From Wikipedia, the free encyclopedia
| Schizoaffective disorder |
|---|
| Specialty | Psychiatry |
|---|
| Symptoms | Hallucinations, delusions, disorganized thinking, depressed mood, manic behavior |
|---|
| Complications | Social isolation, suicide |
|---|
| Types | Bipolar type, depressive type |
|---|
| Causes | Unknown |
|---|
| Risk factors | Genetics, brain chemistry and structure, stress, drug use, trauma from abuse |
|---|
| Medication | Antipsychotics, mood stabilizers |
|---|
Schizoaffective disorder (
SZA,
SZD or
SAD) is a
mental disorder characterized by
abnormal thought processes and an
unstable mood. The diagnosis is made when the person has symptoms of both
schizophrenia (usually psychosis) and a mood disorder—either
bipolar disorder or
depression—but does not meet the diagnostic criteria for schizophrenia or a mood disorder individually.
The main criterion for the schizoaffective disorder diagnosis is the
presence of psychotic symptoms for at least two weeks without any mood
symptoms present. Schizoaffective disorder can often be
misdiagnosed when the correct diagnosis may be
psychotic depression, psychotic
bipolar disorder,
schizophreniform disorder, or
schizophrenia. It is imperative for providers to accurately diagnose patients, as treatment and
prognosis differs greatly for each of these diagnoses.
There are two types of schizoaffective disorder: the
bipolar type, which is distinguished by symptoms of
mania,
hypomania, or
mixed episode; and the
depressive type, which is distinguished by symptoms of
depression only. Common symptoms of the disorder include
hallucinations,
delusions, and
disorganized speech and thinking.
Auditory hallucinations, or "hearing voices," are most common. The onset of symptoms usually begins in young adulthood.
Genetics (researched in the field of
genomics); problems with
neural circuits; chronic early, and chronic or short-term current
environmental stress
appear to be important causal factors. No single isolated organic cause
has been found, but extensive evidence exists for abnormalities in the
metabolism of
tetrahydrobiopterin (BH4),
dopamine, and
glutamic acid
in people with schizophrenia, psychotic mood disorders, and
schizoaffective disorder. People with schizoaffective disorder are
likely to have
co-occurring conditions, including
anxiety disorders and
substance use disorders.
The mainstay of current treatment is
antipsychotic medication combined with
mood stabilizer medication or
antidepressant
medication, or both. There is growing concern by some researchers that
antidepressants may increase psychosis, mania, and long-term mood
episode cycling in the disorder. When there is risk to self or others, usually early in treatment, hospitalization may be necessary.
Psychiatric rehabilitation,
psychotherapy, and
vocational rehabilitation are very important for
recovery of higher psychosocial function. As a group, people with schizoaffective disorder that were diagnosed using
DSM-IV and
ICD-10 criteria (which have since been updated) have a better
outcome, but have variable individual psychosocial functional outcomes compared to people with mood disorders, from worse to the same. Outcomes for people with
DSM-5 diagnosed schizoaffective disorder depend on data from
prospective cohort studies, which have not been completed yet. The DSM-5 diagnosis was updated because DSM-IV criteria resulted in overuse of the diagnosis; that is, DSM-IV criteria led to many patients being misdiagnosed with the disorder. DSM-IV
prevalence estimates were less than one percent of the population, in the range of 0.5–0.8 percent; newer DSM-5 prevalence estimates are not yet available.
Signs and symptoms
Schizoaffective disorder is defined by
mood disorder-free psychosis in the context of a long-term psychotic and mood disorder.
Psychosis must meet criterion A for
schizophrenia which may include
delusions,
hallucinations,
disorganized speech, thinking or behavior and
negative symptoms. Both delusions and hallucinations are classic symptoms of psychosis. Delusions are false beliefs which are strongly held despite evidence to the contrary.
Beliefs should not be considered delusional if they are in keeping
with cultural beliefs. Delusional beliefs may or may not reflect mood
symptoms (for example, someone experiencing depression may or may not
experience delusions of guilt). Hallucinations are disturbances in
perception involving any of the five senses, although
auditory hallucinations (or "hearing voices") are the most common. A lack of responsiveness or negative symptoms include
alogia (lack of spontaneous speech),
blunted affect (reduced intensity of outward emotional expression),
avolition (loss of motivation), and
anhedonia (inability to experience pleasure). Negative symptoms can be more lasting and more debilitating than positive symptoms of psychosis.
