in some form of clinical
practice, with professional services including psychological assessment,
provision of psychotherapy, development and administration of clinical
programs, and
forensics (e.g., providing expert testimony in a
legal proceeding).
In clinical practice, clinical psychologists may work with
individuals, couples, families, or groups in a variety of settings,
including private practices, hospitals, mental health organizations,
schools, businesses, and non-profit agencies. Clinical psychologists who
provide clinical services may also choose to specialize. Some
specializations are codified and credentialed by regulatory agencies
within the country of practice. In the United States such specializations are credentialed by the
American Board of Professional Psychology (ABPP).
Training and certification to practice
Clinical
psychologists study a generalist program in psychology plus
postgraduate training and/or clinical placement and supervision. The
length of training differs across the world, ranging from four years
plus post-Bachelors supervised practice to a doctorate of three to six years which combines clinical placement. In the USA, about half of all clinical psychology graduate students are being trained in
Ph.D. programs—a model that emphasizes research—with the other half in
Psy.D. programs, which has more focus on practice (similar to professional degrees for medicine and law). Both models are accredited by the
American Psychological Association
and many other English-speaking psychological societies. A smaller
number of schools offer accredited programs in clinical psychology
resulting in a
Masters degree, which usually take two to three years post-Bachelors.
In the U.K., clinical psychologists undertake a Doctor of Clinical Psychology (D.Clin.Psych.), which is a practitioner
doctorate with both clinical and research components. This is a three-year full-time salaried program sponsored by the
National Health Service
(NHS) and based in universities and the NHS. Entry into these programs
is highly competitive and requires at least a three-year undergraduate
degree in psychology plus some form of experience, usually in either the
NHS as an Assistant Psychologist or in academia as a Research
Assistant. It is not unusual for applicants to apply several times
before being accepted onto a training course as only about one-fifth of
applicants are accepted each year. These clinical psychology doctoral degrees are accredited by the
British Psychological Society and the Health Professions Council (
HPC). The
HPC
is the statutory regulator for practitioner psychologists in the UK.
Those who successfully complete clinical psychology doctoral degrees are
eligible to apply for registration with the HPC as a clinical
psychologist.
The practice of clinical psychology requires a license in the
United States, Canada, the United Kingdom, and many other countries.
Although each of the U.S. states is somewhat different in terms of
requirements and licenses, there are three common elements:
- Graduation from an accredited school with the appropriate degree
- Completion of supervised clinical experience or internship
- Passing a written examination and, in some states, an oral examination
All U.S. state and Canadian province licensing boards are members of
the Association of State and Provincial Psychology Boards (ASPPB) which
created and maintains the Examination for Professional Practice in
Psychology (EPPP). Many states require other examinations in addition to
the EPPP, such as a jurisprudence (i.e. mental health law) examination
and/or an oral examination.
Most states also require a certain number of continuing education
credits per year in order to renew a license, which can be obtained
through various means, such as taking audited classes and attending
approved workshops. Clinical psychologists require the Psychologist
license to practice, although licenses can be obtained with a
masters-level degree, such as Marriage and Family Therapist (MFT),
Licensed Professional Counselor (LPC), and Licensed Psychological Associate (LPA).
In the U.K. registration as a clinical psychologist with the Health Professions Council
(HPC) is necessary. The
HPC
is the statutory regulator for practitioner psychologists in the U.K.
In the U.K. the following titles are restricted by law "registered
psychologist" and "practitioner psychologist"; in addition, the
specialist title "clinical psychologist" is also restricted by law.
Assessment
An important area of expertise for many clinical psychologists is
psychological assessment, and there are indications that as many as 91% of
psychologists engage in this core clinical practice. Such evaluation is usually done in service to gaining insight into and forming
hypotheses
about psychological or behavioral problems. As such, the results of
such assessments are usually used to create generalized impressions
(rather than
diagnoses)
in service to informing treatment planning. Methods include formal
testing measures, interviews, reviewing past records, clinical
observation, and physical examination.
Measurement domains
There exist hundreds of various assessment tools, although only a few have been shown to have both high
validity (i.e., test actually measures what it claims to measure) and
reliability (i.e., consistency). These measures generally fall within one of several categories, including the following:
- Intelligence & achievement tests – These tests are designed to measure certain specific kinds of cognitive functioning (often referred to as IQ) in comparison to a norming group. These tests, such as the WISC-IV,
attempt to measure such traits as general knowledge, verbal skill,
memory, attention span, logical reasoning, and visual/spatial
perception. Several tests have been shown to predict accurately certain
kinds of performance, especially scholastic.
