From Wikipedia, the free encyclopedia
| Acupuncture | |
|---|---|
| Intervention | |

Needles being inserted into a person's skin
|
|
| ICD-10-PCS | 8E0H30Z |
| ICD-9: | 99.91-99.92 |
| MeSH | D015670 |
| OPS-301 code: | 8-975.2 |
Acupuncture (from Latin, 'acus' (needle) + 'punctura' (to puncture)[1]) is the stimulation of specific
acupuncture points along the skin of the body using thin needles.[2] It can be associated with the application of heat, pressure, or laser light to these same points.[2] Clinical practice varies depending on the country.[3] Traditional acupuncture involves needle insertion, moxibustion, and cupping therapy.[4] It is a form of alternative medicine[5] and a key component of traditional Chinese medicine (TCM).[6] According to TCM, stimulating specific acupuncture points corrects imbalances in the flow of qi through channels known as meridians.[7] TCM theory and practice are not based upon scientific knowledge.[7] Acupuncture aims to treat a range of conditions,[6] though it is most commonly used for pain relief.[8][9] It is rarely used alone but rather as an adjunct to other forms of treatment.[10]
Evidence on the effectiveness of acupuncture is "variable and inconsistent, even for single conditions".[11] An overview of high-quality Cochrane reviews suggested that acupuncture may alleviate some, but not all, kinds of pain.[12] A systematic review of systematic reviews found that for reducing pain, real acupuncture was no better than sham acupuncture and concluded that there is little evidence that acupuncture is an effective treatment for reducing pain.[n 1][8] Although minimally invasive, the puncturing of the skin with acupuncture needles poses problems when designing trials that adequately control for placebo effects.[14][15] Some research results suggest acupuncture can alleviate pain, though other research consistently suggests that acupuncture's effects are mainly due to placebo.[3] The evidence suggests that short-term treatment with acupuncture does not produce long-term benefits.[16] A systematic review concluded that the analgesic effect of acupuncture seemed to lack clinical relevance and could not be clearly distinguished from bias.[17]
Acupuncture is generally safe when done by an appropriately trained practitioner using clean technique and single-use needles.[4][18] When properly delivered, it has a low rate of mostly minor adverse effects.[2][4] Between 2000 and 2009, at least ninety-five cases of serious adverse events, including five deaths, were reported to have resulted from acupuncture.[8] Many of these cases occurred in developed countries and many were due to malpractice.[8] The most frequently reported adverse events were pneumothorax and infections.[8] Since serious adverse events continue to be reported, it is recommended that acupuncturists be trained sufficiently to reduce the risk.[8] A meta-analysis found that acupuncture for chronic low back pain was cost-effective as an adjunct to standard care, but not as a substitute for standard care except in cases where comorbid depression presented,[19] while a systematic review found insufficient evidence for the cost-effectiveness of acupuncture in the treatment of chronic low back pain.[20]
Acupuncture has been the subject of active scientific research, both in regard to its basis and therapeutic effectiveness, since the late 20th century.[14] Scientific investigation has not found any histological or physiological evidence for traditional Chinese concepts such as qi, meridians, and acupuncture points.[n 2][24][25] In response, some contemporary practitioners use acupuncture without following the traditional Chinese approach[26][27] and have abandoned the concepts of qi and meridians as pseudoscientific.[28][29] A Nature editorial described TCM as "fraught with pseudoscience", and said that the most obvious reason why it hasn't delivered many cures is that the majority of its treatments have no logical mechanism of action.[30] Acupuncture is currently used widely throughout China and many other countries, including the United States.[4][31] It is uncertain exactly when acupuncture originated or how it evolved, but it is generally thought to derive from ancient China.[32] In Chinese history the introduction of acupuncture is attributed to the emperor Shennong.[33] Hieroglyphs and pictographs have been found dating from the Shang Dynasty (1600–1100 BCE) that suggest acupuncture along with moxibustion was in practice.[34]
Clinical practice
Acupuncture is the stimulation of defined, specific acupuncture points along the skin of the body using thin needles.[2] It can be associated with the application of heat, pressure, or laser light to these same points.[2] Classically, acupuncture is individualized and based on philosophy and intuition, and not on scientific research.[35] In modern acupuncture, a consultation is followed by taking the pulse on both arms and inspecting the tongue. This initial evaluation may last up to 60 minutes.[36] Subsequent visits typically last about a half an hour.[36] The number and frequency of acupuncture sessions vary, but most practitioners do not think one session is sufficient.[5] A common treatment plan for a single complaint usually involves six to twelve treatments, to be carried out over a few months.[36] A typical session entails lying still while approximately five to twenty needles are inserted; for the majority of cases, the needles will be left in place for ten to twenty minutes.[36]
Clinical practice varies depending on the country.[3][37] A comparison of the average number of patients treated per hour found significant differences between China (10) and the United States (1.2).[38] Traditional acupuncture involves needle insertion, moxibustion, and cupping therapy.[4] Traditional acupuncture may be accompanied by various ancillary procedures, such as palpation of the radial artery and other parts of the body and examining the tongue.[5] Acupuncturists generally practice acupuncture as an overall system of care, which includes using traditional diagnostic techniques, acupuncture needling, and other adjunctive treatments.[39] Chinese herbs are also often used.[39] Although various different techniques of acupuncture practice have emerged, the method used in traditional Chinese medicine (TCM) seems to be the most widely adopted in the US.[5] The main methods practiced in the UK are TCM and Western medical acupuncture.[40]
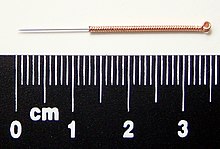
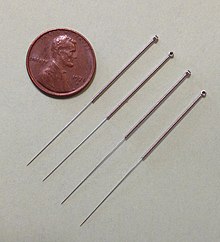
Needles
Acupuncture needles are typically made of stainless steel, making them flexible and preventing them from rusting or breaking.[41] Needles are usually disposed of after each use to prevent contamination.[41] Reusable needles can used as well and should be sterilized between uses.[41][42] Needles vary in length between 13 to 130 millimetres (0.51 to 5.12 in), with shorter needles used near the face and eyes, and longer needles in more fleshy areas; needle diameters vary from 0.16 mm (0.006 in) to 0.46 mm (0.018 in),[43] with thicker needles used on more robust patients. Thinner needles may be flexible and require tubes for insertion. The tip of the needle should not be made too sharp to prevent breakage, although blunt needles cause more pain.[44]
Apart from the usual filiform needle, other needle types include three-edged needles and the Nine Ancient Needles.[43] Japanese acupuncturists use extremely thin needles that are used superficially, sometimes without penetrating the skin, and surrounded by a guide tube (a 17th-century invention adopted in China and the West). Korean acupuncture uses copper needles and has a greater focus on the hand.[37]
Needling technique
Insertion
The skin is sterilized and the needles are inserted, frequently with a plastic guide tube. Needles may be manipulated in various ways, including spinning, flicking, or moving up and down relative to the skin. Since most pain is felt in the superficial layers of the skin, a quick insertion of the needle is recommended.[45] Often, the needles are stimulated by hand in order to cause a dull, localized, aching sensation that is called de qi, as well as "needle grasp," a tugging feeling felt by the acupuncturist and generated by a mechanical interaction between the needle and skin.[5] Acupuncture can be painful.[46] The skill level of the acupuncturist may influence how painful the needle insertion is, and a sufficiently skilled practitioner may be able to insert the needles without causing any pain.[45]De-qi sensation
