 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˈsɪmvəstætɪn/ |
| Trade names | Zocor, other |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a692030 |
| License data |
|
| Pregnancy category | |
| Routes of administration | by mouth |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 5% |
| Protein binding | 95% |
| Metabolism | Hepatic (CYP3A4) |
| Elimination half-life | 2 hours for simvastatin and 1.9 hours for simvastatin acid |
| Excretion | Renal 13%, faecal 60% |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.115.749 |
| Chemical and physical data | |
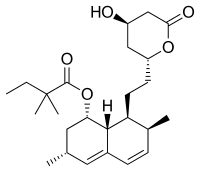
| Formula | C25H38O5 |
| Molar mass | 418.574 g·mol−1 |
| 3D model (JSmol) | |
Simvastatin, marketed under the trade name Zocor among others, is a lipid-lowering medication. It is used along with exercise, diet, and weight loss to decrease elevated lipid levels. It is also used to decrease the risk of heart problems in those at high risk. It is taken by mouth.
Common side effects include constipation, headaches, and nausea. Serious side effects may include muscle breakdown, liver problems, and increased blood sugar levels. A lower dose may be needed in people with kidney problems. There is evidence of harm to the developing baby when taken during pregnancy and it should not be used by those who are breastfeeding. It is in the statin class of medications and works by decreasing the manufacture of cholesterol by the liver.
Simvastatin was patented by Merck in 1980, and came into medical use in 1992. It is on the World Health Organization's List of Essential Medicines. It is available as a generic medication and at a relatively low cost. Simvastatin is made from the fungus Aspergillus terreus. In 2017, it was the eighth most commonly prescribed medication in the United States, with more than 56 million prescriptions.
Medical uses
The primary uses of simvastatin are to treat dyslipidemia and to prevent atherosclerosis-related complications such as stroke and heart attacks in those who are at high risk. It is recommended to be used as an addition to a low-cholesterol diet.
In the Scandinavian Simvastatin Survival Study
(a placebo-controlled, randomized clinical trial of five years'
duration), simvastatin reduced overall mortality in people with existing
cardiovascular disease and high LDL cholesterol by 30% and reduced
cardiovascular mortality by 42%.
The risks of heart attack, stroke, or needing a coronary
revascularization procedure were reduced by 37%, 28%, and 37%,
respectively.
The Heart Protection Study
evaluated the effects of simvastatin in people with risk factors
including existing cardiovascular disease, diabetes, or stroke, but
having relatively low LDL cholesterol. In this trial, which lasted 5.4
years, overall mortality was reduced by 13% and cardiovascular mortality
was reduced by 18%. People receiving simvastatin experienced 38% fewer
nonfatal heart attacks and 25% fewer strokes.
Simvastatin has been used to explore whether statins have an effect on delaying on the onset and progression of age-related macular degeneration (AMD).
Results from one trial showed participants assigned to simvastatin had
lower odds (0.51 OR) of having AMD progression at three years compared
to those assigned to placebo, though the results were not significant. Overall, evidence is insufficient to conclude that simvastatin has an effect in delaying the onset and progression of AMD.
Contraindications
Simvastatin is contraindicated with pregnancy, breastfeeding, and liver disease.
Pregnancy must be avoided while on simvastatin due to potentially
severe birth defects. Patients cannot breastfeed while on simvastatin
due to potentially disrupting the infant's lipid metabolism. High doses of simvastatin are also contraindicated with the widely used antihypertensive amlodipine. A lower dose is also recommended in people taking the calcium channel blockers, verapamil and diltiazem, as well as those taking amiodarone.
Adverse effects
Common
side effects (>1% incidence) may include indigestion and eczema.
Rare side effects include joint pain, memory loss, and muscle cramps.
Cholestatic hepatitis, hepatic cirrhosis, rhabdomyolysis (destruction
of muscles and blockade of renal system), and myositis have been
reported in patients receiving the drug chronically. Serious allergic reactions to simvastatin are rare.
If the following signs of a serious allergic reaction occur, seek
medical attention immediately: rash, hoarseness itching/swelling,
dizziness, or difficulty swallowing/breathing.
A type of DNA variant known as a single nucleotide polymorphism (SNP) may help predict individuals prone to developing myopathy when taking simvastatin; a study ultimately including 32,000 patients concluded the carriers of one or two risk alleles of a particular SNP, rs4149056, were at a five-fold or 16-fold increased risk, respectively.