- Personality tests – Tests of personality aim to describe patterns of behavior, thoughts, and feelings. They generally fall within two categories: objective and projective. Objective measures, such as the MMPI,
are based on restricted answers—such as yes/no, true/false, or a rating
scale—which allow for the computation of scores that can be compared to
a normative group. Projective tests, such as the Rorschach inkblot test, allow for open-ended answers, often based on ambiguous stimuli.
- Neuropsychological tests – Neuropsychological tests consist of specifically designed tasks used to measure psychological functions known to be linked to a particular brain structure or pathway. They are typically used to assess impairment after an injury or illness known to affect neurocognitive functioning, or when used in research, to contrast neuropsychological abilities across experimental groups.
- Clinical observation – Clinical psychologists are also
trained to gather data by observing behavior. The clinical interview is a
vital part of the assessment, even when using other formalized tools,
which can employ either a structured or unstructured format. Such
assessment looks at certain areas, such as general appearance and
behavior, mood and affects, perception, comprehension, orientation,
insight, memory, and content of the communication. One psychiatric
example of a formal interview is the mental status examination, which is often used in psychiatry as a screening tool for treatment or further testing.
Diagnostic impressions
Several new models are being discussed, including a "dimensional
model" based on empirically validated models of human differences (such
as the
five factor model of personality) and a "psychosocial model", which would take changing, intersubjective states into greater account.
The proponents of these models claim that they would offer greater
diagnostic flexibility and clinical utility without depending on the
medical concept of illness.
However, they also admit that these models are not yet robust enough to
gain widespread use, and should continue to be developed.
Clinical psychologists do not tend to diagnose, but rather use
formulation—an
individualized map of the difficulties that the patient or client
faces, encompassing predisposing, precipitating and perpetuating
(maintaining) factors.
Clinical v. mechanical prediction
Clinical assessment can be characterized as a
prediction problem where the purpose of assessment is to make inferences (predictions) about past, present, or future behavior. For example, many
therapy decisions are made on the basis of what a
clinician expects will help a patient make therapeutic gains. Once observations have been collected (e.g.,
psychological test results, diagnostic impressions, clinical history,
X-ray, etc.), there are two mutually exclusive ways to combine those sources of information to arrive at a decision,
diagnosis, or prediction. One way is to combine the data in an
algorithmic,
or "mechanical" fashion. Mechanical prediction methods are simply a
mode of combination of data to arrive at a decision/prediction of
behavior (e.g.,
treatment response).
The mechanical prediction does not preclude any type of data from being
combined; it can incorporate clinical judgments, properly coded, in the
algorithm.
The defining characteristic is that, once the data to be combined is
given, the mechanical approach will make a prediction that is 100%
reliable.
That is, it will make exactly the same prediction for exactly the same
data every time. Clinical prediction, on the other hand, does not
guarantee this, as it depends on the
decision-making processes of the clinician making the judgment, their current state of mind, and knowledge base.
What has come to be called the "clinical versus statistical prediction" debate was first described in detail in 1954 by
Paul Meehl,
where he explored the claim that mechanical (formal, algorithmic)
methods of data combination could outperform clinical (e.g., subjective,
informal, "in the clinician's head") methods when such combinations are
used to arrive at a prediction of behavior. Meehl concluded that
mechanical modes of combination performed as well or better than
clinical modes. Subsequent
meta-analyses of studies that directly compare mechanical and clinical predictions have born out Meehl's 1954 conclusions. A 2009 survey of practicing
clinical psychologists found that clinicians almost exclusively use their clinical judgment to make behavioral predictions for their
patients, including
diagnosis and
prognosis.
Intervention
Psychotherapy involves a formal relationship between professional and
client—usually an individual, couple, family, or small group—that
employs a set of procedures intended to form a therapeutic alliance,
explore the nature of psychological problems, and encourage new ways of
thinking, feeling, or behaving.