De-qi (Chinese: 得气; pinyin: dé qì; "arrival of qi") refers to a sensation of numbness, distension, or electrical tingling at the needling site which might radiate along the corresponding meridian. If de-qi can not be generated, then inaccurate location of the acupoint, improper depth of needle insertion, inadequate manual manipulation, or a very weak constitution of the patient have to be considered, all of which are thought to decrease the likelihood of successful treatment. If the de-qi sensation doesn't immediately occur upon needle insertion, various manual manipulation techniques can be applied to promote it (such as "plucking", "shaking" or "trembling").[47]Once de-qi is achieved, further techniques might be utilized which aim to "influence" the de-qi; for example, by certain manipulation the de-qi sensation allegedly can be conducted from the needling site towards more distant sites of the body. Other techniques aim at "tonifying" (Chinese: 补; pinyin: bǔ) or "sedating" (Chinese: 泄; pinyin: xiè) qi.[47] The former techniques are used in deficiency patterns, the latter in excess patterns.[47]
De qi is more important in Chinese acupuncture, while Western and Japanese patients may not consider it a necessary part of the treatment.[37]
Non-invasive needling
There is also a non-invasive therapy developed in early 20th century Japan using an elaborate set of "needles" for the treatment of children (shōnishin or shōnihari).[48][49]Related practices
Acupressure, a non-invasive form of acupuncture, uses physical pressure applied to acupressure points by the hand, elbow, or with various devices.[51] Acupuncture is often accompanied by moxibustion, the burning of cone-shaped preparations of moxa (made from dried mugwort) on or near the skin, often but not always near or on an acupuncture point. Traditionally, acupuncture was used to treat acute conditions while moxibustion was used for chronic diseases. Moxibustion could be direct (the cone was placed directly on the skin and allowed to burn the skin producing a blister and eventually a scar), or indirect (either a cone of moxa was placed on a slice of garlic, ginger or other vegetable, or a cylinder of moxa was held above the skin, close enough to either warm or burn it).[52]
Cupping therapy is an ancient Chinese form of alternative medicine in which a local suction is created on the skin; practitioners believe this mobilizes blood flow in order to promote healing.[53] Tui na is a TCM method of attempting to stimulate the flow of qi by various bare-handed techniques that do not involve needles.[54] Electroacupuncture is a form of acupuncture in which acupuncture needles are attached to a device that generates continuous electric pulses (this has been described as "essentially transdermal electrical nerve stimulation [TENS] masquerading as acupuncture").[11] Sonopuncture is a stimulation of the body similar to acupuncture using sound instead of needles.[55] This may be done using purpose-built transducers to direct a narrow ultrasound beam to a depth of 6–8 centimetres at acupuncture meridian points on the body.[56] Alternatively, tuning forks or other sound emitting devices are used.[57] Acupuncture point injection is the injection of various substances (such as drugs, vitamins or herbal extracts) into acupoints.[58] Auriculotherapy, commonly known as ear acupuncture, auricular acupuncture, or auriculoacupuncture, is considered to date back to ancient China which involves inserting needles to stimulate points on the outer ear.[59] The modern approach was developed in France during the early 1950s.[59] There is no scientific evidence that it can cure disease; the evidence of effectiveness is negligible.[59] Scalp acupuncture, developed in Japan, is based on reflexological considerations regarding the scalp area. Hand acupuncture, developed in Korea, centers around assumed reflex zones of the hand. Medical acupuncture attempts to integrate reflexological concepts, the trigger point model, and anatomical insights (such as dermatome distribution) into acupuncture practice, and emphasizes a more formulaic approach to acupuncture point location.[60] Cosmetic acupuncture is the use of acupuncture in an attempt to reduce wrinkles on the face.[61] Veterinary acupuncture is performed on animals; evidence is sparse.[62]
Effectiveness
The application of evidence-based medicine to researching acupuncture's effectiveness is a controversial activity, and has produced different results in a growing evidence base of research.[14]Some research results suggest acupuncture can alleviate pain but others consistently suggest that acupuncture's effects are mainly due to placebo.[3] It is difficult but not impossible to design rigorous research trials for acupuncture.[63][64] Due to acupuncture's invasive nature, one of the major challenges in efficacy research is in the design of an appropriate placebo control group.[14][15] For efficacy studies to determine whether acupuncture has specific effects, "sham" forms of acupuncture where the patient, practitioner, and analyst are blinded seem the most acceptable approach.[63] The under-performance of acupuncture interventions in such sham controlled trials may indicate that therapeutic effects are due entirely to non-specific effects, or that the sham treatments are not inert or systematic protocols yield less than optimal treatment.[65][66] A 2012 review found "A common control procedure has been the use of sham acupuncture where needles are inserted on either meridians not specific for the condition under study, or in areas outside meridians; often this is coupled with a more superficial needle insertion than what is performed in the true acupuncture group."[67] The research seems to suggest that needles do not need to stimulate the traditionally specified acupuncture points or penetrate the skin to attain an anticipated effect (e.g. psychosocial factors).[5] A 2012 review found "acupuncture was not better than sham interventions or conventional therapy in the longer term."[67] The evidence suggests that any benefits of acupuncture are short-lasting.[16]
Any evidence on the effectiveness of acupuncture is "variable and inconsistent, even for single conditions",[11] and publication bias is cited as a concern in the reviews of randomized controlled trials (RCTs) of acupuncture.[11][68][69] A 1998 review of studies on acupuncture found that trials originating in China, Japan, Hong Kong and Taiwan were uniformly favourable to acupuncture, as were ten out of 11 studies conducted in Russia.[70] A 2011 assessment of the quality of RCTs on TCM, including acupuncture, concluded that the methodological quality of most such trials (including randomization, experimental control and blinding) was generally poor, particularly for trials published in Chinese journals (though the quality of acupuncture trials was better than the drug-related trials).[71] The study also found that trials published in non-Chinese journals tended to be of higher quality.[71]
A 2014 Nature Reviews Cancer article found that "contrary to the claimed mechanism of redirecting the flow of qi through meridians, researchers usually find that it generally does not matter where the needles are inserted, how often (that is, no dose-response effect is observed), or even if needles are actually inserted. In other words, ‘sham’ or ‘placebo’ acupuncture generally produces the same effects as ‘real’ acupuncture and, in some cases, does better."[72] A 2013 meta-analysis found little evidence that the effectiveness of acupuncture on pain (compared to sham) was modified by the location of the needles, the number of needles used, the experience or technique of the practitioner, or by the circumstances of the sessions.[73] The same analysis also suggested that the number of needles and sessions is important, as greater numbers improved the outcomes of acupuncture compared to non-acupuncture controls.[73] A 2013 editorial found that the inconsistency of results of acupuncture studies (that acupuncture relieved pain in some conditions but had no effect in other very similar conditions) suggests false positive results, which may be caused by factors like biased study designs, poor blinding, and the classification of electrified needles (a type of TENS) as acupuncture.[11] The same editorial suggested that given the inability to find consistent results despite more than 3,000 studies of acupuncture, the treatment seems to be a placebo effect and the existing equivocal positive results are noise one expects to see after a large number of studies are performed on an inert therapy.[11] It concluded that the best controlled studies showed a clear pattern, in which the outcome does not rely upon needle location or even needle insertion, and since "these variables are those that define acupuncture, the only sensible conclusion is that acupuncture does not work."[11]
Pain