In 2012, the Clinical Pharmacogenetics Implementation Consortium has
released guidelines regarding the use of rs4149056 genotype in guiding
dosing of simvastatin and updated the guideline in 2014.
In March 2012, the U.S. Food and Drug Administration
(FDA) updated its guidance for statin users to address reports of
memory loss, liver damage, increased blood sugar, development of type 2 diabetes, and muscle injury. The new guidance indicates:
- FDA has found that liver injury associated with statin use is rare but can occur.
- The reports about memory loss, forgetfulness, and confusion span all statin products and all age groups. The FDA says these experiences are rare, but that those affected often report feeling "fuzzy" or unfocused in their thinking.
- A small increased risk of raised blood sugar levels and the development of type 2 diabetes have been reported with the use of statins.
- Some drugs interact with statins in a way that increases the risk of muscle injury called myopathy, characterized by unexplained muscle weakness or pain.
On 19 March 2010, the FDA issued another statement regarding
simvastatin, saying it increases the risk of muscle injury (myopathy)
when taken at high doses or at lower doses in combination with other
drugs.
The highest dose rate causes muscle damage in 610 of every 10,000
people in contrast to a lower dose, which causes muscle damage in eight
of 10,000 people.
The FDA warning, released again on 8 June 2011, suggested that
high-dose "simvastatin should be used only in patients who have been
taking this dose for 12 months or more without evidence of muscle
injury" and that it "should not be started in new patients, including
patients already taking lower doses of the drug."
Interactions
Simvastatin has important interactions with grapefruit
juice and other drugs, including some that are commonly used for the
treatment of cardiovascular disease. These interactions are clinically
important because increasing simvastatin serum levels above those
normally provided by the maximum recommended dose increases the risk of
muscle damage, including the otherwise rare and potentially fatal side
effect of rhabdomyolysis.
Consuming large amounts of grapefruit juice increases serum
levels of simvastatin by up to three-fold, increasing the risk of side
effects. The FDA recommends that people taking statins should avoid consuming more than a quart (946 ml) of grapefruit juice per day.
Simvastatin also interacts with other drugs, including some used
to treat cardiovascular problems. It should not be taken by people who
are also taking the antifungal drugs fluconazole, itraconazole, or posaconazole; the antibiotics erythromycin, clarithromycin, or telithromycin; HIV protease inhibitors; the antidepressant nefazodone; the cardiovascular drug gemfibrozil; the immunosuppressant ciclosporin, or the endometriosis drug danazol. Reduced maximum doses of simvastatin apply for patients taking certain other drugs, including the cardiovascular drugs verapamil, diltiazem, amiodarone, amlodipine, and ranolazine.
Pharmacology
All statins act by inhibiting 3-hydroxy-3-methylglutaryl (HMG) coenzyme A reductase. HMG-CoA reductase, the rate-limiting enzyme of the HMG-CoA reductase pathway, the metabolic pathway responsible for the endogenous production of cholesterol. Statins are more effective than other lipid-regulating drugs at lowering LDL-cholesterol concentration, but they are less effective than the fibrates
in reducing triglyceride concentration. However, statins reduce
cardiovascular disease events and total mortality irrespective of the
initial cholesterol concentration. This is a major piece of evidence
that statins work in another way than the lowering of cholesterol
(called pleiotropic effects).
The drug is in the form of an inactive lactone that is hydrolyzed after ingestion to produce the active agent. It is a white, nonhygroscopic, crystalline powder that is practically insoluble in water, and freely soluble in chloroform, methanol, and ethanol.
Simvastatin is an effective serum lipid-lowering drug that can decrease low density lipoprotein (LDL) levels by up to 50%. Simvastatin had been shown to interact with lipid-lowering transcription factor PPAR-alpha and that interaction might control the neurotrophic action of the drug.
History
The development of simvastatin was closely linked with lovastatin. Biochemist Jesse Huff and his colleagues at Merck began researching the biosynthesis of cholesterol in the early 1950s.[35] In 1956, mevalonic acid was isolated from a yeast extract by Karl Folkers,
Carl Hoffman, and others at Merck, while Huff and his associates
confirmed that mevalonic acid was an intermediate in cholesterol
biosynthesis. In 1959, the HMG-CoA reductase enzyme (a major contributor of internal cholesterol production) was discovered by researchers at the Max Planck Institute. This discovery encouraged scientists worldwide to find an effective inhibitor of this enzyme.
