| Traditional Chinese medicine | |
| Traditional Chinese | 中醫 |
|---|---|
| Simplified Chinese | 中医 |
| Literal meaning | "Chinese medicine" |
Traditional Chinese medicine (TCM; simplified Chinese: 中医; traditional Chinese: 中醫; pinyin: Zhōngyī) is a style of traditional medicine based on more than 2,500 years of Chinese medical practice that includes various forms of herbal medicine, acupuncture, massage (tui na), exercise (qigong), and dietary therapy, but recently also influenced by modern Western medicine. TCM is widely used in Greater China where it has a long history, and recently it has begun "gaining global recognition". One of the basic tenets of TCM is that "the body's vital energy (ch'i or qi) circulates through channels, called meridians, that have branches connected to bodily organs and functions."
Concepts of the body and of disease used in TCM reflect its ancient
origins and its emphasis on dynamic processes over material structure,
similar to European humoral theory.
Scientific investigation has not found evidence for traditional Chinese concepts such as qi, meridians, and acupuncture points. The TCM theory and practice are not based upon scientific knowledge, and there is disagreement between TCM practitioners on what diagnosis and treatments should be used for any given patient. The effectiveness of Chinese herbal medicine remains poorly researched and supported. There are concerns over a number of potentially toxic plants, animal parts, and mineral Chinese medicinals.
There are also concerns over illegal trade and transport of endangered
species including rhinoceroses and tigers, and the welfare of specially
farmed animals including bears. A review of cost-effectiveness research for TCM found that studies had low levels of evidence, but so far have not shown benefit outcomes.
Pharmaceutical research has explored the potential for creating new
drugs from traditional remedies, with few successful results. A Nature editorial described TCM as "fraught with pseudoscience", and said that the most obvious reason it hasn't delivered many cures is that the majority of its treatments have no logical mechanism of action.
Proponents propose that research has so far missed key features of the
art of TCM, such as unknown interactions between various ingredients and
complex interactive biological systems.
The doctrines of Chinese medicine are rooted in books such as the Yellow Emperor's Inner Canon and the Treatise on Cold Damage, as well as in cosmological notions such as yin-yang and the five phases.
Starting in the 1950s, these precepts were standardized in the People's
Republic of China, including attempts to integrate them with modern
notions of anatomy and pathology. In the 1950s, the Chinese government promoted a systematized form of TCM.
TCM describes health as the harmonious interaction of these
entities and the outside world, and disease as a disharmony in
interaction. TCM diagnosis aims to trace symptoms to patterns
of an underlying disharmony, by measuring the pulse, inspecting the
tongue, skin, and eyes, and looking at the eating and sleeping habits of
the person as well as many other things.
History
The Compendium of Materia Medica is a pharmaceutical text written by Li Shizhen (1518–1593 AD) during the Ming Dynasty of China. This edition was published in 1593.
Acupuncture chart from Hua Shou (fl. 1340s, Yuan Dynasty). This image from Shi si jing fa hui (Expression of the Fourteen Meridians). (Tokyo: Suharaya Heisuke kanko, Kyoho gan 1716).
Traces of therapeutic activities in China date from the Shang dynasty (14th–11th centuries BCE). Though the Shang did not have a concept of "medicine" as distinct from other fields, their oracular inscriptions on bones and tortoise shells refer to illnesses that affected the Shang royal family: eye disorders, toothaches, bloated abdomen, etc., which Shang elites usually attributed to curses sent by their ancestors. There is no evidence that the Shang nobility used herbal remedies.
According to a 2006 overview, the "Documentation of Chinese materia
medica (CMM) dates back to around 1,100 BCE when only dozens of drugs
were first described. By the end of the 16th century, the number of
drugs documented had reached close to 1,900. And by the end of the last
century, published records of CMM had reached 12,800 drugs."
Stone and bone needles found in ancient tombs led Joseph Needham to speculate that acupuncture might have been carried out in the Shang dynasty. This being said, most historians now make a distinction between medical lancing (or bloodletting) and acupuncture in the narrower sense of using metal needles to treat illnesses by stimulating specific points along circulation channels ("meridians") in accordance with theories related to the circulation of Qi. The earliest evidence for acupuncture in this sense dates to the second or first century BCE.
The Yellow Emperor's Inner Canon (Huang Di Nei Jing), the
oldest received work of Chinese medical theory, was compiled around the
first century BCE on the basis of shorter texts from different medical
lineages. Written in the form of dialogues between the legendary Yellow Emperor and his ministers, it offers explanations on the relation between humans, their environment, and the cosmos, on the contents of the body, on human vitality and pathology, on the symptoms of illness, and on how to make diagnostic and therapeutic decisions in light of all these factors. Unlike earlier texts like Recipes for Fifty-Two Ailments, which was excavated in the 1970s from a tomb that had been sealed in 168 BCE, the Inner Canon rejected the influence of spirits and the use of magic.