A 2014 systematic review suggests that the nocebo effect of acupuncture is clinically relevant and that the rate of adverse events may be a gauge of the nocebo effect.[74] A 2012 meta-analysis conducted by the Acupuncture Trialists' Collaboration found "relatively modest" efficiency of acupuncture (in comparison to sham) for the treatment of four different types of chronic pain, and on that basis concluded that it "is more than a placebo" and a reasonable referral option.[75] Commenting on this meta-analysis, both Edzard Ernst and David Colquhoun said the results were of negligible clinical significance.[76][77]A 2011 overview of high-quality Cochrane reviews suggested that acupuncture is effective for some but not all kinds of pain.[12] A 2011 systematic review of systematic reviews which highlighted recent high-quality RCTs found that for reducing pain, real acupuncture was no better than sham acupuncture, and concluded that numerous reviews have shown little convincing evidence that acupuncture is an effective treatment for reducing pain.[8] The same review found that neck pain was one of only four types of pain for which a positive effect was suggested, but cautioned that the primary studies used carried a considerable risk of bias.[8]
A 2010 systematic review suggested that acupuncture is more than a placebo for commonly occurring chronic pain conditions, but the authors acknowledged that it is still unknown if the overall benefit is clinically meaningful or cost-effective.[78] A 2010 review found real acupuncture and sham acupuncture produce similar improvements, which can only be accepted as evidence against the efficacy of acupuncture.[79] The same review found limited evidence that real acupuncture and sham acupuncture appear to produce biological differences despite similar effects.[79] A 2009 systematic review and meta-analysis found that acupuncture had a small analgesic effect, which appeared to lack any clinical importance and could not be discerned from bias.[17] The same review found that it remains unclear whether acupuncture reduces pain independent of a psychological impact of the needling ritual.[17]
Low back
A 2013 systematic review found supportive evidence that real acupuncture may be more effective than sham acupuncture with respect to relieving lower back pain, but there were methodological limitations with the studies.[80] A 2013 systematic review found that acupuncture may be effective for nonspecific lower back pain, but the authors noted there were limitations in the studies examined, such as heterogeneity in study characteristics and low methodological quality in many studies.[81] A 2012 systematic review found some supporting evidence that acupuncture was more effective than no treatment for chronic non-specific low back pain; the evidence was conflicting comparing the effectiveness over other treatment approaches.[10] A 2011 overview of Cochrane reviews found inconclusive evidence regarding acupuncture efficacy in treating low back pain.[12] A 2011 systematic review of systematic reviews found that "for chronic low back pain, individualized acupuncture is not better in reducing symptoms than formula acupuncture or sham acupuncture with a toothpick that does not penetrate the skin."[8] A 2013 meta-analysis found that acupuncture was better than no treatment for reducing lower back pain, but not better than sham acupuncture, and concluded that the effect of acupuncture "is likely to be produced by the nonspecific effects of manipulation".[82] A 2010 review found that sham acupuncture was as effective as real acupuncture for chronic low back pain.[5] The specific therapeutic effects of acupuncture were small, whereas its clinically relevant benefits were mostly due to contextual and psychosocial circumstances.[5] Brain imaging studies have shown that traditional acupuncture and sham acupuncture differ in their effect on limbic structures, while at the same time showed equivalent analgesic effects.[5] Commenting on this review, David Gorski stated "if quackademic medicine can infiltrate the NEJM, there’s nowhere it can't go."[83] A 2005 Cochrane review found insufficient evidence to recommend for or against either acupuncture or dry needling for acute low back pain.[84] The same review found low quality evidence for pain relief and improvement compared to no treatment or sham therapy for chronic low back pain only in the short term immediately after treatment.[84] The same review also found that acupuncture is not more effective than conventional therapy and other alternative medicine treatments.[84]Headaches and migraines
A 2012 review found that acupuncture has demonstrated benefit for the treatment of headaches, but that safety needed to be more fully documented in order to make any strong recommendations in support of its use.[85] A 2009 Cochrane review of the use of acupuncture for migraine prophylaxis treatment concluded that "true" acupuncture was no more efficient than sham acupuncture, but "true" acupuncture appeared to be as effective as, or possibly more effective than routine care in the treatment of migraines, with fewer adverse effects than prophylactic drug treatment.[86] The same review stated that the specific points chosen to needle may be of limited importance.[86] A 2009 Cochrane review found insufficient evidence to support acupuncture for tension-type headaches.[86]The same review found evidence that suggested that acupuncture might be considered a helpful non-pharmacological approach for frequent episodic or chronic tension-type headache.[86] A separate 2009 Cochrane review found that acupuncture could be useful in the prophylaxis of tension-type headaches.[87]
Osteoarthritis
As of 2014[update] a meta-analysis showed that acupuncture may help osteoarthritis pain but it was noted that the effects were insignificant in comparison to sham needles.[88] A 2013 systematic review and network meta-analysis found that the evidence suggests that acupuncture may be considered one of the more effective physical treatments for alleviating pain due to knee osteoarthritis in the short-term compared to other relevant physical treatments, though much of the evidence in the topic is of poor quality and there is uncertainty about the efficacy of many of the treatments.[89] A 2012 review found "the potential beneficial action of acupuncture on osteoarthritis pain does not appear to be clinically relevant."[67] A 2014 review concluded that "current evidence supports the use of acupuncture as an alternative to traditional analgesics in osteoarthritis patients."[90] A 2010 Cochrane review found that acupuncture shows statistically significant benefit over sham acupuncture in the treatment of peripheral joint osteoarthritis; however, these benefits were found to be so small that their clinical significance was doubtful, and "probably due at least partially to placebo effects from incomplete blinding".[91] The Osteoarthritis Research Society International released a set of consensus recommendations in 2008 which concluded that acupuncture may be useful for treating the symptoms of osteoarthritis of the knee.[92] A separate guideline issued by the National Clinical Guideline Centre stated that acupuncture should not be used in osteoarthritis management.[93]Extremity conditions
A 2007 review found that acupuncture was significantly better than sham acupuncture at treating chronic knee pain; the evidence was not conclusive due to the lack of large, high-quality trials.[94] A 2014 systematic review found moderate quality evidence that acupuncture was more effective than sham acupuncture in the treatment of lateral elbow pain.[95] A 2014 systematic review found that although manual acupuncture was effective at relieving short-term pain when used to treat tennis elbow, its long-term effect in relieving pain was "unremarkable".[96]A 2011 overview of Cochrane reviews found inconclusive evidence regarding acupuncture efficacy in treating shoulder pain and lateral elbow pain.[12]
Nausea and vomiting and post-operative pain
A 2014 overview of systematic reviews found insufficient evidence to suggest that acupuncture is an effective treatment for postoperative nausea and vomiting (PONV) in a clinical setting.[97] A 2013 systematic review concluded that acupuncture might be beneficial in prevention and treatment of PONV.[98] A 2009 Cochrane review found that stimulation of the P6 acupoint on the wrist was as effective (or ineffective) as antiemetic drugs and was associated with minimal side effects.[97][99] The same review found "no reliable evidence for differences in risks of postoperative nausea or vomiting after P6 acupoint stimulation compared to antiemetic drugs."[99]A 2014 overview of systematic reviews found insufficient evidence to suggest that acupuncture is effective for surgical or post-operative pain.[97] For the use of acupuncture for post-operative pain, there was contradictory evidence.[97] A 2014 systematic review found supportive but limited evidence for use of acupuncture for acute post-operative pain after back surgery.[100] A 2014 systematic review found that while the evidence suggested acupuncture could be an effective treatment for postoperative gastroparesis, a firm conclusion could not be reached because the trials examined were of low quality.[101]
