From Wikipedia, the free encyclopedia
|
|
| Transcranial magnetic stimulation | |
|---|---|
| Intervention | |

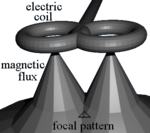
Transcranial magnetic stimulation (schematic diagram)
|
|
TMS is used diagnostically to measure the connection between the brain and a muscle to evaluate damage from stroke, multiple sclerosis, amyotrophic lateral sclerosis, movement disorders, motor neuron disease and injuries and other disorders affecting the facial and other cranial nerves and the spinal cord.[3]
Evidence suggests it is useful for neuropathic pain[4] and treatment-resistant major depressive disorder.[4][5] A 2015 Cochrane review found not enough evidence to make any conclusions in schizophrenia.[6] For negative symptoms another review found possible efficacy.[4] As of 2014, all other investigated uses of repetitive TMS have only possible or no clinical efficacy.[4]
Matching the discomfort of TMS to distinguish true effects from placebo is an important and challenging issue that influences the results of clinical trials.[4][7][8][9] The greatest risks of TMS are the rare occurrence of syncope (fainting) and even less commonly, induced seizures.[7] Other adverse effects of TMS include discomfort or pain, transient induction of hypomania, transient cognitive changes, transient hearing loss, transient impairment of working memory, and induced currents in electrical circuits in implanted devices.[7]
Medical uses
The use of TMS can be divided into diagnostic and therapeutic uses.Diagnosis
TMS can be used clinically to measure activity and function of specific brain circuits in humans.[3] The most robust and widely accepted use is in measuring the connection between the primary motor cortex and a muscle to evaluate damage from stroke, multiple sclerosis, amyotrophic lateral sclerosis, movement disorders, motor neuron disease and injuries and other disorders affecting the facial and other cranial nerves and the spinal cord.[3][10][11][12] TMS has been suggested as a means of assessing short-interval intracortical inhibition (SICI) which measures the internal pathways of the motor cortex but this use has not yet been validated.[13]Treatment
For neuropathic pain, for which there is little effective treatment, high-frequency (HF) repetitive TMS (rTMS) appears effective.[4] For treatment-resistant major depressive disorder, HF-rTMS of the left dorsolateral prefrontal cortex (DLPFC) appears effective and low-frequency (LF) rTMS of the right DLPFC has probable efficacy.[4][5] The Royal Australia and New Zealand College of Psychiatrists has endorsed rTMS for treatment resistant MDD.[14] As of October 2008, the US Food and Drug Administration authorized the use of rTMS as an effective treatment for clinical depression.[15]Adverse effects
Although TMS is generally regarded as safe, risks increase for therapeutic rTMS compared to single or paired TMS for diagnostic purposes.[16] In the field of therapeutic TMS, risks increase with higher frequencies.[7]The greatest immediate risk is the rare occurrence of syncope (fainting) and even less commonly, induced seizures.[7][17]
Other adverse short-term effects of TMS include discomfort or pain, transient induction of hypomania, transient cognitive changes, transient hearing loss, transient impairment of working memory, and induced currents in electrical circuits in implanted devices.[7]
Devices and procedure
During a transcranial magnetic stimulation (TMS) procedure, a magnetic field generator, or "coil" is placed near the head of the person receiving the treatment.[1]:3 The coil produces small electric currents in the region of the brain just under the coil via electromagnetic induction. The coil is positioned by finding anatomical landmarks on the skull including, but not limited to, the inion or the nasion.[18] The coil is connected to a pulse generator, or stimulator, that delivers electric current to the coil.[2]Society and culture
Regulatory approvals
The ANT Neuro neuronavigation solution visor2 was approved as a CE class IIa medical device in April 2012.