It was also one of the first books in which the cosmological doctrines
of Yinyang and the Five Phases were brought to a mature synthesis.
The Treatise on Cold Damage Disorders and Miscellaneous Illnesses (Shang Han Lun) was collated by Zhang Zhongjing sometime between 196 and 220 CE; at the end of the Han dynasty. Focusing on drug prescriptions rather than acupuncture, it was the first medical work to combine Yinyang and the Five Phases with drug therapy. This formulary was also the earliest public Chinese medical text to group symptoms into clinically useful "patterns" (zheng
證) that could serve as targets for therapy. Having gone through
numerous changes over time, the formulary now circulates as two distinct
books: the Treatise on Cold Damage Disorders and the Essential Prescriptions of the Golden Casket, which were edited separately in the eleventh century, under the Song dynasty.
In the centuries that followed, several shorter books tried to summarize or systematize its contents of the book Yellow Emperor's Inner Canon. The Canon of Problems (probably second century CE) tried to reconcile divergent doctrines from the Inner Canon and developed a complete medical system centered on needling therapy. The AB Canon of Acupuncture and Moxibustion (Zhenjiu jiayi jing 針灸甲乙經, compiled by Huangfu Mi sometime between 256 and 282 CE) assembled a consistent body of doctrines concerning acupuncture; whereas the Canon of the Pulse (Maijing 脈經; ca. 280) presented itself as a "comprehensive handbook of diagnostics and therapy."
In 1950, Chairman Mao Zedong made a speech in support of traditional Chinese medicine (TCM) which was influenced by political necessity. Mao believed he and the Chinese Communist Party should promote TCM but he did not personally believe in TCM and he did not use it. In 1952, the president of the Chinese Medical Association
said that, "This One Medicine, will possess a basis in modern natural
sciences, will have absorbed the ancient and the new, the Chinese and
the foreign, all medical achievements—and will be China’s New Medicine!"
Historical physicians
Philosophical background
Traditional
Chinese medicine (TCM) is a broad range of medicine practices sharing
common concepts which have been developed in China and are based on a
tradition of more than 2,000 years, including various forms of herbal medicine, acupuncture, massage (Tui na), exercise (qigong), and dietary therapy. It is primarily used as a complementary alternative medicine approach. TCM is widely used in China and it is also used in the West. Its philosophy is based on Yinyangism (i.e., the combination of Five Phases theory with Yin-yang theory), which was later absorbed by Daoism.
Yin and yang
Yin and yang are ancient Chinese concepts which can be traced back to the Shang dynasty
(1600–1100 BC). They represent two abstract and complementary aspects
that every phenomenon in the universe can be divided into. Primordial analogies for these aspects are the sun-facing (yang) and the shady (yin) side of a hill. Two other commonly used representational allegories of yin and yang are water and fire. In the yin-yang theory, detailed attributions are made regarding the yin or yang character of things:
| Phenomenon | Yin | Yang |
|---|---|---|
| Celestial bodies | moon | sun |
| Gender | female | male |
| Location | inside | outside |
| Temperature | cold | hot |
| Direction | downward | upward |
| Degree of humidity | damp/moist | dry |
The concept of yin and yang is also applicable to the human body; for
example, the upper part of the body and the back are assigned to yang,
while the lower part of the body are believed to have the yin character.
Yin and yang characterization also extends to the various body
functions, and – more importantly – to disease symptoms (e.g., cold and
heat sensations are assumed to be yin and yang symptoms, respectively).
Thus, yin and yang of the body are seen as phenomena whose lack (or
over-abundance) comes with characteristic symptom combinations:
- Yang vacuity (also termed "vacuity-heat"): heat sensations, possible sweating at night, insomnia, dry pharynx, dry mouth, dark urine, and a "fine" and rapid pulse.
- Yin vacuity ("vacuity-cold"): aversion to cold, cold limbs, bright white complexion, long voidings of clear urine, diarrhea, pale and enlarged tongue, and a slightly weak, slow and fine pulse.
TCM also identifies drugs believed to treat these specific symptom combinations, i.e., to reinforce yin and yang.
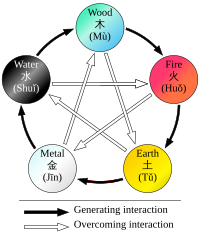
Interactions of Wu Xing
Five Phases theory
Five Phases (五行, pinyin: wǔ xíng), sometimes also translated as the "Five Elements"
theory, presumes that all phenomena of the universe and nature can be
broken down into five elemental qualities – represented by wood (木, pinyin: mù), fire (火pinyin: huǒ), earth (土, pinyin: tǔ), metal (金, pinyin: jīn), and water (水, pinyin: shuǐ). In this way, lines of correspondence can be drawn:
| Phenomenon | Wood | Fire | Earth | Metal | Water |
|---|---|---|---|---|---|
| Direction | East | South | Centre | West | North |
| Color | green/violet | red/purple | yellow/pink | white | black |
| Climate | wind | heat | damp | dryness | cold |
| Taste | sour | bitter | sweet | acrid | salty |
| Zang Organ | Liver | Heart | Spleen | Lung | Kidney |
| Fu Organ | Gallbladder | Small intestine | Stomach | Large intestine | Bladder |
| Sense organ | eye | tongue | mouth | nose | ears |
| Facial part | above bridge of nose | between eyes, lower part | bridge of nose | between eyes, middle part | cheeks (below cheekbone) |
| Eye part | iris | inner/outer corner of the eye | upper and lower lid | sclera | pupil |
Strict rules are identified to apply to the relationships between the
Five Phases in terms of sequence, of acting on each other, of
counteraction, etc. All these aspects of Five Phases theory constitute the basis of the zàng-fǔ concept, and thus have great influence regarding the TCM model of the body. Five Phase theory is also applied in diagnosis and therapy.