Mood symptoms are of
mania,
hypomania,
mixed episode, or
depression, and tend to be episodic rather than continuous. A
mixed episode
represents a combination of symptoms of mania and depression at the
same time. Symptoms of mania include elevated or irritable mood,
grandiosity (inflated self-esteem), agitation, risk-taking behavior,
decreased need for sleep, poor concentration, rapid speech, and racing
thoughts.
Symptoms of depression include low mood, apathy, changes in appetite
or weight, disturbances in sleep, changes in motor activity, fatigue,
guilt or feelings of worthlessness, and suicidal thinking.
DSM-5 states that if a patient only experiences psychotic
symptoms during a mood episode, their diagnosis is Mood Disorder with
Psychotic Features and not Schizophrenia or Schizoaffective Disorder. If
the patient experiences psychotic symptoms without mood symptoms for
longer than a two-week period, their diagnosis is either Schizophrenia
or Schizoaffective Disorder. If mood disorder episodes are present for
the majority and residual course of the illness and up until the
diagnosis, the patient can be diagnosed with Schizoaffective Disorder.
Causes
A combination of genetic and
environmental factors are believed to play a role in the development of schizoaffective disorder.
Genetic studies do not support the view that schizophrenia, psychotic mood disorders and schizoaffective disorder are distinct etiological
entities, but rather the evidence suggests the existence of common
inherited vulnerability that increases the risks for all these syndromes. Some susceptibility pathways may be specific for schizophrenia, others for bipolar disorder,
and yet other mechanisms and genes may confer risk for mixed
schizophrenic and affective [or mood disorder] psychoses, but there is
no support from genetics for the view that these are distinct disorders
with distinct etiologies and pathogenesis. Laboratory studies of putative endophenotypes, brain imaging studies, and post mortem studies shed little additional light on the validity
of the schizoaffective disorder diagnosis, as most studies combine
subjects with different chronic psychoses in comparison to healthy
subjects.
Viewed broadly then, biological and environmental factors interact
with a person's genes in ways which may increase or decrease the risk
for developing schizoaffective disorder; exactly how this happens (the
biological mechanism) is not yet known. Schizophrenia spectrum
disorders, of which schizoaffective disorder is a part, have been
increasingly linked to advanced
paternal age at the time of conception, a known cause of genetic mutations.
The physiology of people diagnosed with schizoaffective disorder
appears to be similar, but not identical, to that of those diagnosed
with schizophrenia and bipolar disorder; however, human
neurophysiological function in normal brain and mental disorder
syndromes is not fully understood.
Substance abuse
A
clear causal connection between drug use and psychotic spectrum
disorders, including schizoaffective disorder, has been difficult to
prove. In the specific case of
cannabis (marijuana), however, evidence supports a link between earlier onset of psychotic illness and cannabis use. The more often cannabis is used, particularly in early adolescence, the more likely a person is to develop a psychotic illness, with frequent use being correlated with double the risk of psychosis and schizoaffective disorder. A 2009 Yale review stated that in individuals with an established psychotic disorder,
cannabinoids can exacerbate symptoms, trigger relapse, and have negative consequences on the course of the illness. While cannabis use is accepted as a contributory cause of schizoaffective disorder by many, it remains controversial, since not all young people who use cannabis later develop psychosis, but those who do use cannabis have an increased
odds ratio of about 3.
Certain drugs can imitate symptoms of schizophrenia (which we know has
similar symptoms to schizoaffective disorder). This is important to note
when including that substance-induced psychosis should be ruled out
when diagnosing patients so that patients are not misdiagnosed.
Diagnosis
Psychosis as a
symptom of a psychiatric disorder is first and foremost a
diagnosis of exclusion. So a new-onset episode of psychosis
cannot
be considered to be a symptom of a psychiatric disorder until other
relevant and known medical causes of psychosis are excluded, or ruled
out. Many clinicians improperly perform, or entirely miss this step, introducing avoidable diagnostic error and misdiagnosis.
An initial assessment includes a comprehensive history and
physical examination. Although no biological laboratory tests exist
which confirm schizoaffective disorder, biological tests should be
performed to
exclude
psychosis associated with or caused by substance use, medications,
toxins or poisons, surgical complications, or other medical illnesses.
Since non-medical mental health practitioners are not trained to exclude
medical causes of psychosis, people experiencing psychosis should be
referred to an emergency department or hospital.