Nexstim obtained 510(k) FDA clearance of Navigated Brain Stimulation for the assessment of the primary motor cortex for pre-procedural planning in December 2009.[19]
Nexstim obtained FDA 510K clearance for NexSpeech navigated brain stimulation device for neurosurgical planning in June 2011.[20]
Depression
A number of deep TMS have received FDA 510k clearance to market for use in adults with treatment resistant major depressive disorders.[21][22][23][24]Migraine
The use of single-pulse TMS was approved by the FDA for treatment of migraines in December 2013.[25] It is approved as a Class II medical device under the "de novo pathway".[26][27]Health insurance
United States
Commercial health insurance
In 2013, several commercial health insurance plans in the United States, including Anthem, Health Net, and Blue Cross Blue Shield of Nebraska and of Rhode Island, covered TMS for the treatment of depression for the first time.[28] In contrast, UnitedHealthcare issued a medical policy for TMS in 2013 that stated there is insufficient evidence that the procedure is beneficial for health outcomes in patients with depression. UnitedHealthcare noted that methodological concerns raised about the scientific evidence studying TMS for depression include small sample size, lack of a validated sham comparison in randomized controlled studies, and variable uses of outcome measures.[29] Other commercial insurance plans whose 2013 medical coverage policies stated that the role of TMS in the treatment of depression and other disorders had not been clearly established or remained investigational included Aetna, Cigna and Regence.[30]Medicare
Policies for Medicare coverage vary among local jurisdictions within the Medicare system,[31] and Medicare coverage for TMS has varied among jurisdictions and with time. For example:- In early 2012 in New England, Medicare covered TMS for the first time in the United States.[32] However, that jurisdiction later decided to end coverage after October, 2013.[33]
- In August 2012, the jurisdiction covering Arkansas, Louisiana, Mississippi, Colorado, Texas, Oklahoma, and New Mexico determined that there was insufficient evidence to cover the treatment,[34] but the same jurisdiction subsequently determined that Medicare would cover TMS for the treatment of depression after December 2013.[35]
United Kingdom's National Health Service
The United Kingdom's National Institute for Health and Care Excellence (NICE) issues guidance to the National Health Service (NHS) in England, Wales, Scotland and Northern Ireland. NICE guidance does not cover whether or not the NHS should fund a procedure. Local NHS bodies (primary care trusts and hospital trusts) make decisions about funding after considering the clinical effectiveness of the procedure and whether the procedure represents value for money for the NHS.[36]NICE evaluated TMS for severe depression (IPG 242) in 2007, and subsequently considered TMS for reassessment in January 2011 but did not change its evaluation.[37] The Institute found that TMS is safe, but there is insufficient evidence for its efficacy.[37]
In January 2014, NICE reported the results of an evaluation of TMS for treating and preventing migraine (IPG 477). NICE found that short-term TMS is safe but there is insufficient evidence to evaluate safety for long-term and frequent uses. It found that evidence on the efficacy of TMS for the treatment of migraine is limited in quantity, that evidence for the prevention of migraine is limited in both quality and quantity.[38]
Technical information
TMS – Butterfly Coils
TMS uses electromagnetic induction to generate an electric current across the scalp and skull without physical contact. A plastic-enclosed coil of wire is held next to the skull and when activated, produces a magnetic field oriented orthogonally to the plane of the coil. The magnetic field passes unimpeded through the skin and skull, inducing an oppositely directed current in the brain that activates nearby nerve cells in much the same way as currents applied directly to the cortical surface.[39]
The path of this current is difficult to model because the brain is irregularly shaped and electricity and magnetism are not conducted uniformly throughout its tissues. The magnetic field is about the same strength as an MRI, and the pulse generally reaches no more than 5 centimeters into the brain unless using the deep transcranial magnetic stimulation variant of TMS.[40] Deep TMS can reach up to 6 cm into the brain to stimulate deeper layers of the motor cortex, such as that which controls leg motion.[41]
Mechanism of action
From the Biot–Savart law
 .