Clinicians have a wide range of individual interventions to draw
from, often guided by their training—for example, a cognitive behavioral
therapy (
CBT) clinician might use worksheets to record distressing cognitions, a
psychoanalyst might encourage
free association, while a psychologist trained in
Gestalt
techniques might focus on immediate interactions between client and
therapist. Clinical psychologists generally seek to base their work on
research evidence and outcome studies as well as on trained clinical
judgment. Although there are literally dozens of recognized therapeutic
orientations, their differences can often be categorized on two
dimensions: insight vs. action and in-session vs. out-session.
- Insight – emphasis is on gaining a greater understanding of the
motivations underlying one's thoughts and feelings (e.g. psychodynamic
therapy)
- Action – focus is on making changes in how one thinks and acts (e.g. solution focused therapy, cognitive behavioral therapy)
- In-session – interventions center on the here-and-now interaction
between client and therapist (e.g. humanistic therapy, Gestalt therapy)
- Out-session – a large portion of therapeutic work is intended to
happen outside of session (e.g. bibliotherapy, rational emotive behavior
therapy)
The methods used are also different in regards to the population
being served as well as the context and nature of the problem. Therapy
will look very different between, say, a traumatized child, a depressed
but high-functioning adult, a group of people recovering from substance
dependence, and a ward of the state suffering from terrifying delusions.
Other elements that play a critical role in the process of
psychotherapy include the environment, culture, age, cognitive
functioning, motivation, and duration (i.e. brief or long-term therapy).
Four main schools
Many clinical psychologists are
integrative or
eclectic
and draw from the evidence base across different models of therapy in
an integrative way, rather than using a single specific model.
In the UK, clinical psychologists have to show competence in at
least two models of therapy, including CBT, to gain their doctorate. The
British Psychological Society
Division of Clinical Psychology has been vocal about the need to follow
the evidence base rather than being wedded to a single model of
therapy.
Psychodynamic
The psychodynamic perspective developed out of the
psychoanalysis of
Sigmund Freud.
The core object of psychoanalysis is to make the unconscious
conscious—to make the client aware of his or her own primal drives
(namely those relating to sex and aggression) and the various
defenses used to keep them in check. The essential tools of the psychoanalytic process are the use of
free association and an examination of the client's
transference
towards the therapist, defined as the tendency to take unconscious
thoughts or emotions about a significant person (e.g. a parent) and
"transfer" them onto another person. Major variations on Freudian
psychoanalysis practiced today include
self psychology,
ego psychology, and
object relations theory. These general orientations now fall under the umbrella term
psychodynamic psychology,
with common themes including examination of transference and defenses,
an appreciation of the power of the unconscious, and a focus on how
early developments in childhood have shaped the client's current
psychological state.
Humanistic
Humanistic psychology was developed in the 1950s in reaction to both behaviorism and psychoanalysis, largely due to the
person-centered therapy of
Carl Rogers (often referred to as Rogerian Therapy) and
existential psychology developed by
Viktor Frankl and
Rollo May.
Rogers believed that a client needed only three things from a clinician
to experience therapeutic improvement—congruence, unconditional
positive regard, and empathetic understanding. By using
phenomenology,
intersubjectivity
and first-person categories, the humanistic approach seeks to get a
glimpse of the whole person and not just the fragmented parts of the
personality.
This aspect of holism links up with another common aim of humanistic
practice in clinical psychology, which is to seek an integration of the
whole person, also called
self-actualization. From 1980,
Hans-Werner Gessmann integrated the ideas of humanistic psychology into group psychotherapy as
humanistic psychodrama. According to humanistic thinking,
each individual person already has inbuilt potentials and resources
that might help them to build a stronger personality and self-concept.
The mission of the humanistic psychologist is to help the individual
employ these resources via the therapeutic relationship.
Behavioral and cognitive behavioral
Cognitive behavioral therapy (CBT) developed from the combination of
cognitive therapy and
rational emotive behavior therapy, both of which grew out of
cognitive psychology and
behaviorism.
CBT is based on the theory that how we think (cognition), how we feel
(emotion), and how we act (behavior) are related and interact together
in complex ways. In this perspective, certain dysfunctional ways of
interpreting and appraising the world (often through
schemas or
beliefs)
can contribute to emotional distress or result in behavioral problems.
The object of many cognitive behavioral therapies is to discover and
identify the biased, dysfunctional ways of relating or reacting and
through different methodologies help clients transcend these in ways
that will lead to increased well-being. There are many techniques used, such as
systematic desensitization,
socratic questioning,
and keeping a cognition observation log. Modified approaches that fall
into the category of CBT have also developed, including
dialectic behavior therapy and
mindfulness-based cognitive therapy.