Delirium
should be ruled out, which can be distinguished by visual
hallucinations, acute onset and fluctuating level of consciousness,
indicating other underlying factors which includes medical illnesses. Excluding medical illnesses associated with psychosis is performed by using
blood tests to measure:
Other investigations which may be performed include:
Blood tests are not usually repeated for relapse in people with an
established diagnosis of schizoaffective disorder, unless there is a
specific
medical indication. These may include serum
BSL if
olanzapine has previously been prescribed, thyroid function if lithium has previously been taken to rule out
hypothyroidism, liver function tests if
chlorpromazine has been prescribed,
CPK levels to exclude
neuroleptic malignant syndrome,
and a urinalysis and serum toxicology screening if substance use is
suspected. Assessment and treatment may be done on an outpatient basis;
admission to an inpatient facility is considered if there is a risk to
self or others.
Illicit drugs aren't the only ones that precipitate
psychosis or mania—prescribed drugs can too, and in particular, some
psychiatric drugs. We investigated this and found that about 1 in 12
psychotic or manic patients in an inpatient psychiatric facility are
there due to antidepressant-induced psychosis or mania. That's
unfortunate for the field [of psychiatry] and disastrous for some of our
patients.
It is important to be understood
here. I want to call attention to the fact that some persons with a
family history of even the subtler forms of bipolar disorder or
psychosis are more vulnerable than others to the mania- or
psychosis-inducing potential of antidepressants, stimulants and sleeping
medications. While I'm not making a blanket statement against these
medications, I am urging caution in their use. I believe
[clinicians] should ask patients and their families whether there is a
family history of bipolar disorder or psychosis before prescribing these
medications. Most patients and their families don't know the answer
when they are first asked, so time should be allowed for the patient to
ask family or relatives, between the session when asked by [the
clinician] and a follow-up session. This may increase the wait for a
medication slightly, but because some patients are vulnerable, this is a
necessary step for [the clinician] to take. I believe that psychiatry as a field has not emphasized this point sufficiently.
As a result, some patients have been harmed by the very treatments that
were supposed to help them; or to the disgrace of psychiatry, harmed and then misdiagnosed.
Substance-induced psychosis should also be ruled out. Both substance- and medication-induced psychosis can be
excluded to a high level of certainty while the person is psychotic, typically in an emergency department, using both a
- Broad spectrum urine toxicology screening, and a
- Full serum toxicology screening (of the blood).
Some
dietary supplements
may also induce psychosis or mania, but cannot be ruled out with
laboratory tests. So a psychotic person's family, partner, or friends
should be asked whether he or she is currently taking any dietary
supplements.
Common mistakes made when diagnosing psychotic patients include:
- Not properly excluding delirium,
- Missing a toxic psychosis by not screening for substances and medications,
- Not appreciating medical abnormalities (e.g., vital signs),
- Not obtaining a medical history and family history,
- Indiscriminate screening without an organizing framework,
- Not asking family or others about dietary supplements,
- Premature diagnostic closure, and
- Not revisiting or questioning the initial diagnostic impression of primary psychiatric disorder.
Only after these relevant and known causes of psychosis have been ruled out can a psychiatric
differential diagnosis
be made. A mental health clinician will incorporate family history,
observation of a psychotic person's behavior while the person is
experiencing active symptoms, to begin a psychiatric differential
diagnosis. Diagnosis also includes self-reported experiences, as well as
behavioral abnormalities reported by family members, friends, or
significant others. Mistakes in this stage include:
DSM-5 criteria
The DSM-IV schizoaffective disorder definition was plagued by problems of being inconsistently (or
unreliably) used on patients; when the diagnosis is made, it doesn't stay with most patients over time; and it has questionable
diagnostic validity (that is, it doesn't describe a distinct disorder, nor predict any particular outcome). These problems have been slightly reduced (or "modestly improved") in the
DSM-5 according to Carpenter.
The second cardinal guideline in the DSM-5 diagnosis of schizoaffective disorder is one of timeframe.
- DSM-5 requires two episodes of psychosis (whereas DSM-IV needed only one) to qualify for the schizoaffective disorder diagnosis. As such, it is no longer an "episode diagnosis."
The new schizoaffective framework looks at the time from "the [first
episode of] psychosis up to the current episode [of psychosis], rather
than only defining a single episode with [co-occurring] psychotic and
mood syndromes."
Specifically, one of the episodes of psychosis must last a minimum of
two weeks without mood disorder symptoms, but the person may be mildly
to moderately depressed while psychotic.
The other period of psychosis "requires the overlap of mood [disorder]
symptoms with psychotic symptoms to be conspicuous" and last for a
greater portion of the disorder.
These two changes are intended by the DSM-5 workgroup to accomplish two goals:
- Increase the diagnosis' consistency (or reliability) when it is used;
- Significantly decrease the overall use of the schizoaffective disorder diagnosis.
If the schizoaffective diagnosis is used less often, other diagnoses
(like psychotic mood disorders and schizophrenia) are likely to be used
more often; but this is hypothetical until real-world data arrive.