.The exact details of how TMS functions are still being explored. The effects of TMS can be divided into two types depending on the mode of stimulation:
- Single or paired pulse TMS causes neurons in the neocortex under the site of stimulation to depolarize and discharge an action potential. If used in the primary motor cortex, it produces muscle activity referred to as a motor evoked potential (MEP) which can be recorded on electromyography. If used on the occipital cortex, 'phosphenes' (flashes of light) might be perceived by the subject. In most other areas of the cortex, the participant does not consciously experience any effect, but his or her behaviour may be slightly altered (e.g., slower reaction time on a cognitive task), or changes in brain activity may be detected using sensing equipment.[43]
- Repetitive TMS produces longer-lasting effects which persist past the initial period of stimulation. rTMS can increase or decrease the excitability of the corticospinal tract depending on the intensity of stimulation, coil orientation, and frequency. The mechanism of these effects is not clear, though it is widely believed to reflect changes in synaptic efficacy akin to long-term potentiation (LTP) and long-term depression (LTD).[44]
Coil types
The design of transcranial magnetic stimulation coils used in either treatment or diagnostic/experimental studies may differ in a variety of ways. These differences should be considered in the interpretation of any study result, and the type of coil used should be specified in the study methods for any published reports.The most important considerations include:
- the type of material used to construct the core of the coil
- the geometry of the coil configuration
- the biophysical characteristics of the pulse produced by the coil.
A number of different types of coils exist, each of which produce different magnetic field patterns. Some examples:
- round coil: the original type of TMS coil
- figure-eight coil (i.e., butterfly coil): results in a more focal pattern of activation
- double-cone coil: conforms to shape of head, useful for deeper stimulation
- four-leaf coil: for focal stimulation of peripheral nerves[49]
- H-coil: for deep transcranial magnetic stimulation
History
Early attempts at stimulation of the brain using a magnetic field included those, in 1896, of Jacques-Arsène d'Arsonval in Paris and in 1910, of Silvanus P. Thompson in London.[citation needed] The principle of inductive brain stimulation with eddy currents has been noted since the 20th century[citation needed]. The first successful TMS study was performed in 1985 by Anthony Barker and his colleagues at the Royal Hallamshire Hospital in Sheffield, England.[50][non-primary source needed] Its earliest application demonstrated conduction of nerve impulses from the motor cortex to the spinal cord, stimulating muscle contractions in the hand. As compared to the previous method of transcranial stimulation proposed by Merton and Morton in 1980[51]{{primary-inline} in which direct electric current was applied to the scalp, the use of electromagnets greatly reduced the discomfort of the procedure, and allowed mapping of the cerebral cortex and its connections.Research
TMS research in animal studies is limited due to early FDA approval of TMS treatment of drug-resistant depression. Because of this, there has been no specific coils for animal models. Hence, there are limited number of TMS coils that can be used for animal studies.[52] There are some attempts in the literature showing new coil designs for mice with an improved stimulation profile.[53]Areas of research include:
- rehabilitation of aphasia and motor disability after stroke,[4][7][11][12][54]
- tinnitus,[4][55]
- anxiety disorders,[4] including panic disorder[56] and obsessive-compulsive disorder.[4] The most promising areas to target for OCD appear to be the orbitofrontal cortex and the supplementary motor area.[57] Older protocols that targeted the prefrontal dorsal cortex were less successful in treating OCD.[58]
- amyotrophic lateral sclerosis,[4][59]
- multiple sclerosis,[4]
- epilepsy,[4][60]
- Alzheimer's disease,[4]
- Parkinson's disease,[61]
- schizophrenia,[4][6]
- substance abuse,[4] addiction,[4][62] and posttraumatic stress disorder (PTSD).[4][63]
- autism[64]
- brain death, coma, and other persistent vegetative states.[4]
- Functional connectivity between the cerebellum and other areas of the brain[65]
Study blinding
It is difficult to establish a convincing form of "sham" TMS to test for placebo effects during controlled trials in conscious individuals, due to the neck pain, headache and twitching in the scalp or upper face associated with the intervention.[4][7] "Sham" TMS manipulations can affect cerebral glucose metabolism and MEPs, which may confound results.[66] This problem is exacerbated when using subjective measures of improvement.[7] Placebo responses in trials of rTMS in major depression are negatively associated with refractoriness to treatment, vary among studies and can influence results.[67]A 2011 review found that only 13.5% of 96 randomized control studies of rTMS to the dorsolateral prefrontal cortex had reported blinding success and that, in those studies, people in real rTMS groups were significantly more likely to think that they had received real TMS, compared with those in sham rTMS groups.[68] Depending on the research question asked and the experimental design, matching the discomfort of rTMS to distinguish true effects from placebo can be an important and challenging issue.[4][7][8][9]