Allergies
A 2015 meta-analysis suggests that acupuncture might be a good option for people with allergic rhinitis (AR).[102] Several randomized clinical trials (RCTs) support the use of acupuncture for AR and itch.[103] Experimental studies refer to a specific effect of acupuncture in atopic eczema and asthma, but large RCTs are lacking.[103] Using acupuncture to treat other allergic conditions such as contact eczema, drug rashes, or anaphylaxis is not recommended.[103] Additional research is required to clearly determine any effects of allergic disease therapy above placebo.[103] There is insufficient evidence that acupuncture has specific effects on seasonal allergic rhinitis (SAR).[104] There is some evidence that acupuncture might have specific effects on perennial allergic rhinitis (PAR), though all of the efficacy studies were small and conclusions should be made with caution.[104] There is mixed evidence for the symptomatic treatment or prevention of AR.[105] For seasonal AR, the evidence failed to demonstrate specific effects for acupuncture.[105] For perennial AR, there was suggestive evidence for the effectiveness of acupuncture.[105] Acupuncture is an unproven treatment for allergic-immunologic conditions.[106] A 2015 clinical practice guideline released by the American Academy of Otolaryngology – Head and Neck Surgery stated that clinicians may offer acupuncture as a treatment for allergic rhinitis to patients interested in non-pharmacologic treatments.[107] The confidence in the evidence of effectiveness of acupuncture for this condition was low.[108]Attention deficit hyperactivity disorder
A 2011 Cochrane review concluded that there was no evidence to support the use of acupuncture for attention deficit hyperactivity disorder (ADHD).[109] A 2011 review concluded there was limited evidence as to the effectiveness of acupuncture as a treatment option for ADHD but cautioned that firm conclusions could not be drawn because of the risk of bias.[110]A 2012 systematic review of randomised clinical trials (RCTs) using acupuncture in the treatment of cancer pain found that the number and quality of RCTs was too low to draw definite conclusions.[111] A 2011 Cochrane review found that there is insufficient evidence to determine whether acupuncture is an effective treatment for cancer pain in adults.[112] A 2014 systematic review found that acupuncture may be effective as an adjunctive treatment to palliative care for cancer patients.[113]
A 2013 systematic review found that acupuncture is an acceptable adjunctive treatment for chemotherapy-induced nausea and vomiting, but that further research with a low risk of bias is needed.[114] A 2013 systematic review found that the quantity and quality of available RCTs for analysis were too low to draw valid conclusions for the effectiveness of acupuncture for cancer-related fatigue.[115] A 2014 systematic review reached inconclusive results with regard to the effectiveness of acupuncture for treating cancer-related fatigue.[116] A 2012 systematic review and meta-analysis found very limited evidence regarding the effectiveness of acupuncture compared with conventional intramuscular injections for the treatment of hiccups in cancer patients.[117] The methodological quality and amount of RCTs in the review was low.[117]
Depression
A 2013 Cochrane review found unclear evidence for major depressive disorders in pregnant women.[118] A 2010 Cochrane review found insufficient evidence to recommend acupuncture to treat depression.[119] A 2010 systematic review of systematic reviews found that the effectiveness of acupuncture to treat depression is unproven and their conclusions are "consistent with acupuncture effects in depression being indistinguishable from placebo effects."[120] A 2010 review concluded that acupuncture was safe and effective in the treatment of major depressive disorder and post-stroke depression.[121]Fertility and childbirth
A 2014 systematic review and meta-analysis found poor quality evidence for use of acupuncture in infertile men to improve sperm motility, sperm concentration, and the pregnancy rate; the evidence was rated as insufficient to draw any conclusion regarding efficacy.[122] A 2013 Cochrane review found no evidence of acupuncture for improving the success of in vitro fertilization (IVF).[123] A 2013 systematic review found no benefit of adjuvant acupuncture for IVF on pregnancy success rates.[124] A 2012 systematic review found that acupuncture may be a useful adjunct to IVF,[125] but its conclusions were rebutted after reevaluation using more rigorous, high quality meta-analysis standards.[126] A 2011 overview of systematic reviews found that the evidence that acupuncture was effective was not compelling for most gynecologic conditions. The exceptions to this conclusion included the use of acupuncture during embryo transfer as an adjunct to in vitro fertilization.[127] A 2012 systematic review and meta-analysis found that acupuncture did not significantly improve the outcomes of in vitro fertilization.[128]Obesity
Two reviews have found low quality evidence that acupuncture was effective for the treatment of obesity.[129][130]Rheumatological conditions
A 2013 Cochrane review found low to moderate evidence that acupuncture improves pain and stiffness in treating people with fibromyalgia compared with no treatment and standard care.[131] A 2012 review found "there is insufficient evidence to recommend acupuncture for the treatment of fibromyalgia."[67] A 2010 systematic review found a small pain relief effect that was not apparently discernible from bias; acupuncture is not a recommendable treatment for the management of fibromyalgia on the basis of this review.[132]A 2012 review found that the effectiveness of acupuncture to treat rheumatoid arthritis is "sparse and inconclusive."[67] A 2005 Cochrane review concluded that acupuncture use to treat rheumatoid arthritis "has no effect on ESR, CRP, pain, patient's global assessment, number of swollen joints, number of tender joints, general health, disease activity and reduction of analgesics."[133] A 2010 overview of systematic reviews found insufficient evidence to recommend acupuncture in the treatment of most rheumatic conditions, with the exceptions of osteoarthritis, low back pain, and lateral elbow pain.[134]
Stroke
A 2014 overview of systematic reviews and meta-analyses found that the evidence does not demonstrate acupuncture helps reduce the rates of death or disability after a stroke or improve other aspects of stroke recovery, such as poststroke motor dysfunction, but the evidence suggests it may help with poststroke neurological impairment and dysfunction such as dysphagia, which would need to be confirmed with future rigorous studies.[135] A 2012 review found evidence of benefit for acupuncture combined with exercise in treating shoulder pain after stroke.[136] A 2010 systematic review found that acupuncture was not effective as a treatment for functional recovery after a stroke.[137] A 2008 Cochrane review found that evidence was insufficient to draw any conclusion about the effect of acupuncture on dysphagia after acute stroke.[138] A 2006 Cochrane review found no clear evidence for acupuncture on subacute or chronic stroke.[139] A 2005 Cochrane review found no clear evidence of benefit for acupuncture on acute stroke.[140] A 2014 meta-analysis found tentative evidence for acupuncture in cerebral infarction, a type of ischemic stroke, but the authors noted the trials reviewed were often of poor quality.[141] Another 2014 meta-analysis found that the effectiveness of acupuncture for treating spasticity after a stroke was uncertain as the studies available were of poor quality.[142] A 2015 systematic review and meta-analysis found that acupuncture could be effective to treat spasticity after stroke, but called for more studies to be conducted to determine how long its effects lasted.[143]Tinnitus
A 2012 systematic review found that existing RCTs of acupuncture were insufficient to draw firm conclusions regarding acupuncture's effectiveness to treat tinnitus.[144] A 2014 systematic review found that acupuncture might be beneficial as a treatment for tinnitus, but noted that many of the included studies had methodological flaws.[145]A 2009 review found no evidence that acupuncture was superior to sham acupuncture with respect to reducing hot flashes associated with menopause.[146] A 2014 Cochrane review found insufficient evidence to support the effectiveness of acupuncture in the treatment of menopausal vasomotor symptoms.[147] A 2014 meta-analysis found that acupuncture was effective at improving the frequency and severity of hot flashes.[148]
Other conditions