Validity problems with the diagnosis remain and await further work in
the fields of
psychiatric genetics,
neuroimaging, and
cognitive science that includes the overlapping fields of
cognitive,
affective, and
social neuroscience, which may change the way schizoaffective disorder is
conceptualized and defined in future versions of the
DSM and
ICD.
Types
One of two types of schizoaffective disorder may be noted in a diagnosis based on the mood component of the disorder:
- Bipolar type, when the disturbance includes manic episodes, hypomania, or mixed episodes—major depressive episodes also typically occur;
- Depressive type, when the disturbance includes major depressive
episodes exclusively—that is, without manic, hypomanic, or mixed
episodes.
Problems with DSM-IV schizoaffective disorder
The
American Psychiatric Association's
DSM-IV criteria for schizoaffective disorder persisted for 19 years
(1994–2013). Clinicians adequately trained in diagnosis used the
schizoaffective diagnosis too often, largely because the criteria were poorly defined,
ambiguous, and hard to use (or poorly
operationalized). Poorly trained clinicians used the diagnosis without making necessary
exclusions of common causes of psychosis, including some prescribed psychiatric medications.
Specialty books written by experts on schizoaffective disorder have
existed for over eight years before DSM-5 describing the overuse of the
diagnosis.
Carpenter and the DSM-5 schizoaffective disorders workgroup
analyzed data made available to them in 2009, and reported in May 2013
that:
a recent review of psychotic disorders from large private
insurance and Medicare databases in the U.S. found that the diagnosis
of DSM-IV schizoaffective disorder was used for about a third of cases
with non-affective psychotic disorders. Hence, this unreliable and
poorly defined diagnosis is clearly overused.
As stated above, the DSM-IV schizoaffective disorder diagnosis is very inconsistently used or unreliable.
A diagnosis is unreliable when several different mental health
professionals observing the same individual make different diagnoses
excessively.
Even when a structured DSM-IV diagnostic interview and best estimate
procedures were made by experts in the field that included information
from family informants and prior clinical records,
reliability was still poor for the DSM-IV schizoaffective diagnosis.
The DSM-IV schizoaffective diagnosis isn't stable over time either.
An initial diagnosis of schizoaffective disorder during time spent at a
psychiatric inpatient facility was stable at 6-month and 24-month
follow ups for only 36% of patients. By comparison, diagnostic stability was 92% for schizophrenia, 83% for bipolar disorder and 74% for major depression.
Most patients diagnosed with DSM-IV schizoaffective disorder are later
diagnosed with a different disorder, and that disorder is more stable
over time than the DSM-IV schizoaffective disorder diagnosis.
In April 2009, Carpenter and the DSM-5 schizoaffective disorder
workgroup reported that they were "developing new criteria for
schizoaffective disorder to improve reliability and
face validity,"
and were "determining whether the dimensional assessment of mood
[would] justify a recommendation to drop schizoaffective disorder as a
diagnostic category." Speaking to an audience at the May 2009 annual conference of the
American Psychiatric Association, Carpenter said:
We had hoped to get rid of schizoaffective [disorder] as a
diagnostic category [in the DSM-5] because we don't think it's [a]
valid [scientific entity] and we don't think it's reliable. On the other
hand, we think it's absolutely indispensable to clinical practice.
A major reason why DSM-IV schizoaffective disorder was indispensable
to clinical practice is because it offered clinicians a diagnosis for
patients with psychosis in the context of mood disorder whose clinical
picture, at the time diagnosed, appeared different from DSM-IV
"schizophrenia" or "mood disorder with psychotic features."
But DSM-IV schizoaffective disorder carries an unnecessarily
worse prognosis than a "mood disorder with psychotic features"
diagnosis, because
long-term data
revealed that a significant proportion of DSM-IV schizoaffective
disorder patients had 15-year outcomes indistinguishable from patients
with mood disorders with or without psychotic features, even though the clinical picture at the time of first diagnosis looked different from both schizophrenia and mood disorders.
These problems with the DSM-IV schizoaffective disorder
definition result in most people the diagnosis is used on being
misdiagnosed; furthermore,
outcome studies
done 10 years after the diagnosis was released showed that the group of
patients defined by the DSM-IV and ICD-10 schizoaffective diagnosis had
significantly better outcomes than predicted, so the diagnosis carries a
misleading and unnecessarily poor
prognosis.
The DSM-IV criteria for schizoaffective disorder will continue to be
used on U.S. board examinations in psychiatry through the end of 2014;
established practitioners may continue to use the problematic DSM-IV
definition much further into the future also.
