 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌmɛləˈtoʊnɪn/ ( |
| Trade names | Circadin, Slenyto, others |
| Other names | N-acetyl-5-methoxy tryptamine |
| AHFS/Drugs.com | Consumer Drug Information |
| License data | |
| Routes of administration | By mouth, sublingual, transdermal |
| ATC code | |
| Physiological data | |
| Source tissues | pineal gland |
| Target tissues | wide spread, including brain, retina, and circulatory system |
| Receptors | melatonin receptor |
| Precursor | N-acetylserotonin |
| Metabolism | Liver via CYP1A2 mediated 6-hydroxylation |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 30–50% |
| Metabolism | Liver via CYP1A2 mediated 6-hydroxylation |
| Metabolites | 6-hydroxymelatonin, N-acetyl-5lhydroxytryptamine, 5-methoxytryptamine |
| Elimination half-life | 30–50 minutes |
| Excretion | Kidney |
| Identifiers | |
| CAS Number | |
|---|---|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.725 |
| Chemical and physical data | |
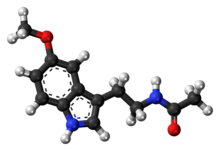
| Formula | C13H16N2O2 |
| Molar mass | 232.283 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 117 °C (243 °F) |
Melatonin is a hormone primarily released by the pineal gland at night, and has long been associated with control of the sleep–wake cycle. As a dietary supplement, it is often used for the short-term treatment of insomnia, such as from jet lag or shift work, and is typically taken by mouth. Evidence of its benefit for this use, however, is not strong. A 2017 review found that sleep onset occurred six minutes faster with use, but found no change in total time asleep. The melatonin receptor agonist medication ramelteon may work as well as melatonin supplements, at greater cost but with different adverse effects, for some sleep conditions.
Side effects from melatonin supplements are minimal at low doses for short durations. They may include somnolence (sleepiness), headaches, nausea, diarrhea, abnormal dreams, irritability, nervousness, restlessness, insomnia, anxiety, migraine, lethargy, psychomotor hyperactivity, dizziness, hypertension, abdominal pain, heartburn, mouth ulcers, dry mouth, hyperbilirubinaemia, dermatitis, night sweats, pruritus, rash, dry skin, pain in the extremities, symptoms of menopause, chest pain, glycosuria (sugar in the urine), proteinuria (protein in the urine), abnormal liver function tests, increased weight, tiredness, mood swings, aggression and feeling hungover. Its use is not recommended during pregnancy or breastfeeding or for those with liver disease.
In vertebrates, melatonin is involved in synchronizing circadian rhythms, including sleep–wake timing and blood pressure regulation, and in control of seasonal rhythmicity including reproduction, fattening, moulting and hibernation. Many of its effects are through activation of the melatonin receptors, while others are due to its role as an antioxidant. In plants, it functions to defend against oxidative stress. It is also present in various foods.
Melatonin was discovered in 1958. It is sold over the counter in Canada and the United States; in the United Kingdom, it is a prescription-only medication. It is not approved by the US Food and Drug Administration (FDA) for any medical use. In Australia and the European Union, it is indicated for difficulty sleeping in people over the age of 54. In the European Union, it is indicated for the treatment of insomnia in children and adolescents. It was approved for medical use in the European Union in 2007.
Medical uses
In the European Union it is indicated for the treatment of insomnia in children and adolescents aged 2–18 with autism spectrum disorder (ASD) and / or Smith–Magenis syndrome, where sleep hygiene measures have been insufficient and for monotherapy for the short-term treatment of primary insomnia characterized by poor quality of sleep in people who are aged 55 or over.
Sleep disorders
Positions on the benefits of melatonin for insomnia are mixed. A review by the Agency for Healthcare Research and Quality (AHRQ) from 2015 stated that evidence of benefit in the general population was unclear. A review from 2017, found a modest effect on time until onset of sleep. Another review from 2017 put this decrease at six minutes to sleep onset but found no difference in total sleep time.
Melatonin may also be useful in delayed sleep phase syndrome. Melatonin appears to work as well as ramelteon but costs less.