For the following conditions, the Cochrane Collaboration or other reviews have concluded there is no strong evidence of benefit: alcohol dependence,[149] ankle sprain,[150][151] autism,[152][153] chronic asthma,[154] bell's palsy,[155] traumatic brain injury,[156] carpal tunnel syndrome,[157] chronic obstructive pulmonary disease,[158] cardiac arrhythmias,[159] cerebral hemorrhage,[160] cocaine dependence,[161] constipation,[162] depression,[119] diabetic peripheral neuropathy,[163] drug detoxification,[164][165] primary dysmenorrhoea,[166] dyspepsia,[167] enuresis,[168] endometriosis,[169] epilepsy,[170] erectile dysfunction,[171] essential hypertension,[172] glaucoma,[173] gynaecological conditions (except possibly fertility and nausea/vomiting),[174] hot flashes,[146][147][175] hypoxic ischemic encephalopathy in neonates,[176] insomnia,[177][178] irritable bowel syndrome,[179][180] induction of childbirth,[181] labor pain,[182][183] lumbar spinal stenosis,[184] mumps,[185] myopia,[186] obstetrical conditions,[187] Parkinson's disease,[188] polycystic ovary syndrome,[189] premenstrual syndrome,[190] preoperative anxiety,[191] psychological symptoms associated with opioid addiction,[192] restless legs syndrome,[193] schizophrenia,[194] smoking cessation,[195] stress urinary incontinence,[196] acute stroke,[197] stroke rehabilitation,[198] temporomandibular joint dysfunction,[199][200] tennis elbow,[201] uremic itching,[202] uterine fibroids,[203] vascular dementia,[204] and whiplash.[205]Moxibustion and cupping
A 2010 overview of systematic reviews found that moxibustion was effective for several conditions but the primary studies were of poor quality, so there persists ample uncertainty, which limits the conclusiveness of their findings.[206] A 2012 systematic review suggested that cupping therapy seems to be effective for herpes zoster and various other conditions but due to the high risk of publication bias, larger studies are needed to draw definitive conclusions.[207]Safety
Adverse events
Acupuncture is generally safe when administered by an experienced, appropriately trained practitioner using clean technique and sterile single-use needles.[4][18] When not delivered properly by a qualified practitioner it can cause potentially serious adverse effects.[18] To reduce the risk of serious adverse events after acupuncture, acupuncturists should be trained sufficiently.[8] People with serious spinal disease, such as cancer or infection, are not good candidates for acupuncture.[5] Contraindications to acupuncture are conditions that should not be treated with acupuncture; these contraindications include coagulopathy disorders (e.g. haemophilia and advanced liver disease), warfarin use, severe psychiatric disorders (e.g. psychosis), and skin infections or skin trauma (e.g. burns).[5] Further, electroacupuncture should be avoided at the spot of implanted electrical devices (e.g. pacemakers).[5]
A 2011 systematic review of systematic reviews (internationally and without language restrictions) found that serious complications following acupuncture continue to be reported.[8] Between 2000 and 2009, ninety-five cases of serious adverse events, including five deaths, were reported.[8] Many such events are not inherent to acupuncture but are due to malpractice of acupuncturists.[8] This might be why such complications have not been reported in surveys of adequately-trained acupuncturists.[8] Most such reports are from Asia, which may reflect the large number of treatments performed there or it might be because there are a relatively higher number of poorly trained Asian acupuncturists.[8] Many serious adverse events were reported from developed countries.[8] This included Australia, Austria, Canada, Croatia, France, Germany, Holland, Ireland, New Zealand, Spain, Sweden, Switzerland, the UK, and the US.[8] The number of adverse effects reported from the UK appears particularly unusual, which may indicate less under-reporting in the UK than other countries.[8] 38 cases of infections were reported and 42 cases of organ trauma were reported.[8] The most frequent adverse events included pneumothorax, and bacterial and viral infections.[8]
A 2013 review found (without restrictions regarding publication date, study type or language) 295 cases of infections were reported, mycobacterium was the pathogen in at least 96%.[208] Likely sources of infection include towels, hot packs or boiling tank water, and reusing reprocessed needles.[208] Possible sources of infection include contaminated needles, reusing personal needles, a person's skin contained mycobacterium and reusing needles at various sites in the same person.[208] Although acupuncture is generally considered a safe procedure, in the last decade reports of infection transmission have increased significantly, including those of mycobacterium.[208] Although it is recommended that practitioners of acupuncture use disposable needles, the reuse of sterilized needles is still permitted.[208] It is also recommended that thorough control practices for preventing infection be implemented and adapted.[208]
English-language
A 2013 systematic review of the English-language case reports found that serious adverse events associated with acupuncture are rare, but acupuncture is not without risk.[4] Between 2000 and 2011, there were 294 adverse events reported in the English-language literature from 25 countries and regions.[4] The majority of the reported adverse events were relatively minor, and the incidences were low.[4] For example, a prospective survey of 34,000 acupuncture treatments found no serious adverse events and 43 minor ones, a rate of 1.3 per 1000 interventions.[4] Another survey found there were 7.1% minor adverse events, of which 5 were serious, amid 97,733 acupuncture patients.[4] The most common adverse effect observed was infection (e.g. mycobacterium), and the majority of infections were bacterial in nature, caused by skin contact at the needling site.[4] Infection has also resulted from skin contact with unsterilized equipment or dirty towels, in an unhygienic clinical setting.[4]Other adverse complications included five reported cases of spinal cord injuries (e.g. migrating broken needles or needling too deeply), four brain injuries, four peripheral nerve injuries, five heart injuries, seven other organ and tissue injuries, bilateral hand edema, epithelioid granuloma, pseudolymphoma, argyria, pustules, pancytopenia, and scarring due to hot needle technique.[4] Adverse reactions from acupuncture, which are unusual and uncommon in typical acupuncture practice, were syncope, galactorrhoea, bilateral nystagmus, pyoderma gangrenosum, hepatotoxicity, eruptive lichen planus, and spontaneous needle migration.[4]
A 2013 systematic review found 31 cases of vascular injuries were caused by acupuncture, 3 resulting in death.[209] Two died from pericardial tamponade and one was from an aortoduodenal fistula.[209] The same review found vascular injuries were rare, bleeding and pseudoaneurysm were most prevalent.[209] A 2011 systematic review (without restriction in time or language), aiming to summarize all reported case of cardiac tamponade after acupuncture, found 26 cases resulting in 14 deaths, with little doubt about causality in most fatal instances.[210] The same review concluded cardiac tamponade was a serious, usually fatal, though theoretically avoidable complication following acupuncture, and urged training to minimize risk.[210]
A 2012 review found a number of adverse events were reported after acupuncture in the UK's National Health Service (NHS) but most (95%) were not severe.[40] Though, miscategorization and under-reporting may alter the total figures.[40] From January 2009 to December 2011, there were 468 safety incidents recognized within the NHS organizations.[40] The adverse events recorded included retained needles (31%), dizziness (30%), loss of consciousness/unresponsive (19%), falls (4%), bruising or soreness at needle site (2%), pneumothorax (1%) and other adverse side effects (12%).[40] Acupuncture practitioners should know, and be prepared to be responsible for, any substantial harm from treatments.[40] Some acupuncture proponents argue that because of its long history this suggests it is safe.[40] However, there is an increasing literature on adverse events (e.g. spinal cord injury).[40]
Acupuncture seems to be safe in people getting anticoagulants, assuming needles are used at the correct location and depth.[211] Studies are required to verify these findings.[211] The evidence suggests that acupuncture might be a safe option for people with allergic rhinitis.[102]
Chinese, South Korean, and Japanese-language