DSM-5 research directions
The new schizoaffective disorder criteria continue to have questionable diagnostic validity.
Questionable diagnostic validity does not doubt that people with
symptoms of psychosis and mood disorder need treatment—psychosis and
mood disorder must be treated. Instead, questionable diagnostic validity
means there are unresolved problems with the way the DSM-5
categorizes and defines schizoaffective disorder.
A core concept in modern psychiatry since
DSM-III was released in 1980, is the categorical separation of mood disorders from schizophrenia, known as the
Kraepelinian dichotomy.
Emil Kraepelin
introduced the idea that schizophrenia was separate from mood disorders
after observing patients with symptoms of psychosis and mood disorder,
over a century ago, in 1898. This was a time before
genetics were known and before any treatments existed for
mental illness. The Kraepelinian dichotomy wasn't used for
DSM-I and
DSM-II because both manuals were influenced by the dominant
psychodynamic psychiatry of the time, but the designers of DSM-III wanted to use more scientific and biological definitions.
Consequently, they looked to psychiatry's history and decided to use
the Kraepelinian dichotomy as a foundation for the classification
system.
The Kraepelinian dichotomy continues to be used in DSM-5 despite having been challenged by
data from modern psychiatric genetics for over eight years, and there is now
evidence of a significant overlap in the genetics of schizophrenia and bipolar disorder.
According to this genetic evidence, the Kraepelinian categorical
separation of mood disorders from schizophrenia at the foundation of the
current classification and diagnostic system is a mistaken
false dichotomy.
The dichotomy at the foundation of the current system forms the
basis for a convoluted schizoaffective disorder definition in DSM-IV
that resulted in excessive misdiagnosis.
Real life schizoaffective disorder patients have significant and
enduring symptoms that bridge what are incorrectly assumed to be
categorically separate disorders, schizophrenia and bipolar disorder. People with
psychotic depression,
bipolar disorder with a history of psychosis, and schizophrenia with
mood symptoms also have symptoms that bridge psychosis and mood
disorders.
The categorical diagnostic manuals don't reflect reality in their
separation of psychosis (via the schizophrenia diagnosis) from mood
disorder, nor do they currently emphasize the actual overlap found in
real-life patients. Thus, they are likely to continue to introduce
either-or conceptual and diagnostic error, by way of
confirmation bias into clinicians'
mindsets, hindering accurate assessment and treatment.
The new definition continues the lack of
parsimony of the old definition.
Simpler, clearer, and more usable definitions of the diagnosis were
supported by certain members of the DSM-5 workgroup (see next
paragraph); these were debated but deemed premature, because more
"research [is] needed to establish a new
classification system of equal or greater validity" to the existing system.
Because of DSM-5's continuing problematic categorical foundation,
schizoaffective disorder's conceptual and diagnostic validity remains
doubtful. After enough research is completed and
data
exists, future diagnostic advances will need to either eliminate and
replace, or soften and bridge, the hard categorical separation of mood
disorders from schizophrenia; most likely using a
spectrum or dimensional approach to diagnosis.
More
parsimonious definitions than the current one were considered by Carpenter and the DSM-5 workgroup:
One option for the DSM-5 would have been to remove the
schizoaffective disorder category and to add affective [or mood]
symptoms [that is, mania, hypomania, mixed episode, or depression] as a dimension to schizophrenia and schizophreniform disorder or
to define a single category for the co-occurrence of psychosis and mood
symptoms. This option was extensively debated but ultimately deemed to
be premature in the absence of sufficient clinical and theoretical
validating data justifying such a … reconceptualization. Additionally,
there appeared to be no practical way to introduce affect [or mood]
dimensions covering the entire course of illness, that would capture the
current concept of periods of psychosis related and unrelated to mood episodes.
[N]o valid biomarkers or laboratory measures have emerged to distinguish between affective psychosis [or psychotic mood disorders] and schizophrenia. To the contrary, the idea of a dichotomy between these types of conditions has proven naïve.
[T]he admixture of “schizophrenic” and affective [or mood] symptoms is a
feature of many, or even most, cases with severe mental illness. Most presenting symptoms of psychosis have little validity in determining diagnosis, prognosis, or treatment response in psychosis. [U]ltimately a more … dimensional approach [to assessment and treatment] will be required.
The field of
psychiatry has begun to question its assumptions and analyze its data in order to merge closer with
evidence-based medicine.
The removal of the "episode diagnosis," and the addition of two
episodes of psychosis, as qualifications for the DSM-5 schizoaffective
diagnosis, may improve the diagnosis' consistency over DSM-IV for
research purposes, where diagnostic criteria are by necessity followed
exactingly.