Melatonin is a safer alternative than clonazepam in the treatment of REM sleep behavior disorder – a condition associated with the synucleinopathies like Parkinson's disease and dementia with Lewy bodies. In Europe it is used for short-term treatment of insomnia in people who are 55 years old or older. It is deemed to be a first line agent in this group.
Melatonin reduces the time until onset of sleep and increases sleep duration in children with neurodevelopmental disorders.
Dementia
A 2020 Cochrane review found no evidence that melatonin helped sleep problems in people with moderate to severe dementia due to Alzheimer's disease. A 2019 review found that while melatonin may improve sleep in minimal cognitive impairment, after the onset of Alzheimer's it has little to no effect. Melatonin may, however, help with sundowning.
Jet lag and shift work
Melatonin is known to reduce jet lag, especially in eastward travel. If the time it is taken is not correct, however, it can instead delay adaptation.
Melatonin appears to have limited use against the sleep problems of people who work shift work. Tentative evidence suggests that it increases the length of time people are able to sleep.
Adverse effects
Melatonin appears to cause very few side effects as tested in the short term, up to three months, at low doses. Two systematic reviews found no adverse effects of exogenous melatonin in several clinical trials and comparative trials found the adverse effects headaches, dizziness, nausea, and drowsiness were reported about equally for both melatonin and placebo. Prolonged-release melatonin is safe with long-term use of up to 12 months. Although not recommended for long term use beyond this, low-dose melatonin is generally safer, and a better alternative, than many prescription and over the counter sleep aids if a sleeping medication must be used for an extended period of time. Low-doses of melatonin are usually sufficient to produce a hypnotic effect in most people. Higher doses do not appear to result in a stronger effect, but instead appear to cause drowsiness for a longer period of time.
There is emerging evidence that the timing of taking exogenous melatonin in relation to food is also an important factor. Specifically, taking exogenous melatonin shortly after a meal is correlated with impaired glucose tolerance. Therefore, Rubio-Sastre and colleagues recommend waiting at least 2 hours after the last meal before taking a melatonin supplement.
Melatonin can cause nausea, next-day grogginess, and irritability. In the elderly, it can cause reduced blood flow and hypothermia. In autoimmune disorders, evidence is conflicting whether melatonin supplementation may ameliorate or exacerbate symptoms due to immunomodulation.
Melatonin can lower follicle-stimulating hormone levels. Melatonin's effects on human reproduction remain unclear.
In those taking warfarin, some evidence suggests there may exist a potentiating drug interaction, increasing the anticoagulant effect of warfarin and the risk of bleeding.
Functions
Circadian rhythm
In animals, melatonin plays an important role in the regulation of sleep–wake cycles. Human infants' melatonin levels become regular in about the third month after birth, with the highest levels measured between midnight and 8:00 am. Human melatonin production decreases as a person ages. Also, as children become teenagers, the nightly schedule of melatonin release is delayed, leading to later sleeping and waking times.
Antioxidant
Melatonin was first reported as a potent antioxidant and free radical scavenger in 1993. In vitro, melatonin acts as a direct scavenger of oxygen radicals and reactive nitrogen species including OH•, O2−•, and NO•. In plants, melatonin works with other antioxidants to improve the overall effectiveness of each antioxidant. Melatonin has been proven to be twice as active as vitamin E, believed to be the most effective lipophilic antioxidant. Via signal transduction through melatonin receptors, melatonin promotes the expression of antioxidant enzymes such as superoxide dismutase, glutathione peroxidase, glutathione reductase, and catalase.
Melatonin occurs at high concentrations within mitochondrial fluid which greatly exceed the plasma concentration of melatonin. Due to its capacity for free radical scavenging, indirect effects on the expression of antioxidant enzymes, and its significant concentrations within mitochondria, a number of authors have indicated that melatonin has an important physiological function as a mitochondrial antioxidant.
The melatonin metabolites produced via the reaction of melatonin with reactive oxygen species or reactive nitrogen species also react with and reduce free radicals. Melatonin metabolites generated from redox reactions include cyclic 3-hydroxymelatonin, N1-acetyl-N2-formyl-5-methoxykynuramine (AFMK), and N1-acetyl-5-methoxykynuramine (AMK).