A 2010 systematic review of the Chinese-language literature found numerous acupuncture-related adverse events including pneumothorax, fainting, subarachnoid hemorrhage, and infection as the most frequent, and cardiovascular injuries, subarachnoid hemorrhage, pneumothorax, and recurrent cerebral hemorrhage as the most serious, most of which were due to improper technique.[31] Between 1980 and 2009, the Chinese literature reported 479 adverse events.[31] Prospective surveys shown that mild, transient acupuncture-associated adverse events ranged from 6.71% to 15%.[31] A study with 190,924 patients, the prevalence of serious adverse events was roughly 0.024%.[31] Another study shown a rate of adverse events requiring specific treatment was 2.2%, 4,963 incidences were among 229,230 patients.[31] Infections, mainly hepatitis, after acupuncture are reported often in the English-language research, though it is rarely reported in the Chinese-language research, making it plausible that in China acupuncture-associated infections have been underreported.[31] Infections were mostly caused by poor sterilization of acupuncture needles.[31] Other adverse events included spinal epidural haematoma (in the cervical, thoracic and lumbar spine), chylothorax, injuries of abdominal organs and tissues, injuries in the neck region, injuries to the eyes, including orbital hemorrhage, traumatic cataract, injury of the oculomotor nerve and retinal puncture, hemorrhage to the cheeks and the hypoglottis, peripheral motor nerve injuries and subsequent motor dysfunction, local allergic reactions to metal needles, stroke, and cerebral hemorrhage after acupuncture.[31] A causal link between acupuncture and the adverse events cardiac arrest, pyknolepsy, shock, fever, cough, thirst, aphonia, leg numbness, and sexual dysfunction remains uncertain.[31] The same review concluded that acupuncture can be considered inherently safe when practiced by properly trained practitioners, but the review also stated there is a need to find effective strategies to minimize the health risks.[31] Between 1999 and 2010, the Republic of Korean-literature contained reports of 1104 adverse events.[212] Between the 1980s and 2002, the Japanese-language literature contained reports of 150 adverse events.[213]Children and pregnancy
When used on children, acupuncture is safe when administered by well-trained, licensed practitioners using sterile needles; however, a 2011 review found there was limited research to draw definite conclusions about the overall safety of pediatric acupuncture.[2] The same review found 279 adverse events, of which 25 were serious.[2] The adverse events were mostly mild in nature (e.g. bruising or bleeding).[2] The prevalence of mild adverse events ranged from 10.1% to 13.5%, an estimated 168 incidences were among 1,422 patients.[2] On rare occasions adverse events were serious (e.g. cardiac rupture or hemoptysis), many might have been a result of substandard practice.[2] The incidence of serious adverse events was 5 per one million, which included children and adults.[2] When used during pregnancy, the majority of adverse events caused by acupuncture were mild and transient, with few serious adverse events.[214] The most frequent mild adverse event was needling or unspecified pain, followed by bleeding.[214] Although two deaths (one stillbirth and one neonatal death) were reported, there was a lack of acupuncture associated maternal mortality.[214] Limiting the evidence as certain, probable or possible in the causality evaluation, the estimated incidence of adverse events following acupuncture in pregnant women was 131 per 10,000.[214] Although acupuncture is not contraindicated in pregnant women, some specific acupuncture points that are particularly sensitive to needle insertion; these spots, as well as the abdominal region, should be avoided during pregnancy.[5]Moxibustion and cupping
Four adverse events associated with moxibustion were bruising, burns and cellulitis, spinal epidural abscess, and large superficial basal cell carcinoma.[4] Ten adverse events were associated with cupping.[4] The minor ones were keloid scarring, burns, and bullae;[4] the serious ones were acquired hemophilia A, stroke following cupping on the back and neck, factitious panniculitis, reversible cardiac hypertrophy, and iron deficiency anemia.[4]Cost-effectiveness
A 2013 meta-analysis found that acupuncture for chronic low back pain was cost-effective as a complement to standard care, but not as a substitute for standard care except in cases where comorbid depression presented.[19] The same meta-analysis found there was no difference between sham and non-sham acupuncture.[19] A 2011 systematic review found insufficient evidence for the cost-effectiveness of acupuncture in the treatment of chronic low back pain.[20] A 2010 systematic review found that the cost-effectiveness of acupuncture could not be concluded.[78] A 2012 review found that acupuncture was cost-effective for some[215] pain conditions.Risk of forgoing conventional medical care
As with other alternative medicines, unethical or naïve practitioners may induce patients to exhaust financial resources by pursuing ineffective treatment.[7][216] Profession ethical codes set by accrediting organizations such as the National Certification Commission for Acupuncture and Oriental Medicine require practitioners to make "timely referrals to other health care professionals as may be appropriate."[217]Theory
| Acupuncture | |||
| Simplified Chinese | 针刺 | ||
|---|---|---|---|
Qi, meridians and acupuncture points
Traditional Chinese medicine (TCM) distinguishes several different kinds of qi.[220] In a general sense, qi is something that is defined by five "cardinal functions":[220][221]Actuation (推動, tuīdòng) is of all physical processes in the body, especially the circulation of all body fluids such as blood in their vessels.[221] This includes actuation of the functions of the zang-fu organs and meridians.[221] Warming (溫煦, pinyin: wēnxù) the body, especially the limbs.[221] Defense (防御, pinyin: fángyù) against Exogenous Pathogenic Factors[221] Containment (固攝, pinyin: gùshè) of body fluids, i.e. keeping blood, sweat, urine, semen etc. from leakage or excessive emission.[221] Transformation (氣化, pinyin: qìhuà) of food, drink, and breath into qi, xue (blood), and jinye ("fluids"), and/or transformation of all of the latter into each other.[221]
To fulfill its functions, qi has to steadily flow from the inside of the body (where the zang-fu organs are located) to the "superficial" body tissues of the skin, muscles, tendons, bones, and joints.[222] It is assisted in its flow by "channels" referred to as meridians.[222] TCM identifies 12 "regular" and 8 "extraordinary" meridians; the Chinese terms being 十二经脉 (pinyin: shí-èr jīngmài, lit. "the Twelve Vessels") and 奇经八脉 (pinyin: qí jīng bā mài).[222] There's also a number of less customary channels branching off from the "regular" meridians.[223] Contemporary research has not supported the existence of qi or meridians.[24][25][26][224] The meridians are believed to connect to the bodily organs, of which those considered hollow organs (such as the stomach and intestines) were also considered yang while those considered solid (such as the liver and lungs) were considered yin. They were also symbolically linked to the rivers found in ancient China, such as the Yangtze, Wei and Yellow Rivers.[225]
Acupuncture points are mainly (but not always) found at specified locations along the meridians.[226] There also is a number of acupuncture points with specified locations outside of the meridians; these are called extraordinary points and are credited to treat certain diseases.[226] A third category of acupuncture points called "A-shi" points have no fixed location but represent tender or reflexive points appearing in the course of pain syndromes.[226] The actual number of points have varied considerably over time, initially they were considered to number 365, symbolically aligning with the number of days in the year (and in Han times, the number of bones thought to be in the body).[227] The Nei ching mentioned only 160 and a further 135 could be deduced giving a total of 295.[227] The modern total was once considered 670 but subsequently expanded due to more recent interest in auricular (ear) acupuncture and the treatment of further conditions.[227] In addition, it is considered likely that some points used historically have since ceased being used.[227]
TCM concept of disease
In TCM, disease is generally perceived as a disharmony or imbalance in the functions or interactions of such concepts as yin, yang, qi, xuĕ, zàng-fǔ, meridians, and of the interaction between the body and the environment.[228] Therapy is based on which "pattern of disharmony" can be identified.[229][230] In the case of the meridians, typical disease patterns are invasions with wind, cold, and damp Excesses.[231] In order to determine which pattern is at hand, practitioners will examine things like the color and shape of the tongue, the relative strength of pulse-points, the smell of the breath, the quality of breathing, or the sound of the voice.[232][233] TCM and its concept of disease do not strongly differentiate between cause and effect.[234] In theory, however, endogenous, exogenous and miscellaneous causes of disease are recognized.[235]Traditional diagnosis