Correspondences between the body and the universe have
historically not only been seen in terms of the Five Elements, but also
of the "Great Numbers" (大數, pinyin: dà shū)
For example, the number of acu-points has at times been seen to be 365,
corresponding with the number of days in a year; and the number of main
meridians–12–has been seen as corresponding with the number of rivers
flowing through the ancient Chinese empire.
Model of the body
Old Chinese medical chart on acupuncture meridians
TCM "holds that the body's vital energy (chi or qi) circulates through channels, called meridians, that have branches connected to bodily organs and functions." Its view of the human body is only marginally concerned with anatomical structures, but focuses primarily on the body's functions (such as digestion, breathing, temperature maintenance, etc.):
The tendency of Chinese thought is to seek out dynamic functional activity rather than to look for the fixed somatic structures that perform the activities. Because of this, the Chinese have no system of anatomy comparable to that of the West.
— Ted Kaptchuk, The Web That Has No Weaver
These functions are aggregated and then associated with a primary
functional entity – for instance, nourishment of the tissues and
maintenance of their moisture are seen as connected functions, and the
entity postulated to be responsible for these functions is xuě (blood). These functional entities thus constitute concepts rather than something with biochemical or anatomical properties.
The primary functional entities used by traditional Chinese
medicine are qì, xuě, the five zàng organs, the six fǔ organs, and the
meridians which extend through the organ systems.
These are all theoretically interconnected: each zàng organ is paired
with a fǔ organ, which are nourished by the blood and concentrate qi for
a particular function, with meridians being extensions of those
functional systems throughout the body.
Concepts of the body and of disease used in TCM have notions of a pre-scientific culture, similar to European humoral theory. TCM is characterized as full of pseudoscience. Some practitioners no longer consider yin and yang and the idea of an energy flow to apply. Scientific investigation has not found any histological or physiological evidence for traditional Chinese concepts such as qi, meridians, and acupuncture points.
It is a generally held belief within the acupuncture community that
acupuncture points and meridians structures are special conduits for
electrical signals but no research has established any consistent
anatomical structure or function for either acupuncture points or
meridians. The scientific evidence for the anatomical existence of either meridians or acupuncture points is not compelling. Stephen Barrett of Quackwatch
writes that, "TCM theory and practice are not based upon the body of
knowledge related to health, disease, and health care that has been
widely accepted by the scientific community. TCM practitioners disagree
among themselves about how to diagnose patients and which treatments
should go with which diagnoses. Even if they could agree, the TCM
theories are so nebulous that no amount of scientific study will enable
TCM to offer rational care."
TCM has been the subject of controversy within China. In 2006, the Chinese scholar Zhang Gongyao
triggered a national debate when he published an article entitled
"Farewell to Traditional Chinese Medicine," arguing that TCM was a
pseudoscience that should be abolished in public healthcare and
academia.
The Chinese government however, interested in the opportunity of export
revenues, took the stance that TCM is a science and continued to
encourage its development.
Qi
TCM distinguishes many kinds of qi (simplified Chinese: 气; traditional Chinese: 氣; pinyin: qì). In a general sense, qi is something that is defined by five "cardinal functions":
- Actuation (simplified Chinese: 推动; traditional Chinese: 推動; pinyin: tuīdòng) – of all physical processes in the body, especially the circulation of all body fluids such as blood in their vessels. This includes actuation of the functions of the zang-fu organs and meridians.
- Warming (Chinese: 溫煦; pinyin: wēnxù) – the body, especially the limbs.
- Defense (Chinese: 防御; pinyin: fángyù) – against Exogenous Pathogenic Factors
- Containment (simplified Chinese: 固摄; traditional Chinese: 固攝; pinyin: gùshè) – of body fluids, i.e., keeping blood, sweat, urine, semen, etc. from leakage or excessive emission.
- Transformation (simplified Chinese: 气化; traditional Chinese: 氣化; pinyin: qìhuà) – of food, drink, and breath into qi, xue (blood), and jinye (“fluids”), and/or transformation of all of the latter into each other.