Behavior therapy is a rich tradition. It is well researched with a strong evidence base. Its roots are in
behaviorism.
In behavior therapy, environmental events predict the way we think and
feel. Our behavior sets up conditions for the environment to feedback
back on it. Sometimes the feedback leads the behavior to increase-
reinforcement and sometimes the behavior decreases- punishment.
Oftentimes behavior therapists are called
applied behavior analysts or behavioral health counselors. They have studied many areas from developmental disabilities to
depression and
anxiety disorders.
In the area of mental health and addictions a recent article looked at
APA's list for well established and promising practices and found a
considerable number of them based on the principles of operant and
respondent conditioning. Multiple assessment techniques have come from this approach including
functional analysis (psychology),
which has found a strong focus in the school system. In addition,
multiple intervention programs have come from this tradition including
community reinforcement approach for treating addictions,
acceptance and commitment therapy,
functional analytic psychotherapy, including
dialectic behavior therapy and
behavioral activation. In addition, specific techniques such as
contingency management and
exposure therapy have come from this tradition.
Systems or family therapy
Systems or
family therapy
works with couples and families, and emphasizes family relationships as
an important factor in psychological health. The central focus tends to
be on interpersonal dynamics, especially in terms of how change in one
person will affect the entire system.
Therapy is therefore conducted with as many significant members of the
"system" as possible. Goals can include improving communication,
establishing healthy roles, creating alternative narratives, and
addressing problematic behaviors.
Other therapeutic perspectives
There exist dozens of recognized schools or orientations of
psychotherapy—the list below represents a few influential orientations
not given above. Although they all have some typical set of techniques
practitioners employ, they are generally better known for providing a
framework of theory and philosophy that guides a therapist in his or her
working with a client.
- Existential – Existential psychotherapy
postulates that people are largely free to choose who we are and how we
interpret and interact with the world. It intends to help the client
find deeper meaning in life and to accept responsibility for living. As
such, it addresses fundamental issues of life, such as death, aloneness,
and freedom. The therapist emphasizes the client’s ability to be
self-aware, freely make choices in the present, establish personal
identity and social relationships, create meaning, and cope with the
natural anxiety of living.
- Gestalt - Gestalt therapy was primarily founded by Fritz Perls
in the 1950s. This therapy is perhaps best known for using techniques
designed to increase self-awareness, the best-known perhaps being the
"empty chair technique." Such techniques are intended to explore
resistance to "authentic contact", resolve internal conflicts, and help
the client complete "unfinished business".
- Postmodern – Postmodern psychology says that the experience
of reality is a subjective construction built upon language, social
context, and history, with no essential truths.
Since "mental illness" and "mental health" are not recognized as
objective, definable realities, the postmodern psychologist instead sees
the goal of therapy strictly as something constructed by the client and
therapist. Forms of postmodern psychotherapy include narrative therapy, solution-focused therapy, and coherence therapy.
- Transpersonal – The transpersonal perspective places a stronger focus on the spiritual facet of human experience. It is not a set of techniques so much as a willingness to help a client explore spirituality and/or transcendent states of consciousness. It also is concerned with helping clients achieve their highest potential.
- Multiculturalism – Although the theoretical foundations of
psychology are rooted in European culture, there is a growing
recognition that there exist profound differences between various ethnic
and social groups and that systems of psychotherapy need to take those
differences into greater consideration.
Further, the generations following immigrant migration will have some
combination of two or more cultures—with aspects coming from the parents
and from the surrounding society—and this process of acculturation
can play a strong role in therapy (and might itself be the presenting
problem). Culture influences ideas about change, help-seeking, locus of
control, authority, and the importance of the individual versus the
group, all of which can potentially clash with certain givens in
mainstream psychotherapeutic theory and practice.
As such, there is a growing movement to integrate knowledge of various
cultural groups in order to inform therapeutic practice in a more
culturally sensitive and effective way.
- Feminism – Feminist therapy
is an orientation arising from the disparity between the origin of most
psychological theories (which have male authors) and the majority of
people seeking counseling being female. It focuses on societal,
cultural, and political causes and solutions to issues faced in the
counseling process. It openly encourages the client to participate in
the world in a more social and political way.