But the new definition remains long, unwieldy, and perhaps still not
very useful for community clinicians—with two psychoses, one for two
weeks minimum and without mood disorder (but the person can be mildly or
moderately depressed) and the other with significant mood disorder and
psychosis lasting for most of the time, and with lasting mood symptoms
for most of the residual portion of the illness. Community clinicians used the previous definition "for about a third of cases with non-affective psychotic disorders."
Non-affective psychotic disorders are, by definition, not
schizoaffective disorder. For clinicians to make such sizeable errors of
misdiagnosis may imply systemic problems with the schizoaffective
disorder diagnosis itself. Already, at least one expert believes the new
schizoaffective definition hasn't gone far enough to solve the previous
definition's problems.
From a scientific standpoint, modern clinical psychiatry is still
a very young, underdeveloped medical specialty because its target
organ, the human brain, is not yet well understood. The human brain's
neural circuits, for example, are just beginning to be mapped by modern neuroscience in the
Human Connectome Project and
CLARITY.
Clinical psychiatry, furthermore, has begun to understand and
acknowledge its current limitations—but further steps by the field are
required to significantly reduce misdiagnosis and
patient harm; this is crucial both for responsible patient care and to retain public trust. Looking forward, a
paradigm shift is needed in psychiatric research to address unanswered questions about schizoaffective disorder. The
dimensional
Research Domain Criteria project currently being developed by the U.S.
National Institutes of Mental Health, may be the specific problem
solving framework psychiatry needs to develop a more scientifically
mature understanding of schizoaffective disorder as well as all other
mental disorders.
Treatment
The
primary treatment of schizoaffective disorder is medication, with
improved outcomes using combined long-term psychological and social
supports. Hospitalization may occur for severe episodes either voluntarily or (if mental health legislation allows it)
involuntarily. Long-term hospitalization is uncommon since
deinstitutionalization beginning in the 1950s, although it still occurs. Community support services including drop-in centers, visits by members of a
community mental health team, supported employment
and support groups are common. Evidence indicates that regular exercise
has a positive effect on the physical and mental health of those with
schizoaffective disorder.
Participating in internet forums is sometimes used by people with
schizoaffective disorder in addition to outpatient medication
treatment.
Therapy
Skillfully
delivered psychosocial treatments are perhaps the most important
component of pushing for and encouraging improved overall functioning in
schizoaffective disorder. Supportive
psychotherapy and
cognitive behavioral therapy are both helpful.
Intensive case management (ICM) has been shown to reduce
hospitalizations, improve adherence to treatment, and improve social
functioning.
With ICM, clients are assigned a case manager responsible for
coordination of care and assisting clients to access supports to address
needs in multiple areas related to well-being, including housing.
High quality psychosocial or
psychiatric rehabilitation is very important for
recovery
from schizoaffective disorder. Psychiatric or psychosocial
rehabilitation focuses on solving community integration problems such as
obtaining and keeping housing and increasing involvement in positive
social groups. It also focuses on improving and increasing
activities of daily living; increasing daily healthy habits (such as normalizing
sleep-wake cycles;
increasing early morning natural light exposure; increasing moderate
exercise [such as 20–30 minutes of moderate to brisk early morning to
pre-afternoon walking daily, in order to help normalize circadian
rhythms]; helping individuals understand the specific benefits of
healthy food choices; increasing stress-reduction activities such as
yoga, tai chi, or meditation); and decreasing unhealthy behaviors (such
as substance abuse and smoking); thereby significantly improving quality
of life. High quality psychiatric rehabilitation may also focus on
vocational rehabilitation
including preparing the client for volunteer, part-time paid work,
returning to school for further education, job skills training for
full-time flexible or supported employment, and other client
self-improvement efforts. Core principles of effective psychiatric
rehabilitation must include providing
hope when the client lacks it,
respect for the client wherever they are in the recovery process,
empowering the client, teaching the client
wellness planning, and emphasizing the importance for the client to develop
social support networks.
A long-term goal of psychiatric and vocational rehabilitation is that
the client learn and actively engage in active stress management while
in education or employment, while receiving treatment.
Psychiatric rehabilitation consists of eight main areas:
- Psychiatric (symptom reduction and management)
- Health and Medical (maintaining consistency of care)
- Housing (safe environments)
- Basic living skills (hygiene, meals [including increasing healthy food intake and reducing processed food intake], safety, planning and chores)
- Social (relationships, family boundaries, communication and integration of client into the community)
- Education and vocation (coping skills, motivation and suitable goals chosen by client)
- Finance (personal budget)
- Community and legal (resources)
Medication
Antipsychotic medication is usually required both for acute treatment and the prevention of relapse. There is no single antipsychotic of choice in treating schizoaffective disorder, but
atypical antipsychotics should be considered because they have mood-stabilizing activity.