Vacuity of qi will be characterized especially by pale complexion,
lassitude of spirit, lack of strength, spontaneous sweating, laziness to
speak, non-digestion of food, shortness of breath (especially on
exertion), and a pale and enlarged tongue.
Qi is believed to be partially generated from food and drink, and
partially from air (by breathing). Another considerable part of it is
inherited from the parents and will be consumed in the course of life.
TCM uses special terms for qi running inside of the blood vessels
and for qi that is distributed in the skin, muscles, and tissues
between those. The former is called yíng-qì (simplified Chinese: 营气; traditional Chinese: 營氣); its function is to complement xuè and its nature has a strong yin aspect (although qi in general is considered to be yang). The latter is called weì-qì (simplified Chinese: 卫气; traditional Chinese: 衛氣); its main function is defense and it has pronounced yang nature.
Qi is said to circulate in the meridians. Just as the qi held by
each of the zang-fu organs, this is considered to be part of the
'principal' qi (simplified Chinese: 元气; traditional Chinese: 元氣; pinyin: yuánqì) of the body (also called 真氣 Chinese: 真气; pinyin: zhēn qì, ‘’true‘’ qi, or 原氣 Chinese: 原气; pinyin: yuán qì, ‘’original‘’ qi).
Xue
In contrast to
the majority of other functional entities, xuè (血, "blood") is
correlated with a physical form – the red liquid running in the blood
vessels.
Its concept is, nevertheless, defined by its functions: nourishing all
parts and tissues of the body, safeguarding an adequate degree of
moisture, and sustaining and soothing both consciousness and sleep.
Typical symptoms of a lack of xuě (usually termed "blood vacuity" [血虚, pinyin: xuě xū])
are described as: Pale-white or withered-yellow complexion, dizziness,
flowery vision, palpitations, insomnia, numbness of the extremities;
pale tongue; "fine" pulse.
Jinye
Closely
related to xuě are the jīnyė (津液, usually translated as "body fluids"),
and just like xuě they are considered to be yin in nature, and defined
first and foremost by the functions of nurturing and moisturizing the
different structures of the body. Their other functions are to harmonize yin and yang, and to help with the secretion of waste products.
Jīnyė are ultimately extracted from food and drink, and
constitute the raw material for the production of xuě; conversely, xuě
can also be transformed into jīnyė. Their palpable manifestations are all bodily fluids: tears, sputum, saliva, gastric acid, joint fluid, sweat, urine, etc.
Zang-fu
The zàng-fǔ (simplified Chinese: 脏腑; traditional Chinese: 臟腑)
constitute the centre piece of TCM's systematization of bodily
functions. Bearing the names of organs, they are, however, only
secondarily tied to (rudimentary) anatomical assumptions (the fǔ a
little more, the zàng much less). As they are primarily defined by their functions, they are not equivalent to the anatomical organs–to highlight this fact, their names are usually capitalized.
The term zàng (臟) refers to the five entities considered to be yin in nature–Heart, Liver, Spleen, Lung, Kidney–, while fǔ (腑) refers to the six yang organs–Small Intestine, Large Intestine, Gallbladder, Urinary Bladder, Stomach and Sānjiaō.
The zàng's essential functions consist in production and storage
of qì and xuě; they are said to regulate digestion, breathing, water
metabolism, the musculoskeletal system, the skin, the sense organs,
aging, emotional processes, and mental activity, among other structures
and processes. The fǔ organs' main purpose is merely to transmit and digest (傳化, pinyin: chuán-huà) substances such as waste and food.
Since their concept was developed on the basis of Wǔ Xíng
philosophy, each zàng is paired with a fǔ, and each zàng-fǔ pair is
assigned to one of five elemental qualities (i.e., the Five Elements or
Five Phases). These correspondences are stipulated as:
- Fire (火) = Heart (心, pinyin: xīn) and Small Intestine (小腸, pinyin: xiaǒcháng) (and, secondarily, Sānjiaō [三焦, "Triple Burner"] and Pericardium [心包, pinyin: xīnbaò])
- Earth (土) = Spleen (脾, pinyin: pí) and Stomach (胃, pinyin: weì)
- Metal (金) = Lung (肺, pinyin: feì) and Large Intestine (大腸, pinyin: dàcháng)
- Water (水) = Kidney (腎, pinyin: shèn) and Bladder (膀胱, pinyin: pángguāng)
- Wood (木) = Liver (肝, pinyin: gān) and Gallbladder (膽, pinyin: dān)
The zàng-fǔ are also connected to the twelve standard meridians–each yang meridian is attached to a fǔ organ, and five of the yin meridians are attached to a zàng. As there are only five zàng but six yin meridians, the sixth is assigned to the Pericardium, a peculiar entity almost similar to the Heart zàng.