- Positive psychology – Positive psychology is the scientific study of human happiness and well-being, which started to gain momentum in 1998 due to the call of Martin Seligman, then president of the APA. The history of psychology shows that the field has been primarily dedicated to addressing mental illness
rather than mental wellness. Applied positive psychology's main focus,
therefore, is to increase one's positive experience of life and ability
to flourish by promoting such things as optimism about the future, a
sense of flow in the present, and personal traits like courage,
perseverance, and altruism.
There is now preliminary empirical evidence to show that by promoting
Seligman's three components of happiness—positive emotion (the pleasant
life), engagement (the engaged life), and meaning (the meaningful
life)—positive therapy can decrease clinical depression.
Integration
In the last couple of decades, there has been a growing movement to
integrate the various therapeutic approaches, especially with an
increased understanding of cultural, gender, spiritual, and
sexual-orientation issues. Clinical psychologists are beginning to look
at the various strengths and weaknesses of each orientation while also
working with related fields, such as
neuroscience,
behavioral genetics,
evolutionary biology, and
psychopharmacology.
The result is a growing practice of eclecticism, with psychologists
learning various systems and the most efficacious methods of therapy
with the intent to provide the best solution for any given problem.
Professional ethics
The field of clinical psychology in most countries is strongly
regulated by a code of ethics. In the U.S., professional ethics are
largely defined by the APA Code of Conduct, which is often used
by states to define licensing requirements. The APA Code generally sets a
higher standard than that which is required by law as it is designed to
guide responsible behavior, the protection of clients, and the
improvement of individuals, organizations, and society. The Code is applicable to all psychologists in both research and applied fields.
The APA Code is based on five principles: Beneficence and
Nonmaleficence, Fidelity and Responsibility, Integrity, Justice, and
Respect for People's Rights and Dignity.
Detailed elements address how to resolve ethical issues, competence,
human relations, privacy and confidentiality, advertising, record
keeping, fees, training, research, publication, assessment, and therapy.
In the UK the
British Psychological Society
has published a Code of Conduct and Ethics for clinical psychologists.
This has four key areas: Respect, Competence, Responsibility and
Integrity. Other European professional organisations have similar codes of conduct and ethics.
Comparison with other mental health professions
Psychiatry
Although clinical psychologists and
psychiatrists
can be said to share a same fundamental aim—the alleviation of mental
distress—their training, outlook, and methodologies are often quite
different. Perhaps the most significant difference is that psychiatrists
are licensed physicians. As such, psychiatrists often use the
medical model to assess psychological problems (i.e., those they treat are seen as patients with an illness) and rely on
psychotropic medications as the chief method of addressing the illness—although many also employ
psychotherapy as well. Psychiatrists and
medical psychologists
(who are clinical psychologists that are also licensed to prescribe)
are able to conduct physical examinations, order and interpret
laboratory tests and
EEGs, and may order brain imaging studies such as
CT or
CAT,
MRI, and
PET scanning.
Clinical psychologists generally do not
prescribe medication, although there is a growing movement for psychologists to have
prescribing privileges. These medical privileges require additional training and education. To date,
medical psychologists
may prescribe psychotropic medications in Guam, Iowa, Idaho, Illinois,
New Mexico, Louisiana, the Public Health Service, the Indian Health
Service, and the United States Military.
Counseling psychology
Counseling psychologists
undergo the same level of rigor in study and use many of the same
interventions and tools as clinical psychologists, including
psychotherapy and assessment. Traditionally, counseling psychologists
helped people with what might be considered normal or moderate
psychological problems—such as the feelings of anxiety or sadness
resulting from major life changes or events.
However, that distinction has faded over time, and of the counseling
psychologists who do not go into academia (which does not involve
treatment or diagnosis), the majority of counseling psychologists treat
mental illness alongside clinical psychologists. Many counseling
psychologists also receive specialized training in career assessment,
group therapy, and relationship counseling.
Counseling psychology as a field values multiculturalism
and social advocacy, often stimulating research in multicultural
issues. There are fewer counseling psychology graduate programs than
those for clinical psychology and they are more often housed in
departments of education rather than psychology. Counseling
psychologists tend to be more frequently employed in university
counseling centers compared to hospitals and private practice for
clinical psychologists.