Paliperidone is an antipsychotic with FDA approval for the treatment of schizoaffective disorder. Antipsychotics should be used at the minimum dose necessary to control symptoms. Potential side effects include
extrapyramidal symptoms, including
tremor, muscle stiffness, and
restlessness or
akathisia.
Atypical antipsychotics carry a risk of
metabolic syndrome, including weight gain, increased
blood sugar, and increased
blood cholesterol, so regular monitoring of weight and blood work should be carried out. Some atypical antipsychotics, such as
ziprasidone and
aripiprazole, are associated with less risk than others, such as olanzapine. Medication choice is based on how
effectively it reduces symptoms, how few side effects it causes, and cost.
In people with treatment-refractory psychosis, a
clozapine trial should be considered. Clozapine is an
atypical antipsychotic that is recognized as being particularly effective when other antipsychotic agents have failed.
Clozapine should also be considered in people with chronic and
persistent suicidal thinking and behaviour, as it has been shown to
reduce the risk of suicide in patients with schizoaffective disorder and
a history of suicidality. Between 0.5 and 2% of patients taking clozapine may develop a life-threatening complication called
agranulocytosis, which is a significant drop in a type of
white blood cell. Because of this risk, people taking clozapine must have regular monitoring of
blood cell counts.
For depression, if an antidepressant is prescribed,
extra attentiveness must be given
by the prescribing clinician due its risk for long-term mood cycle
acceleration (that is, inducing more frequent episodes of depression per
unit of time) and
medication-induced psychosis or mania. For individuals who show emerging
psychosis,
mania,
mixed episode
symptoms, or mood cycle acceleration, switching to an antipsychotic
plus lithium or lamotrigine is preferable to antidepressants.
Electroconvulsive therapy
Electroconvulsive therapy,
or ECT, may be considered for patients with schizoaffective disorder
experiencing severe depression or severe psychotic symptoms that have
not responded to treatment with antipsychotics.
Epidemiology
Schizoaffective disorder is estimated to occur in 0.5 to 0.8 percent of people at some point in their life. 30% of cases occur between the ages of 25 and 35.
It is more common in women than men; however, this is because of the
high concentration of women in the depressive subcategory, whereas the
bipolar subtype has a more or less even gender distribution.
History
The term
schizoaffective psychosis was introduced by the American psychiatrist
Jacob Kasanin in 1933
[65]
to describe an episodic psychotic illness with predominant affective
symptoms, that was thought at the time to be a good-prognosis
schizophrenia. Kasanin's concept of the illness was influenced by the
psychoanalytic teachings of
Adolf Meyer and Kasanin postulated that
schizoaffective psychosis
was caused by "emotional conflicts" of a "mainly sexual nature" and
that psychoanalysis "would help prevent the recurrence of such attacks." He based his description on a case study of nine individuals.
Other psychiatrists, before and after Kasanin, have made scientific
observations of schizoaffective disorder based on assumptions of a
biological and genetic cause of the illness. In 1863, German
psychiatrist
Karl Kahlbaum (1828–1899) described schizoaffective disorders as a separate group in his
vesania typica circularis. Kahlbaum distinguished between cross-sectional and longitudinal observations. (
Cross-sectional refers to observation of a single, specific episode of the illness, for example, one episode of psychotic depression; while
longitudinal
refers to long-term observation of many distinct episodes [similar or
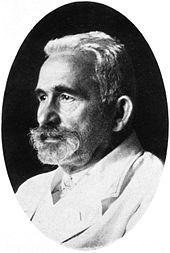
different] often occurring over the span of years.) In 1920,
psychiatrist
Emil Kraepelin
(1856–1926), the founder of contemporary scientific psychiatry,
observed a "great number" of cases that had characteristics of both
groups of psychoses that he originally posited were two distinct and
separate illnesses,
dementia praecox (now called schizophrenia) and
manic depressive insanity (now called bipolar disorders [plural since there are more than one type of bipolar disorder] and recurrent depression).
Kraepelin acknowledged that "there are many overlaps in this area," that is, the area between schizophrenia and mood disorders. In 1959, psychiatrist
Kurt Schneider
(1887–1967) began to further refine conceptualizations of the different
forms that schizoaffective disorders can take since he observed
"concurrent and sequential types". (The
concurrent type
of illness he referred to is a longitudinal course of illness with
episodes of mood disorder and psychosis occurring predominantly at the
same time [now called psychotic mood disorders or affective psychosis];
while his
sequential type refers to a longitudinal course predominantly marked by alternating mood and psychotic episodes.)