The acupuncturist decides which points to treat by observing and questioning the patient to make a diagnosis according to the tradition used. In TCM, the four diagnostic methods are: inspection, ausculation and olfaction, inquiring, and palpation. Inspection focuses on the face and particularly on the tongue, including analysis of the tongue size, shape, tension, color and coating, and the absence or presence of teeth marks around the edge.[236] Auscultation and olfaction is listening for particular sounds (such as wheezing) and attending to body odor.[236] Inquiring is focusing on the "seven inquiries": chills and fever; perspiration; appetite, thirst and taste; defecation and urination; pain; sleep; and menses and leukorrhea.[236] Palpation is focusing on feeling the body for tender A-shi points and feeling the left and right radial pulses.[236] There is significant heterogeneity among acupuncturists considering appropriate treatment protocols.[65]Tongue and pulse
Examination of the tongue and the pulse are among the principal diagnostic methods in TCM. Certain sectors of the tongue's surface are believed to correspond to the zàng-fŭ. For example, teeth marks on one part of the tongue might indicate a problem with the heart, while teeth marks on another part of the tongue might indicate a problem with the liver.[232]Pulse palpation involves measuring the pulse at a superficial and at a deep level at three locations on the radial artery (Cun, Guan, Chi, located two fingerbreadths from the wrist crease, one fingerbreadth from the wrist crease, and right at the wrist crease, respectively, usually palpated with the index, middle and ring finger) of each arm, for 12 pulses, all of which are thought to correspond with certain zàng-fŭ. The pulse is examined for several characteristics including rhythm, strength, and volume, and is described with qualities like "floating, slippery, bolstering-like, feeble, thready and quick". Each of these qualities indicate certain disease patterns. Training on the use of TCM pulse diagnosis can take several years.[237]
Scientific view on TCM theory
Some modern practitioners have embraced the use of acupuncture to treat pain, but have abandoned the use of qi, meridians, yin and yang as explanatory frameworks.[26][27] Some practitioners no longer consider the idea of an energy flow to apply.[28] They, along with acupuncture researchers, explain the analgesic effects of acupuncture as caused by the release of endorphins, and recognize the lack of evidence that it can affect the course of any disease.[28][29] A 2014 review stated that despite ample controversy encircling the validity of acupuncture as a modality, developing literature on its physiological effects in animals and humans is giving new views into the basic mechanisms for acupuncture needling.[238] The same review proposed a model combining both connective tissue plasticity and peripheral sensory modulation as a needle response for acupuncture's physiological effects.[238] The evidence indicates that acupuncture-induced pain relief effect has physiological, anatomical and neurochemical origins.[239] The mechanism of action for acupuncture is still unclear.[240] Evidence suggests that acupuncture generates a sequence of events that include the release of endogenous opioid-like substances that modulate pain signals within the central nervous system.[240] However, a 2014 Nature Reviews Cancer article found that the key mouse studies that suggested acupuncture relieves pain via the local release of adenosine, which then triggered close-by A1 receptors "caused more tissue damage and inflammation relative to the size of the animal in mice than in humans, such studies unnecessarily muddled a finding that local inflammation can result in the local release of adenosine with analgesic effect."[72] The use of qi as an explanatory framework has been decreasing in China, even as it becomes more prominent during discussions of acupuncture in the United States.[29] Despite the scientific evidence against such mystical explanations, academic discussions of acupuncture still make reference to pseudoscientific concepts like qi and meridians, in practice making many scholarly efforts to integrate evidence for efficacy and discussions of the mechanism impossible.[29] Qi, yin, yang and meridians have no counterpart in modern studies of chemistry, biology, physics, or human physiology and to date scientists have been unable to find evidence that supports their existence.[n 2][25]
It is a generally held belief within the acupuncture community that acupuncture points and meridians structures are special conduits for electrical signals but no research has established any consistent anatomical structure or function for either acupuncture points or meridians.[n 2][25] The electrical resistance of acupuncture points and meridians have also been studied, with conflicting results.[25] There has been little systematic investigation of which components of an acupuncture session may be important for any therapeutic effect, including needle placement and depth, type and intensity of stimulation, and number of needles used.[65]
Quackwatch states that:[7]
TCM theory and practice are not based upon the body of knowledge related to health, disease, and health care that has been widely accepted by the scientific community. TCM practitioners disagree among themselves about how to diagnose patients and which treatments should go with which diagnoses. Even if they could agree, the TCM theories are so nebulous that no amount of scientific study will enable TCM to offer rational care.
History
Antiquity
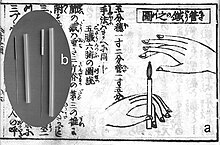
The precise start date that acupuncture was generally held to have originated in ancient China and how it evolved from early times is uncertain.[32] Chinese history attributes the introduction of acupuncture to the emperor Shennong.[33] One explanation is that Han Chinese doctors observed that some soldiers wounded in battle by arrows were believed to have been cured of chronic afflictions that were otherwise untreated,[241] and there are variations on this idea.[242] Sharpened stones known as Bian shi have been found in China, suggesting the practice may date to the Neolithic[243] or possibly even earlier in the Stone Age.[244] Hieroglyphs and pictographs have been found dating from the Shang Dynasty (1600–1100 BCE) which suggests that acupuncture was practiced along with moxibustion.[34] It has also been suggested that acupuncture has its origins in bloodletting[245] or demonology.[246]
Despite improvements in metallurgy over centuries, it was not until the 2nd century BCE during the Han Dynasty that stone and bone needles were replaced with metal.[243] The earliest examples of metal needles were found in a tomb dated to c. 113 BCE, though their use might not necessarily have been acupuncture.[247] The earliest example of the unseen meridians (经络, pinyin: jīng-luò) used for diagnosis and treatment are dated to the second century BCE but these records do not mention needling, while the earliest reference to therapeutic needling occurs in the historical Shiji text (史記, English: Records of the Grand Historian) but does not mention the meridians and may be a reference to lancing rather than acupuncture.[247]
The earliest written record of acupuncture is found in the Huangdi Neijing (黄帝内经; translated as The Yellow Emperor's Inner Canon), dated approximately 200 BCE.[248] It does not distinguish between acupuncture and moxibustion and gives the same indication for both treatments.[248] The Mawangdui texts, which also date from the 2nd century BCE (though antedating both the Shiji and Huangdi Neijing), mention the use of pointed stones to open abscesses, and moxibustion, but not acupuncture.[248] However, by the 2nd century BCE, acupuncture replaced moxibustion as the primary treatment of systemic conditions.[248]
The practice of acupuncture expanded out of China into the areas now part of Japan, Korea, Vietnam and Taiwan, diverging from the narrower theory and practice of mainland TCM in the process.[249] A large number of contemporary practitioners outside of China follow these non-TCM practices, particularly in Europe.[250]
In Europe, examinations of the 5,000-year-old mummified body of Ötzi the Iceman have identified 15 groups of tattoos on his body, some of which are located on what are now seen as contemporary acupuncture points.[251] This has been cited as evidence that practices similar to acupuncture may have been practiced elsewhere in Eurasia during the early Bronze Age.[251]
Middle history
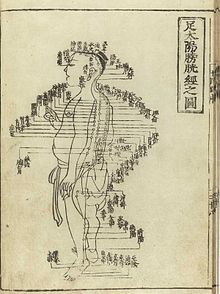
Acupuncture chart from Shisi jing fahui (Expression of the Fourteen Meridians) written by Hua Shou (fl. 1340s, Ming Dynasty). Japanese reprint by Suharaya Heisuke (Edo, 1. year Kyōhō = 1716).