Immune system
While it is known that melatonin interacts with the immune system, the details of those interactions are unclear. An antiinflammatory effect seems to be the most relevant. There have been few trials designed to judge the effectiveness of melatonin in disease treatment. Most existing data are based on small, incomplete trials. Any positive immunological effect is thought to be the result of melatonin acting on high-affinity receptors (MT1 and MT2) expressed in immunocompetent cells. In preclinical studies, melatonin may enhance cytokine production, and by doing this, counteract acquired immunodeficiences. Some studies also suggest that melatonin might be useful fighting infectious disease including viral, such as HIV, and bacterial infections, and potentially in the treatment of cancer.
Biosynthesis
In animals, biosynthesis of melatonin occurs through hydroxylation, decarboxylation, acetylation and a methylation starting with L-tryptophan. L-tryptophan is produced in the shikimate pathway from chorismate or is acquired from protein catabolism. First L-tryptophan is hydroxylated on the indole ring by tryptophan hydroxylase to produce 5-hydroxytryptophan. This intermediate (5-HTP) is decarboxylated by pyridoxal phosphate and 5-hydroxytryptophan decarboxylase to produce serotonin.
Serotonin is itself an important neurotransmitter, but is also converted into N-acetylserotonin by serotonin N-acetyltransferase with acetyl-CoA. Hydroxyindole O-methyltransferase and S-adenosyl methionine convert N-acetylserotonin into melatonin through methylation of the hydroxyl group.
In bacteria, protists, fungi, and plants, melatonin is synthesized indirectly with tryptophan as an intermediate product of the shikimate pathway. In these cells, synthesis starts with D-erythrose 4-phosphate and phosphoenolpyruvate, and in photosynthetic cells with carbon dioxide. The rest of the synthesising reactions are similar, but with slight variations in the last two enzymes.
It has been hypothesized that melatonin is made in the mitochondria and chloroplasts.
Mechanism
In order to hydroxylate L-tryptophan, the cofactor tetrahydrobiopterin (THB) must first react with oxygen and the active site iron of tryptophan hydroxylase. This mechanism is not well understood, but two mechanisms have been proposed:
1. A slow transfer of one electron from the THB to O2 could produce a superoxide which could recombine with the THB radical to give 4a-peroxypterin. 4a-peroxypterin could then react with the active site iron (II) to form an iron-peroxypterin intermediate or directly transfer an oxygen atom to the iron.
2. O2 could react with the active site iron (II) first, producing iron (III) superoxide which could then react with the THB to form an iron-peroxypterin intermediate.
Iron (IV) oxide from the iron-peroxypterin intermediate is selectively attacked by a double bond to give a carbocation at the C5 position of the indole ring. A 1,2-shift of the hydrogen and then a loss of one of the two hydrogen atoms on C5 reestablishes aromaticity to furnish 5-hydroxy-L-tryptophan.
A decarboxylase with cofactor pyridoxal phosphate (PLP) removes CO2 from 5-hydroxy-L-tryptophan to produce 5-hydroxytryptamine. PLP forms an imine with the amino acid derivative. The amine on the pyridine is protonated and acts as an electron sink, enabling the breaking of the C-C bond and releasing CO2. Protonation of the amine from tryptophan restores the aromaticity of the pyridine ring and then imine is hydrolyzed to produce 5-hydroxytryptamine and PLP.
It has been proposed that histidine residue His122 of serotonin N-acetyl transferase is the catalytic residue that deprotonates the primary amine of 5-hydroxytryptamine, which allows the lone pair on the amine to attack acetyl-CoA, forming a tetrahedral intermediate. The thiol from coenzyme A serves as a good leaving group when attacked by a general base to give N-acetylserotonin.
N-acetylserotonin is methylated at the hydroxyl position by S-adenosyl methionine (SAM) to produce S-adenosyl homocysteine (SAH) and melatonin.