By 1976, Akira Endo had isolated the first inhibitor, mevastatin, from the fungus Penicillium citrinium while working at Daiichi Sankyo in Japan. In 1979, Hoffman and colleagues isolated lovastatin from a strain of the fungus Aspergillus terreus.
While developing and researching lovastatin, Merck scientists
synthetically derived a more potent HMG-CoA reductase inhibitor from a
fermentation product of A. terreus, which was designated MK-733 (later to be named simvastatin).
In 1994, publication of the results of the Scandinavian Simvastatin Survival Study
(4S) provided the first unequivocal evidence that lowering LDL
cholesterol via statin treatment reduces cardiovascular events and
overall mortality. A total of 4,444 people with coronary heart disease
5.5 to 8.0 mmol/L were randomized to simvastatin treatment or placebo
and followed for an average of 5 years. Compared to the placebo group,
those treated with simvastatin experienced a 30% decrease in overall
mortality, a 42% reduction in coronary death, a 34% reduction in major
coronary events, and a 37% reduction in revascularization procedures.
Society and culture
Cost
Simvastatin is relatively inexpensive. The wholesale cost in some LMIC is around US$0.01 to 0.15 per 20 mg dose as of 2014. The defined daily dose is 30 mg per the World Health Organization. The price decreased from roughly US$1,200 to $40 per year of medication in LMIC following the patent expiring in 2006. In the United States, it costs about US$10 to 20 per month since patent protection ended. In the UK in 2008, the typical per-patient cost to the NHS of simvastatin was about £1.50 per month. (40 mg/day costs UK NHS £1.37/month in 2012) The price in Canada is about $CAD 130 to 160 per year as of 2016. Under provisions of the Patient Protection and Affordable Care Act (PPACA) in the United States, there is no cost for simvastatin 10 mg, 20 mg, and 40 mg for adults aged 40–75 years based on United States Preventive Services Task Force (USPSTF) recommendations.
Economics
Simvastatin was introduced in the late 1980s, and since 2006 in many countries, it is available as a generic
preparation. This has led to a decrease of the price of most statin
drugs, and a reappraisal of the health economics of preventive statin
treatment.
Prior to losing U.S. patent protection, simvastatin was Merck
& Co.'s largest-selling drug and second-largest selling
cholesterol-lowering drug in the world. In 2005, recorded US$3.1 billion of sales in the United States and US$4.4 billion worldwide.
Zocor had an original patent expiry date of 24 December 2005 but was extended by the United States Patent and Trademark Office (USPTO) to expire on 23 June 2006.
The USPTO granted the patent extension after Merck submitted data from
studies of the drug's positive effect on children. In the UK, the patent
for simvastatin had expired by 2004.
In the UK, simvastatin was the most prescribed medication in the
community in 2013, with 39.9 million items dispensed. This compares to
30.9 million items for aspirin, and 27.7 million for levothyroxine sodium, the second- and third-most prescribed drugs in the UK in 2013.
Marketing
Simvastatin was initially marketed by Merck & Co
under the trade name Zocor but is available generically in most
countries following the patent expiry. A combination of simvastatin
along with ezetimibe is sold under the brand name Vytorin and is jointly marketed by Merck and Schering-Plough.
Brand names include Zocor, Zocor Heart Pro, marketed by the pharmaceutical company
Merck & Co., Simlup, Simvotin, Simcard [India], Denan (Germany),
Liponorm, Sinvacor, Sivastin (Italy), Lipovas (Japan), Lodales (France),
Zocord (Austria and Sweden), Zimstat, Simvahexal (Australia), Lipex
(Australia and New Zealand), Simvastatin-Teva, Simvacor, Simvaxon,
Simovil (Israel), available in Thailand under the brand Bestatin
manufactured by Berlin Pharmaceutical Industry Co Ltd and others.
The U.S. patent for Zocor expired on 23 June 2006. Ranbaxy Laboratories (at the 80-mg strength) and Teva Pharmaceutical Industries
through its Ivax Pharmaceuticals unit (at all other strengths) were
given approval by the FDA to manufacture and sell simvastatin as a generic drug with 180-day exclusivity. Dr. Reddy's Laboratories also has a license from Merck & Co. to sell simvastatin as an authorized generic drug.