Jing-luo
Acupuncture chart from the Ming Dynasty (c. 1368–1644)
The meridians (经络, pinyin: jīng-luò) are believed to be channels running from the zàng-fǔ in the interior (里, pinyin: lǐ) of the body to the limbs and joints ("the surface" [表, pinyin: biaǒ]), transporting qi and xuĕ. TCM identifies 12 "regular" and 8 "extraordinary" meridians; the Chinese terms being 十二经脉 (pinyin: shí-èr jīngmài, lit. "the Twelve Vessels") and 奇经八脉 (pinyin: qí jīng bā mài) respectively. There's also a number of less customary channels branching from the "regular" meridians.
Concept of disease
In
general, disease is perceived as a disharmony (or imbalance) in the
functions or interactions of yin, yang, qi, xuĕ, zàng-fǔ, meridians etc.
and/or of the interaction between the human body and the environment. Therapy is based on which "pattern of disharmony" can be identified. Thus, "pattern discrimination" is the most important step in TCM diagnosis. It is also known to be the most difficult aspect of practicing TCM.
In order to determine which pattern is at hand, practitioners
will examine things like the color and shape of the tongue, the relative
strength of pulse-points, the smell of the breath, the quality of
breathing or the sound of the voice.
For example, depending on tongue and pulse conditions, a TCM
practitioner might diagnose bleeding from the mouth and nose as: "Liver
fire rushes upwards and scorches the Lung, injuring the blood vessels
and giving rise to reckless pouring of blood from the mouth and nose." He might then go on to prescribe treatments designed to clear heat or supplement the Lung.
Disease entities
In TCM, a disease has two aspects: "bìng" and "zhèng". The former is often translated as "disease entity", "disease category", "illness", or simply "diagnosis". The latter, and more important one, is usually translated as "pattern" (or sometimes also as "syndrome"). For example, the disease entity of a common cold might present with a pattern of wind-cold in one person, and with the pattern of wind-heat in another.
From a scientific point of view, most of the disease entitites (病, pinyin: bìng) listed by TCM constitute mere symptoms. Examples include headache, cough, abdominal pain, constipation etc.
Since therapy will not be chosen according to the disease entity
but according to the pattern, two people with the same disease entity
but different patterns will receive different therapy.
Vice versa, people with similar patterns might receive similar therapy
even if their disease entities are different. This is called 异病同治,同病异治 (pinyin: yì bìng tóng zhì, tóng bìng yì zhì,"different diseases, same treatment; same disease, different treatments").
Patterns
In TCM, "pattern" (证, pinyin: zhèng)
refers to a "pattern of disharmony" or "functional disturbance" within
the functional entities the TCM model of the body is composed of. There are disharmony patterns of qi, xuě, the body fluids, the zàng-fǔ, and the meridians. They are ultimately defined by their symptoms and "signs" (i.e., for example, pulse and tongue findings).
In clinical practice, the identified pattern usually involves a combination of affected entities (compare with typical examples of patterns). The concrete pattern identified should account for all the symptoms a person has.
Six Excesses
The Six Excesses (六淫, pinyin: liù yín, sometimes also translated as "Pathogenic Factors", or "Six Pernicious Influences"; with the alternative term of 六邪, pinyin: liù xié, – "Six Evils" or "Six Devils") are allegorical terms used to describe disharmony patterns displaying certain typical symptoms. These symptoms resemble the effects of six climatic factors. In the allegory, these symptoms can occur because one or more of those climatic factors (called 六气, pinyin: liù qì, "the six qi") were able to invade the body surface and to proceed to the interior.
This is sometimes used to draw causal relationships (i.e., prior
exposure to wind/cold/etc. is identified as the cause of a disease), while other authors explicitly deny a direct cause-effect relationship between weather conditions and disease, pointing out that the Six Excesses are primarily descriptions of a certain combination of symptoms translated into a pattern of disharmony. It is undisputed, though, that the Six Excesses can manifest inside the body without an external cause. In this case, they might be denoted "internal", e.g., "internal wind" or "internal fire (or heat)".
The Six Excesses and their characteristic clinical signs are:
- Wind (风, pinyin: fēng): rapid onset of symptoms, wandering location of symptoms, itching, nasal congestion, "floating" pulse; tremor, paralysis, convulsion.
- Cold (寒, pinyin: hán): cold sensations, aversion to cold, relief of symptoms by warmth, watery/clear excreta, severe pain, abdominal pain, contracture/hypertonicity of muscles, (slimy) white tongue fur, "deep"/"hidden" or "string-like" pulse, or slow pulse.
- Fire/Heat (火, pinyin: huǒ): aversion to heat, high fever, thirst, concentrated urine, red face, red tongue, yellow tongue fur, rapid pulse. (Fire and heat are basically seen to be the same)
- Dampness (湿, pinyin: shī): sensation of heaviness, sensation of fullness, symptoms of Spleen dysfunction, greasy tongue fur, "slippery" pulse.
- Dryness (燥, pinyin: zào): dry cough, dry mouth, dry throat, dry lips, nosebleeds, dry skin, dry stools.
- Summerheat (暑, pinyin: shǔ): either heat or mixed damp-heat symptoms.