Regulation
In vertebrates, melatonin secretion is regulated by activation of the beta-1 adrenergic receptor by norepinephrine. Norepinephrine elevates the intracellular cAMP concentration via beta-adrenergic receptors and activates the cAMP-dependent protein kinase A (PKA). PKA phosphorylates the penultimate enzyme, the arylalkylamine N-acetyltransferase (AANAT). On exposure to (day)light, noradrenergic stimulation stops and the protein is immediately destroyed by proteasomal proteolysis. Production of melatonin is again started in the evening at the point called the dim-light melatonin onset.
Blue light, principally around 460–480 nm, suppresses melatonin biosynthesis, proportional to the light intensity and length of exposure. Until recent history, humans in temperate climates were exposed to few hours of (blue) daylight in the winter; their fires gave predominantly yellow light. The incandescent light bulb widely used in the 20th century produced relatively little blue light. Light containing only wavelengths greater than 530 nm does not suppress melatonin in bright-light conditions. Wearing glasses that block blue light in the hours before bedtime may decrease melatonin loss. Use of blue-blocking goggles the last hours before bedtime has also been advised for people who need to adjust to an earlier bedtime, as melatonin promotes sleepiness.
Pharmacology
Pharmacodynamics
In humans, melatonin is a full agonist of melatonin receptor 1 (picomolar binding affinity) and melatonin receptor 2 (nanomolar binding affinity), both of which belong to the class of G-protein coupled receptors (GPCRs). Melatonin receptors 1 and 2 are both Gi/o-coupled GPCRs, although melatonin receptor 1 is also Gq-coupled. Melatonin also acts as a high-capacity free radical scavenger within mitochondria which also promotes the expression of antioxidant enzymes such as superoxide dismutase, glutathione peroxidase, glutathione reductase, and catalase via signal transduction through melatonin receptors.
Pharmacokinetics
When used several hours before sleep according to the phase response curve for melatonin in humans, small amounts (0.3 mg) of melatonin shift the circadian clock earlier, thus promoting earlier sleep onset and morning awakening. Melatonin is rapidly absorbed and distributed, reaching peak plasma concentrations after 60 minutes of administration, and is then eliminated. Melatonin has a half life of 35–50 minutes. In humans, 90% of orally administered exogenous melatonin is cleared in a single passage through the liver, a small amount is excreted in urine, and a small amount is found in saliva. The bioavalibility of melatonin is between 10 and 50%.
Melatonin is metabolized in the liver by cytochrome P450 enzyme CYP1A2 to 6-hydroxymelatonin. Metabolites are conjugated with sulfuric acid or glucuronic acid for excretion in the urine. 5% of melatonin is excreted in the urine as the unchanged drug.
Some of the metabolites formed via the reaction of melatonin with a free radical include cyclic 3-hydroxymelatonin, N1-acetyl-N2-formyl-5-methoxykynuramine (AFMK), and N1-acetyl-5-methoxykynuramine (AMK).
The membrane transport proteins that move melatonin across a membrane include, but are not limited to, glucose transporters, including GLUT1, and the proton-driven oligopeptide transporters PEPT1 and PEPT2.
For research as well as clinical purposes, melatonin concentration in humans can be measured either from the saliva or blood plasma.
History
Melatonin was first discovered in connection to the mechanism by which some amphibians and reptiles change the color of their skin. As early as 1917, Carey Pratt McCord and Floyd P. Allen discovered that feeding extract of the pineal glands of cows lightened tadpole skin by contracting the dark epidermal melanophores.
In 1958, dermatology professor Aaron B. Lerner and colleagues at Yale University, in the hope that a substance from the pineal might be useful in treating skin diseases, isolated the hormone from bovine pineal gland extracts and named it melatonin. In the mid-70s Lynch et al. demonstrated that the production of melatonin exhibits a circadian rhythm in human pineal glands.
The discovery that melatonin is an antioxidant was made in 1993. The first patent for its use as a low-dose sleep aid was granted to Richard Wurtman at MIT in 1995. Around the same time, the hormone got a lot of press as a possible treatment for many illnesses. The New England Journal of Medicine editorialized in 2000: "With these recent careful and precise observations in blind persons, the true potential of melatonin is becoming evident, and the importance of the timing of treatment is becoming clear."