Schneider described schizoaffective disorders as "cases in-between" the
traditional Kraepelinian dichotomy of schizophrenia and mood disorders.
The historical clinical observation that schizoaffective disorder
is an overlap of schizophrenia and mood disorders is explained by genes
for both illnesses being present in individuals with schizoaffective
disorder; specifically, recent research shows that schizophrenia and
mood disorders share common genes and polygenic variations.
Schizoaffective disorder was included as a subtype of schizophrenia
in DSM-I and DSM-II, though research showed a schizophrenic cluster of
symptoms in individuals with a family history of mood disorders whose
illness course, other symptoms and treatment outcome were otherwise more
akin to bipolar disorder than to schizophrenia. DSM-III placed
schizoaffective disorder in "Psychotic Disorders Not Otherwise
Specified" before being formally recognized in DSM-III-R. DSM-III-R included its own diagnostic criteria as well as the subtypes, bipolar and depressive.
In DSM-IV, published in 1994, schizoaffective disorders belonged to the
category "Other Psychotic Disorders" and included almost the same
criteria and the same subtypes of illness as DSM-III-R, with the
addition of mixed bipolar symptomatology.
DSM-IV and DSM-IV-TR (published in 2000) criteria for schizoaffective disorder were poorly defined and poorly
operationalized. These
ambiguous and unreliable criteria lasted 19 years and led clinicians to significantly overuse the schizoaffective disorder diagnosis.
Patients commonly diagnosed with DSM-IV schizoaffective disorder showed
a clinical picture at time of diagnosis that appeared different from
schizophrenia or psychotic mood disorders using DSM-IV criteria, but who
as a group, were
longitudinally determined to have outcomes indistinguishable from those with mood disorders with or without psychotic features. A poor prognosis was assumed to apply to these patients by most clinicians, and this poor prognosis was
harmful to many patients. The poor prognosis for DSM-IV schizoaffective disorder was not based on
patient outcomes research, but was caused by poorly defined criteria interacting with clinical tradition and belief; clinician
enculturation with
unscientific assumptions from the diagnosis' history (discussed above), including the invalid Kraepelinian dichotomy; and by clinicians being unfamiliar with the
scientific limitations of the diagnostic and classification system.
The DSM-5 schizoaffective disorder workgroup analyzed all of the available research
evidence
on schizoaffective disorder, and concluded that "presenting symptoms of
psychosis have little validity in determining diagnosis, prognosis, or
treatment response."
Given our understanding of overlapping genetics in bipolar disorders,
schizoaffective disorder, and schizophrenia, as well as the overlap in
treatments for these disorders; but given the lack of specificity of
presenting symptoms for determining diagnosis, prognosis or treatment
response in these psychotic illness
syndromes, the limits of our knowledge are clearer:
Presenting symptoms of psychosis describe only presenting symptoms to be treated, and not much more. Schizoaffective disorder was changed to a longitudinal or life course diagnosis in DSM-5 for this reason.
Research
Evidence
is lacking about schizoaffective disorder's (likely multiple) causes
and mechanisms (knowing these leads to specific and consistently
effective treatments), and about how exactly mood episodes and psychosis
are related (knowing this may lead to a simpler, clearer, and more
usable behavioral definition of the disorder; as well as a better
diagnostic system).
Whether schizoaffective disorder is a variant of schizophrenia (as in
DSM-5 and ICD-10 classification systems), a variant of bipolar disorder,
or part of a dimensional continuum between
psychotic depression, bipolar disorders and schizophrenia is currently being investigated.
Research into the assessment and treatment of schizoaffective disorder will rely less on
DSM and
ICD criteria as time progresses, and more on the
dimensional Research Domain Criteria currently being developed by the U.S.
National Institute of Mental Health
(NIMH). The Research Domain Criteria initiative, led by Bruce Cuthbert,
Ph.D., of NIMH, is the inspiration for the Roadmap for Mental Health
Research in Europe (ROAMER).
The purpose of the Research Domain Criteria initiative is to address
the marked variability and overlap within and among the disorder
categories, and to foster development of more effective assessment and
treatment for each individual patient.
Over the coming decades, advances resulting from the Research Domain
Criteria in the U.S. and ROAMER in Europe will be incorporated into
future versions of the
DSM and
ICD, with the hope of eventually leading to
personalized mental health
of greater diagnostic accuracy and with more targeted and useful
treatments, including biomedical, psychosocial, and possibly preventive
approaches.