Six-Excesses-patterns can consist of only one or a combination of Excesses (e.g., wind-cold, wind-damp-heat). They can also transform from one into another.
Typical examples of patterns
For
each of the functional entities (qi, xuĕ, zàng-fǔ, meridians etc.),
typical disharmony patterns are recognized; for example: qi vacuity and
qi stagnation in the case of qi; blood vacuity, blood stasis, and blood heat in the case of xuĕ;
Spleen qi vacuity, Spleen yang vacuity, Spleen qi vacuity with
down-bearing qi, Spleen qi vacuity with lack of blood containment,
cold-damp invasion of the Spleen, damp-heat invasion of Spleen and
Stomach in case of the Spleen zàng; wind/cold/damp invasion in the case of the meridians.
TCM gives detailed prescriptions of these patterns regarding
their typical symptoms, mostly including characteristic tongue and/or
pulse findings. For example:
- "Upflaming Liver fire" (肝火上炎, pinyin: gānhuǒ shàng yán): Headache, red face, reddened eyes, dry mouth, nosebleeds, constipation, dry or hard stools, profuse menstruation, sudden tinnitus or deafness, vomiting of sour or bitter fluids, expectoration of blood, irascibility, impatience; red tongue with dry yellow fur; slippery and string-like pulse.
Eight principles of diagnosis
The process of determining which actual pattern is on hand is called 辩证 (pinyin: biàn zhèng, usually translated as "pattern diagnosis", "pattern identification" or "pattern discrimination").
Generally, the first and most important step in pattern diagnosis is an
evaluation of the present signs and symptoms on the basis of the "Eight
Principles" (八纲, pinyin: bā gāng).
These eight principles refer to four pairs of fundamental qualities of a
disease: exterior/interior, heat/cold, vacuity/repletion, and yin/yang. Out of these, heat/cold and vacuity/repletion have the biggest clinical importance.
The yin/yang quality, on the other side, has the smallest importance
and is somewhat seen aside from the other three pairs, since it merely
presents a general and vague conclusion regarding what other qualities
are found. In detail, the Eight Principles refer to the following:
- Yin and yang are universal aspects all things can be classified under, this includes diseases in general as well as the Eight Principles' first three couples. For example, cold is identified to be a yin aspect, while heat is attributed to yang. Since descriptions of patterns in terms of yin and yang lack complexity and clinical practicality, though, patterns are usually not labelled this way anymore. Exceptions are vacuity-cold and repletion-heat patterns, who are sometimes referred to as "yin patterns" and "yang patterns" respectively.
- Exterior (表, pinyin: biǎo) refers to a disease manifesting in the superficial layers of the body – skin, hair, flesh, and meridians. It is characterized by aversion to cold and/or wind, headache, muscle ache, mild fever, a "floating" pulse, and a normal tongue appearance.
- Interior (里, pinyin: lǐ) refers to disease manifestation in the zàng-fǔ, or (in a wider sense) to any disease that can not be counted as exterior. There are no generalized characteristic symptoms of interior patterns, since they'll be determined by the affected zàng or fǔ entity.
- Cold (寒, pinyin: hán) is generally characterized by aversion to cold, absence of thirst, and a white tongue fur. More detailed characterization depends on whether cold is coupled with vacuity or repletion.
- Heat (热, pinyin: rè) is characterized by absence of aversion to cold, a red and painful throat, a dry tongue fur and a rapid and floating pulse, if it falls together with an exterior pattern. In all other cases, symptoms depend on whether heat is coupled with vacuity or repletion.
- Deficiency (虚, pinyin: xū), can be further differentiated into deficiency of qi, xuě, yin and yang, with all their respective characteristic symptoms. Yin deficiency can also cause "empty-heat".
- Excess (实, pinyin: shí) generally refers to any disease that can't be identified as a deficient pattern, and usually indicates the presence of one of the Six Excesses, or a pattern of stagnation (of qi, xuě, etc.). In a concurrent exterior pattern, excess is characterized by the absence of sweating.
After the fundamental nature of a disease in terms of the Eight
Principles is determined, the investigation focuses on more specific
aspects.
By evaluating the present signs and symptoms against the background of
typical disharmony patterns of the various entities, evidence is
collected whether or how specific entities are affected. This evaluation can be done
- in respect of the meridians (经络辩证, pinyin: jīng-luò biàn zhèng)
- in respect of qi (气血辩证, pinyin: qì xuè biàn zhèng)
- in respect of xuè (气血辩证, pinyin: qì xuè biàn zhèng)
- in respect of the body fluids (津液辩证, pinyin: jīn-yė biàn zhèng)
- in respect of the zàng-fǔ (脏腑辩证, pinyin: zàng-fǔ biàn zhèng) – very similar to this, though less specific, is disharmony pattern description in terms of the Five Elements [五行辩证, pinyin: wǔ xíng biàn zhèng])
There are also three special pattern diagnosis systems used in case
of febrile and infectious diseases only ("Six Channel system" or "six
division pattern" [六经辩证, pinyin: liù jīng biàn zhèng]; "Wei Qi Ying Xue system" or "four division pattern" [卫气营血辩证, pinyin: weì qì yíng xuè biàn zhèng]; "San Jiao system" or "three burners pattern" [三焦辩证, pinyin: sānjiaō biàn zhèng]).