However, counseling and clinical psychologists can be employed in a
variety of settings, with a large degree of overlap (prisons, colleges,
community mental health, non-profits, corporations, private practice,
hospitals and Veterans Affairs). Distinctions between the two fields
continue to fade.
| Comparison of mental health professionals in USA
|
| Occupation
|
Degree
|
Common Licenses
|
Prescription Privilege
|
Ave. 2004
Income (USD)
|
| Clinical Psychologist
|
PhD/PsyD
|
Psychologist
|
Mostly no
|
$75,000
|
| Counseling Psychologist (Doctorate)
|
PhD/PsyD
|
Psychologist
|
No
|
$65,000
|
| Counseling Psychologist (Master's)
|
MA/MS/MC
|
MFT/LPC/LPA
|
No
|
$49,000
|
| School Psychologist
|
PhD, EdD
|
Psychologist
|
No
|
$78,000
|
| Psychiatrist
|
MD/DO
|
Psychiatrist
|
Yes
|
$145,600
|
| Clinical Social Worker
|
PhD/MSW
|
LCSW
|
No
|
$36,170
|
| Psychiatric Nurse
|
PhD/MSN/BSN
|
APRN/PMHN
|
No
|
$53,450
|
| Psychiatric and mental health Nurse Practitioner
|
DNP/MSN
|
MHNP
|
Yes (Varies by state)
|
$75,711
|
| Expressive/Art Therapist
|
MA
|
ATR
|
No
|
$45,000
|
School psychology
School psychologists
are primarily concerned with the academic, social, and emotional
well-being of children and adolescents within a scholastic environment.
In the U.K., they are known as "educational psychologists". Like
clinical (and counseling) psychologists, school psychologists with
doctoral degrees are eligible for licensure as health service
psychologists, and many work in private practice. Unlike clinical
psychologists, they receive much more training in education, child
development and behavior, and the psychology of learning. Common degrees
include the
Educational Specialist Degree (Ed.S.),
Doctor of Philosophy (Ph.D.), and
Doctor of Education (Ed.D.).
Traditional job roles for school psychologists employed in school
settings have focused mainly on assessment of students to determine
their eligibility for special education services in schools, and on
consultation with teachers and other school professionals to design and
carry out interventions on behalf of students. Other major roles also
include offering individual and group therapy with children and their
families, designing prevention programs (e.g. for reducing dropout),
evaluating school programs, and working with teachers and administrators
to help maximize teaching efficacy, both in the classroom and
systemically.
Clinical social work
Social workers
provide a variety of services, generally concerned with social
problems, their causes, and their solutions. With specific training,
clinical social workers may also provide psychological counseling (in
the U.S. and Canada), in addition to more traditional social work. The
Masters in Social Work in the U.S. is a two-year, sixty credit program
that includes at least a one-year practicum (two years for clinicians).
Occupational therapy
Occupational therapy—often
abbreviated OT—is the "use of productive or creative activity in the
treatment or rehabilitation of physically, cognitively, or emotionally
disabled people."
Most commonly, occupational therapists work with people with
disabilities to enable them to maximize their skills and abilities.
Occupational therapy practitioners are skilled professionals whose
education includes the study of human growth and development with
specific emphasis on the physical, emotional, psychological,
sociocultural,
cognitive
and environmental components of illness and injury. They commonly work
alongside clinical psychologists in settings such as inpatient and
outpatient mental health, pain management clinics, eating disorder
clinics, and child development services. OT's use support groups,
individual counseling sessions, and activity-based approaches to address
psychiatric symptoms and maximize functioning in life activities.
Criticisms and controversies
Clinical
psychology is a diverse field and there have been recurring tensions
over the degree to which clinical practice should be limited to
treatments supported by empirical research. Despite some evidence showing that all the major therapeutic orientations are about of equal effectiveness, there remains much debate about the efficacy of various forms treatment in use in clinical psychology.
It has been reported that clinical psychology has rarely allied itself with
client groups
and tends to individualize problems to the neglect of wider economic,
political and social inequality issues that may not be the
responsibility of the client.
It has been argued that therapeutic practices are inevitably bound up
with power inequalities, which can be used for good and bad. A
critical psychology
movement has argued that clinical psychology, and other professions
making up a "psy complex", often fail to consider or address
inequalities and power differences and can play a part in the social and
moral control of disadvantage, deviance and unrest.
An October 2009 editorial in the journal
Nature
suggests that a large number of clinical psychology practitioners in
the United States consider scientific evidence to be "less important
than their personal – that is, subjective – clinical experience."