Korea is believed to be the second country that acupuncture spread to outside of China.[252] Within Korea there is a legend that acupuncture was developed by the legendary emperor Dangun though it is more likely to have been brought into Korea from a Chinese colonial prefecture.[252]
Around 90 works on acupuncture were written in China between the Han Dynasty and the Song Dynasty, and the Emperor Renzong of Song, in 1023, ordered the production of a bronze statuette (Dongren) depicting the meridians and acupuncture points then in use.[252] However, after the end of the Song Dynasty, acupuncture lost status, and started to be seen as a technical profession, in comparison to the more scholarly profession of herbalism.[253] It became rarer in the following centuries, and was associated with less prestigious practices like alchemy, shamanism, midwifery and moxibustion.[253]
Portuguese missionaries in the 16th century were among the first to bring reports of acupuncture to the West.[254] Jacob de Bondt, a Dutch surgeon traveling in Asia, described the practice in both Japan and Java.[255] However, in China itself the practice was increasingly associated with the lower-classes and illiterate practitioners.[255]
In 1674, Hermann Buschoff, a Dutch priest in Batavia, published the first book on moxibustion (from Japanese mogusa).[256] The first elaborate Western treatise on acupuncture was published in 1683 by Willem ten Rhijne, a Dutch physician who had worked at the Dutch trading post Dejima in Nagasaki for two years.[257] In 1712 a detailed description of the treatment of "Colics" in Japan was published by the German physician Engelbert Kaempfer. But while moxibustion was widely discussed among central European physicians, ten Rhijne's and especially Kaempfer's explanations about piercing the abdomen had caused some misunderstandings that eventually led to the refutal of acupuncture by influential scholars such as Lorenz Heister and Georg Stahl.[258]
In 1757 the Chinese physician Xu Daqun described the further decline of acupuncture, saying it was a lost art, with few experts to instruct; its decline was attributed in part to the popularity of prescriptions and medications, as well as its association with the lower classes.[259] In 1822, an edict from the Emperor Daoguang banned the practice and teaching of acupuncture within the Imperial Academy of Medicine outright, as unfit for practice by gentlemen-scholars.[260] At this point, acupuncture was still cited in Europe with both skepticism and praise, with little study and only a small amount of experimentation.[260]
While the details of how acupuncture came to Europe are debated, the French doctor Louis Berlioz (the father of the composer Hector Berlioz) is usually credited with first experimenting the procedure in 1810, before publishing his findings in 1816.[260] In the United States, the earliest reports of acupuncture date back to 1826, when Franklin Bache, a surgeon of the United States Navy, published a report in the North American Medical and Surgical Journal on his use of acupuncture to treat lower back pain.[261] Since the beginning of the 19th century, acupuncture was practiced by Asian immigrants living in Chinatowns.[261]
Modern era
In the early years after the Chinese Civil War, Chinese Communist Party leaders ridiculed traditional Chinese medicine, including acupuncture, as superstitious, irrational and backward, claiming that it conflicted with the Party's dedication to science as the way of progress.[262] Communist Party Chairman Mao Zedong later reversed this position, saying that "Chinese medicine and pharmacology are a great treasure house and efforts should be made to explore them and raise them to a higher level."[262] Under Mao's leadership, in response to the lack of modern medical practitioners, acupuncture was revived and its theory rewritten to adhere to the political, economic and logistic necessities of providing for the medical needs of China's population. Despite Mao proclaiming the practice of Chinese medicine to be "scientific", the practice was based more on the materialist assumptions of Marxism in opposition to superstition rather than the Western practice of empirical investigation of nature.[263] Later the 1950s TCM's theory was again rewritten at Mao's insistence as a political response to the lack of unity between scientific and traditional Chinese medicine, and to correct the supposed "bourgeois thought of Western doctors of medicine".[263] Despite publicly promoting the practice, Mao himself did not believe in or use traditional Chinese medicine.[264]Acupuncture gained attention in the United States when the U.S. President Richard Nixon visited China in 1972.[265] During one part of the visit, the delegation was shown a patient undergoing major surgery while fully awake, ostensibly receiving acupuncture rather than anesthesia.[265] Later it was found that the patients selected for the surgery had both a high pain tolerance and received heavy indoctrination before the operation; these demonstration cases were also frequently receiving morphine surreptitiously through an intravenous drip that observers were told contained only fluids and nutrients.[265] One patient receiving open heart surgery while awake was ultimately found to have received a combination of three powerful sedatives as well as large injections of a local anesthetic into the wound.[11]
The greatest exposure in the West came after New York Times reporter James Reston received acupuncture in Beijing for post-operative pain in 1971 and wrote complaisantly about it in his newspaper.[266] In 1972 the first legal acupuncture center in the U.S. was established in Washington DC; during 1973-1974, this center saw up to one thousand patients.[267] In 1973 the American Internal Revenue Service allowed acupuncture to be deducted as a medical expense.[268]
Acupuncture has been the subject of active scientific research both in regard to its basis and therapeutic effectiveness since the late 20th century.[14] Even though acupuncture is currently widely used in clinical practice, it remains a controversial topic.[14] In 2006, a BBC documentary Alternative Medicine filmed a patient undergoing open heart surgery allegedly under acupuncture-induced anesthesia. It was later revealed that the patient had been given a cocktail of weak anesthetics that in combination could have a much more powerful effect. The program was also criticized for its fanciful interpretation of the results of a brain scanning experiment.[269][270] In 2010, acupuncture was recognized by UNESCO as part of the world's intangible cultural heritage.[271]
Ethics
The National Institutes of Health (NIH) consensus statement and conference that produced it in 1997 were criticized by Wallace Sampson, founder of the Scientific Review of Alternative Medicine, writing for an affiliated publication of Quackwatch who stated the meeting was chaired by a strong proponent of acupuncture and failed to include speakers who had obtained negative results on studies of acupuncture. Sampson also stated he believed the report showed evidence of pseudoscientific reasoning.[272]The 2003 World Health Organization's (WHO) report was controversial; critics assailed it as being problematic since, in spite of the disclaimer, supporters used it to claim that the WHO endorsed acupuncture that were lacking sufficient evidence-basis.[273] Medical scientists expressed concern that the evidence supporting acupuncture outlined in the report was weak, and Willem Betz of SKEPP (Studie Kring voor Kritische Evaluatie van Pseudowetenschap en het Paranormale, the Study Circle for the Critical Evaluation of Pseudoscience and the Paranormal) said that the report was evidence that the "WHO has been infiltrated by missionaries for alternative medicine".[273] The WHO 2003 report was also criticized in the 2008 book Trick or Treatment for, in addition to being produced by a panel that included no critics of acupuncture, containing two major errors – including too many results from low-quality clinical trials, and including a large number of trials originating in China where, probably due to publication bias, no negative trials have ever been produced.[274] Ernst and Singh, the authors of the book, described the report as "highly misleading" and a "shoddy piece of work that was never rigorously scrutinized" and stated that the results of high-quality clinical trials do not support the use of acupuncture to treat anything but pain and nausea.[274] Ernst also described the statement in a 2006 peer reviewed article as "[p]erhaps the most obviously over-optimistic overview [of acupuncture]", noting that of the 35 conditions that the WHO stated acupuncture was effective for, 27 of the systematic reviews that the WHO report was based on found that acupuncture was not effective for treating the specified condition.[3]
Placebos have been used in medical care to treat the elderly.[275] For example, a response to "sham" acupuncture in osteoarthritis may be used in the elderly.[275] Placebos have usually been regarded as deception and thus unethical.[275] However, some physicians and ethicists have suggested circumstances for applicable uses for placebos such as it might present a theoretical advantage of an inexpensive treatment without adverse reactions or interactions with drugs or other medications.[275]
Acupuncture is a commonly used alternative medicine modality. Many physicians in the UK appear to recommend alternative medicine, which raises ethical issues. Physicians have a duty of care requiring that each patient be treated with the best treatment for a given condition and situation. As the evidence for most types of alternative medicine is far from strong, the use of alternative medicine in regular healthcare can present an ethical question. A large proportion of physicians in the UK appear to employ some type of alternative medicine, but many have not received the relevant training, which raises issues associated with medical ethics and professional competence.[276]
According to David Gorski, "What Berman is doing in this article in the NEJM is the same thing that CAM advocates in general and acupuncture apologists in particular have a maddening tendency to do. They either cherry pick studies that appear to indicate that their favored woo works. When, as Berman et al were, they are forced to admit that well-designed studies with lots of patients show that their woo is no better than a valid placebo control, they then shift to embracing the placebo, to owning it, so to speak, all without actually calling it placebo".[83]
Acupuncture is perceptibly used at academic medical centers despite little or no convincing scientific evidence for explicit effects for any condition that is discernible from placebo.[72] The evidence that the majority of CAM modalities, such as acupuncture, are little more than 'theatrical placebos' is so compelling that some proponents of acupuncture have essentially conceded this position by advocating the 'harnessing of placebo effects' or developing 'meaningful placebos'.[72]