 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Champix, Chantix, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a606024 |
| License data |
|
| Pregnancy category | |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | <20 span=""> |
| Metabolism | Limited (<10 span=""> |
| Elimination half-life | 24 hours |
| Excretion | Renal (81–92%) |
| Identifiers | |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
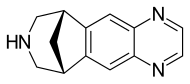
| Formula | C13H13N3 |
| Molar mass | 211.267 g·mol−1 |
| 3D model (JSmol) | |
Varenicline (trade name Chantix and Champix) is a prescription medication used to treat nicotine addiction. It reduces both craving for and decreases the pleasurable effects of cigarettes and other tobacco products.
It is a high-affinity partial agonist for the α4β2 nicotinic acetylcholine receptor subtype (nACh) that leads to the release of dopamine in the nucleus accumbens when activated, and therefore, has the capacity to reduce the feelings of craving and withdrawal caused by smoking cessation. In this respect it is similar to cytisine and different from the nicotinic antagonist bupropion and nicotine replacement therapies (NRTs) like nicotine patches and nicotine gum. It is estimated that varenicline successfully helps one of every 11 people who smoke remain abstinent from tobacco at six months.
Medical uses
Varenicline is used to help people stop smoking tobacco (smoking cessation). A meta-analysis found that less than 20% of people treated with varenicline remain abstinent from smoking at one year. In a 2009 meta-analysis varenicline was found to be more effective than bupropion (odds ratio 1.40) and nicotine replacement therapies (NRT) (odds ratio 1.56).
A 2013 Cochrane overview and network meta-analysis concluded that
varenicline is the most effective medication for tobacco cessation and
that smokers were nearly three times more likely to quit on varenicline
than with placebo treatment. Varenicline was more efficacious than
bupropion or NRT and as effective as combination NRT for tobacco smoking
cessation.
The United States' Food and Drug Administration
(US FDA) has approved the use of varenicline for up to twelve weeks. If
smoking cessation has been achieved it may be continued for another
twelve weeks.
Varenicline has not been tested in those under 18 years old or
pregnant women and therefore is not recommended for use by these groups. Varenicline is considered a class C
pregnancy drug, as animal studies have shown no increased risk of
congenital anomalies; however, no data from human studies is available.
An observational study is currently being conducted assessing for
malformations related to varenicline exposure, but has no results yet.
An alternate drug is preferred for smoking cessation during
breastfeeding due to lack of information and based on the animal studies
on nicotine.
Side effects
Mild nausea
is the most common side effect and is seen in approximately 30% of
people taking varenicline though this rarely (<3 a="" common="" discontinuation="" effects="" href="https://en.wikipedia.org/wiki/Headache" in="" include="" less="" medication.="" of="" other="" results="" side="" the="" title="Headache">headache
, difficulty sleeping, and nightmares. Rare side effects reported by people taking varenicline compared to placebo include change in taste, vomiting, abdominal pain, flatulence, and constipation.
It has been estimated that for every five subjects taking varenicline
at maintenance doses, there will be an event of nausea, and for every 24
and 35 treated subjects, there will be an event of constipation and
flatulence, respectively. Gastrointestinal side-effects lead to
discontinuation of the drug in 2% to 8% of people using varenicline.
Incidence of nausea is dose-dependent: incidence of nausea was higher
in people taking a larger dose (30%) versus placebo (10%) as compared to
people taking a smaller dose (16%) versus placebo (11%).
Depression and suicide
In 2007, the US FDA had announced it had received post-marketing reports of thoughts of suicide and occasional suicidal behavior,
erratic behavior, and drowsiness among people using varenicline for
smoking cessation. In 2009, the US FDA required varenicline to carry a boxed warning that the drug should be stopped if any of these symptoms are experienced.
A 2014 systematic review did not find evidence of an increased suicide risk. Other analyses have reached the same conclusion and found no increased risk of neuropsychiatric side effects with varenicline.
No evidence for increased risks of cardiovascular events, depression,
or self-harm with varenicline versus nicotine replacement therapy has
been found in one post-marketing surveillance study.
In 2016 the FDA removed the black box warning. People are still advised to stop the medication if they "notice any side effects on mood, behavior, or thinking."
Cardiovascular disease
In
June 2011, the US FDA issued a safety announcement that varenicline may
be associated with "a small, increased risk of certain cardiovascular
adverse events in people who have cardiovascular disease."
A prior 2011 review had found increased risk of cardiovascular events compared with placebo. Expert commentary in the same journal raised doubts about the methodology of the review, concerns which were echoed by the European Medicines Agency and subsequent reviews.
Of specific concern were "the low number of events seen, the types of
events counted, the higher drop-out rate in people receiving placebo,
the lack of information on the timing of events, and the exclusion of
studies in which no-one had an event."
In contrast, multiple recent systematic reviews and meta-analyses
have found no increase in overall or serious adverse cardiovascular
events (including for individuals at risk of developing cardiovascular
disease) associated with varenicline use.
Alcohol
It is recommended that people reduce the amount of alcohol they drink when on Varenicline.
Mechanism of action
Varenicline displays full agonism on α7 nicotinic acetylcholine receptors and is a partial agonist on the α4β2, α3β4, and α6β2 subtypes. In addition, it is a weak agonist on the α3β2 containing receptors.
Varenicline's partial agonism on the α4β2 receptors rather than nicotine's full agonism produces less effect of dopamine release than nicotine's. This α4β2
competitive binding reduces the ability of nicotine to bind and
stimulate the mesolimbic dopamine system - similar to the method of
action of buprenorphine in the treatment of opioid addiction.
Pharmacokinetics
Most of the active compound is excreted by the kidneys (92–93%). A small proportion is glucuronidated, oxidised, N-formylated or conjugated to a hexose. The elimination half-life is about 24 hours.
History
Use of Cytisus plant as a smoking substitute during World War II led to use as a cessation aid in eastern Europe and extraction of cytisine. Cytisine analogs led to varenicline at Pfizer.
Varenicline received a "priority review" by the US FDA in
February 2006, shortening the usual 10-month review period to 6 months
because of its demonstrated effectiveness in clinical trials and perceived lack of safety issues. The agency's approval of the drug came on May 11, 2006.
On August 1, 2006, varenicline was made available for sale in the
United States and on September 29, 2006, was approved for sale in the European Union.