It was approved for medical use in the European Union in 2007.
Other animals
In vertebrates, melatonin is produced in darkness, thus usually at night, by the pineal gland, a small endocrine gland located in the center of the brain but outside the blood–brain barrier. Light/dark information reaches the suprachiasmatic nuclei from retinal photosensitive ganglion cells of the eyes rather than the melatonin signal (as was once postulated). Known as "the hormone of darkness", the onset of melatonin at dusk promotes activity in nocturnal (night-active) animals and sleep in diurnal ones including humans.
Many animals use the variation in duration of melatonin production each day as a seasonal clock. In animals including humans, the profile of melatonin synthesis and secretion is affected by the variable duration of night in summer as compared to winter. The change in duration of secretion thus serves as a biological signal for the organization of daylength-dependent (photoperiodic) seasonal functions such as reproduction, behavior, coat growth, and camouflage coloring in seasonal animals. In seasonal breeders that do not have long gestation periods and that mate during longer daylight hours, the melatonin signal controls the seasonal variation in their sexual physiology, and similar physiological effects can be induced by exogenous melatonin in animals including mynah birds and hamsters. Melatonin can suppress libido by inhibiting secretion of luteinizing hormone and follicle-stimulating hormone from the anterior pituitary gland, especially in mammals that have a breeding season when daylight hours are long. The reproduction of long-day breeders is repressed by melatonin and the reproduction of short-day breeders is stimulated by melatonin.
During the night, melatonin regulates leptin, lowering its levels.
Cetaceans have lost all the genes for melatonin synthesis as well as those for melatonin receptors. This is thought to be related to their unihemispheric sleep pattern (one brain hemisphere at a time). Similar trends have been found in sirenians.
Plants
Until its identification in plants in 1987, melatonin was for decades thought to be primarily an animal neurohormone. When melatonin was identified in coffee extracts in the 1970s, it was believed to be a byproduct of the extraction process. Subsequently, however, melatonin has been found in all plants that have been investigated. It is present in all the different parts of plants, including leaves, stems, roots, fruits, and seeds, in varying proportions. Melatonin concentrations differ not only among plant species, but also between varieties of the same species depending on the agronomic growing conditions, varying from picograms to several micrograms per gram. Notably high melatonin concentrations have been measured in popular beverages such as coffee, tea, wine, and beer, and crops including corn, rice, wheat, barley, and oats. In some common foods and beverages, including coffee and walnuts, the concentration of melatonin has been estimated or measured to be sufficiently high to raise the blood level of melatonin above daytime baseline values.
Although a role for melatonin as a plant hormone has not been clearly established, its involvement in processes such as growth and photosynthesis is well established. Only limited evidence of endogenous circadian rhythms in melatonin levels has been demonstrated in some plant species and no membrane-bound receptors analogous to those known in animals have been described. Rather, melatonin performs important roles in plants as a growth regulator, as well as environmental stress protector. It is synthesized in plants when they are exposed to both biological stresses, for example, fungal infection, and nonbiological stresses such as extremes of temperature, toxins, increased soil salinity, drought, etc.
Occurrence
Dietary supplement
Melatonin is categorized by the US Food and Drug Administration (FDA) as a dietary supplement, and is sold over-the-counter in both the US and Canada. FDA regulations applying to medications are not applicable to melatonin, though the FDA has found false claims that it cures cancer. As melatonin may cause harm in combination with certain medications or in the case of certain disorders, a doctor or pharmacist should be consulted before making a decision to take melatonin. In many countries, melatonin is recognized as a neurohormone and it cannot be sold over-the-counter. According to Harriet Hall caution is advisable, since quality control is a documented problem. 71% of products did not contain within 10% of the labelled amount of melatonin, with variations ranging from -83% to +478%, lot-to-lot variability was as high as 465%, and the discrepancies were not correlated to any manufacturer or product type. To make matters worse, 8 out of 31 products were contaminated with the neurotransmitter serotonin.