Considerations of disease causes
Although TCM and its concept of disease do not strongly differentiate between cause and effect, pattern discrimination can include considerations regarding the disease cause; this is called 病因辩证 (pinyin: bìngyīn biàn zhèng, "disease-cause pattern discrimination").
There are three fundamental categories of disease causes (三因, pinyin: sān yīn) recognized:
- external causes: these include the Six Excesses and "Pestilential Qi".
- internal causes: the "Seven Affects" (七情, pinyin: qì qíng, sometimes also translated as "Seven Emotions") – joy, anger, brooding, sorrow, fear, fright and grief. These are believed to be able to cause damage to the functions of the zàng-fú, especially of the Liver.
- non-external-non-internal causes: dietary irregularities (especially: too much raw, cold, spicy, fatty or sweet food; voracious eating; too much alcohol), fatigue, sexual intemperance, trauma, and parasites (虫, pinyin: chóng).
Diagnostics
In TCM, there are five diagnostic methods: inspection, auscultation, olfaction, inquiry, and palpation.
- Inspection focuses on the face and particularly on the tongue, including analysis of the tongue size, shape, tension, color and coating, and the absence or presence of teeth marks around the edge.
- Auscultation refers to listening for particular sounds (such as wheezing).
- Olfaction refers to attending to body odor.
- Inquiry focuses on the "seven inquiries", which involve asking the person about the regularity, severity, or other characteristics of: chills, fever, perspiration, appetite, thirst, taste, defecation, urination, pain, sleep, menses, leukorrhea.
- Palpation which includes feeling the body for tender A-shi points, and the palpation of the wrist pulses as well as various other pulses, and palpation of the abdomen.
Tongue and pulse
Examination
of the tongue and the pulse are among the principal diagnostic methods
in TCM. Details of the tongue, including shape, size, color, texture,
cracks, teethmarks, as well as tongue coating are all considered as part
of tongue diagnosis. Various regions of the tongue's surface are
believed to correspond to the zàng-fŭ organs. For example, redness on
the tip of the tongue might indicate heat in the Heart, while redness on
another the sides of the tongue might indicate a heat in the Liver.
Pulse palpation involves measuring the pulse both at a superficial and at a deep level at three different locations on the radial artery (Cun, Guan, Chi,
located two fingerbreadths from the wrist crease, one fingerbreadth
from the wrist crease, and right at the wrist crease, respectively,
usually palpated with the index, middle and ring finger) of each arm,
for a total of twelve pulses, all of which are thought to correspond
with certain zàng-fŭ. The pulse is examined for several characteristics
including rhythm, strength and volume, and described with qualities
like "floating, slippery, bolstering-like, feeble, thready and quick";
each of these qualities indicate certain disease patterns. Learning TCM pulse diagnosis can take several years.
Herbal medicine
Assorted dried plant and animal parts used in traditional Chinese medicines, clockwise from top left corner: dried Lingzhi (lit. "spirit mushrooms"), ginseng, Luo Han Guo, turtle shell underbelly (plastron), and dried curled snakes.
Chinese red ginseng roots
A bile bear in a “crush cage” on Huizhou Farm, China.
Dried seahorses are extensively used in traditional medicine in China and elsewhere.
The term "herbal medicine" is somewhat misleading in that, while
plant elements are by far the most commonly used substances in TCM,
other, non-botanic substances are used as well: animal, human, and
mineral products are also utilized. Thus, the term "medicinal" (instead of herb) is usually preferred.
Prescriptions
Typically, one batch of medicinals is prepared as a decoction of about 9 to 18 substances.
Some of these are considered as main herbs, some as ancillary herbs;
within the ancillary herbs, up to three categories can be distinguished.
Raw materials
There are roughly 13,000 medicinals used in China and over 100,000 medicinal recipes recorded in the ancient literature. Plant elements and extracts are by far the most common elements used. In the classic Handbook of Traditional Drugs from 1941, 517 drugs were listed – out of these, 45 were animal parts, and 30 were minerals.
Animal substances
Some animal parts used as medicinals can be considered rather strange such as cows' gallstones, hornet's nests, leeches, and scorpion. Other examples of animal parts include horn of the antelope or buffalo, deer antlers, testicles and penis bone of the dog, and snake bile.
Some TCM textbooks still recommend preparations containing animal
tissues, but there has been little research to justify the claimed
clinical efficacy of many TCM animal products.
Some medicinals can include the parts of endangered species, including tiger bones and rhinoceros horn
which is used for many ailments (though not as an aphrodisiac as is commonly misunderstood in the West).