Food products
Naturally-occurring melatonin has been reported in foods including tart cherries to about 0.17–13.46 ng/g, bananas and grapes, rice and cereals, herbs, plums, olive oil, wine and beer. When birds ingest melatonin-rich plant feed, such as rice, the melatonin binds to melatonin receptors in their brains. When humans consume foods rich in melatonin, such as banana, pineapple, and orange, the blood levels of melatonin increase significantly.
Beverages and snacks containing melatonin were being sold in grocery stores, convenience stores, and clubs in May 2011. The FDA considered whether these food products could continue to be sold with the label "dietary supplements". On 13 January 2010, it issued a Warning Letter to Innovative Beverage, creators of several beverages marketed as drinks, stating that melatonin, while legal as a dietary supplement, was not approved as a food additive. A different company selling a melatonin-containing beverage received a warning letter in 2015.
Commercial availability
Immediate-release melatonin is not tightly regulated in countries where it is available as an over-the-counter medication. It is available in doses from 0.3 mg 10 mg or more, it is even possible to buy raw melatonin powder by lbs. Immediate-release formulations cause blood levels of melatonin to reach their peak in about an hour. The hormone may be administered orally, as capsules, gummies, tablets, or liquids. It is also available for use sublingually, or as transdermal patches.
Formerly, melatonin was derived from animal pineal tissue, such as bovine. It is now synthetic, which limits the risk of contamination or the means of transmitting infectious material.
Melatonin is the most popular over-the-counter sleep remedy in the US, resulting in sales in excess of US$400 million during 2017.
Research
Various uses and effects of melatonin have been studied. A 2015 review of studies of melatonin in tinnitus found the quality of evidence low, but not entirely without promise.
Headaches
Tentative evidence shows melatonin may help reduce some types of headaches including cluster and hypnic headaches.
Cancer
A 2013 review by the National Cancer Institutes found evidence for use to be inconclusive. A 2005 review of unblinded clinical trials found a reduced rate of death, but that blinded and independently conducted randomized controlled trials are needed.
Protection from radiation
Both animal and human studies have shown melatonin to protect against radiation-induced cellular damage. Melatonin and its metabolites protect organisms from oxidative stress by scavenging reactive oxygen species which are generated during exposure. Nearly 70% of biological damage caused by ionizing radiation is estimated to be attributable to the creation of free radicals, especially the hydroxyl radical that attacks DNA, proteins, and cellular membranes. Melatonin has been described as a broadly protective, readily available, and orally self-administered antioxidant that is without known, major side effects.
Epilepsy
A 2016 review found no beneficial role of melatonin in reducing seizure frequency or improving quality of life in people with epilepsy.
Secondary dysmenorrhoea
A 2016 review suggested no strong evidence of melatonin compared to placebo for dysmenorrhoea secondary to endometriosis.
Delirium
A 2016 review suggested no clear evidence of melatonin to reduce the incidence of delirium.
Gastroesophageal reflux disease
A 2011 review said melatonin is effective in relieving epigastric pain and heartburn.
Psychiatry
Melatonin might improve sleep in people with autism. Children with autism have abnormal melatonin pathways and below-average physiological levels of melatonin. Melatonin supplementation has been shown to improve sleep duration, sleep onset latency, and night-time awakenings. However, many studies on melatonin and autism rely on self-reported levels of improvement and more rigorous research is needed.
While the packaging of melatonin often warns against use in people under 18 years of age, studies suggest that melatonin is an efficacious and safe treatment for insomnia in people with ADHD, including children. However, larger and longer studies are needed to establish long-term safety and optimal dosing.
Melatonin in comparison to placebo is effective for reducing preoperative anxiety in adults when given as premedication. It may be just as effective as standard treatment with benzodiazepine in reducing preoperative anxiety. Melatonin may also reduce postoperative anxiety (measured 6 hours after surgery) when compared to placebo.
Some supplemental melatonin users report an increase in vivid dreaming. Extremely high doses of melatonin increased REM sleep time and dream activity in people both with and without narcolepsy. Some evidence supports an antidepressant effect.