The black market in rhinoceros horn (driven not just by TCM but also
unrelated status-seeking) has reduced the world's rhino population by
more than 90 percent over the past 40 years. Concerns have also arisen over the use of pangolin scales, turtle plastron, seahorses, and the gill plates of mobula and manta rays. Poachers hunt restricted or endangered species to supply the black market with TCM products. There is no scientific evidence of efficacy for tiger medicines. Concern over China considering to legalize the trade in tiger parts prompted the 171-nation Convention on International Trade in Endangered Species (CITES) to endorse a decision opposing the resurgence of trade in tigers. Fewer than 30,000 saiga antelopes remain, which are exported to China for use in traditional fever therapies. Organized gangs illegally export the horn of the antelopes to China.
The pressures on seahorses (Hippocampus spp.) used in traditional
medicine is enormous; tens of millions of animals are unsustainably
caught annually. Many species of syngnathid are currently part of the IUCN Red List of Threatened Species or national equivalents.
Since TCM recognizes bear bile as a medicinal, more than 12,000 asiatic black bears are held in bear farms. The bile is extracted through a permanent hole in the abdomen leading to the gall bladder,
which can cause severe pain. This can lead to bears trying to kill
themselves. As of 2012, approximately 10,000 bears are farmed in China
for their bile. This practice has spurred public outcry across the country. The bile is collected from live bears via a surgical procedure. The deer penis
is believed to have therapeutic benefits according to traditional
Chinese medicine. Medicinal tiger parts from poached animals include tiger penis, believed to improve virility, and tiger eyes.
The illegal trade for tiger parts in China has driven the species to
near-extinction because of its popularity in traditional medicine. Laws protecting even critically endangered species such as the Sumatran tiger fail to stop the display and sale of these items in open markets. Shark fin soup
is traditionally regarded in Chinese medicine as beneficial for health
in East Asia, and its status as an elite dish has led to huge demand
with the increase of affluence in China, devastating shark populations. The shark fins have been a part of traditional Chinese medicine for centuries.
Shark finning is banned in many countries, but the trade is thriving in
Hong Kong and China, where the fins are part of shark fin soup, a dish
considered a delicacy, and used in some types of traditional Chinese
medicine.
The tortoise (Freshwater turtle - guiban) and the turtle (Chinese softshell turtle
- biejia) species used in traditional Chinese medicine are raised on
farms, while restrictions are made on the accumulation and export of
other endangered species. However, issues concerning the overexploitation of Asian turtles in China have not been completely solved. Australian scientists have developed methods to identify medicines containing DNA traces of endangered species.
Finally, although not an endangered species, sharp rises in exports of
donkeys and donkey hide from Africa to China to make the traditional
remedy ejiao have prompted export restrictions by some African
countries.
Human body parts
Dried human placenta (Ziheche (紫河车) is used in traditional Chinese medicine.
Traditional Chinese Medicine also includes some human parts: the classic Materia medica (Bencao Gangmu) describes the use of 35 human body parts and excreta
in medicines, including bones, fingernail, hairs, dandruff, earwax,
impurities on the teeth, feces, urine, sweat, organs, but most are no
longer in use.
Human placenta has been used an ingredient in certain traditional Chinese medicines, including using dried human placenta, known as "Ziheche", to treat infertility, impotence and other conditions. The consumption of the human placenta is a potential source of infection.
Traditional categorization
The traditional categorizations and classifications that can still be found today are:
- The classification according to the Four Natures (四气, pinyin: sì qì): hot, warm, cool, or cold (or, neutral in terms of temperature) and hot and warm herbs are used to treat cold diseases, while cool and cold herbs are used to treat heat diseases.
- The classification according to the Five Flavors, (五味, pinyin: wǔ wèi, sometimes also translated as Five Tastes): acrid, sweet, bitter, sour, and salty. Substances may also have more than one flavor, or none (i.e., a "bland" flavor). Each of the Five Flavors corresponds to one of zàng organs, which in turn corresponds to one of the Five Phases. A flavor implies certain properties and therapeutic actions of a substance; e.g., saltiness drains downward and softens hard masses, while sweetness is supplementing, harmonizing, and moistening.
- The classification according to the meridian – more precisely, the zàng-fu organ including its associated meridian – which can be expected to be primarily affected by a given medicinal.
- The categorization according to the specific function mainly include: exterior-releasing or exterior-resolving, heat-clearing, downward-draining, or precipitating wind-damp-dispelling, dampness-transforming, promoting the movement of water and percolating dampness or dampness-percolating, interior-warming, qi-regulating or qi-rectifying, dispersing food accumulation or food-dispersing, worm-expelling, stopping bleeding or blood-stanching, quickening the Blood and dispelling stasis or blood-quickening, transforming phlegm, stopping coughing and calming wheezing or phlegm-transforming and cough- and panting-suppressing, Spirit-quieting, calming the liver and expelling wind or liver-calming and wind-extinguishingl orifice-opening supplementing which includes qi-supplementing, blood-nourishing, yin-enriching, and yang-fortifying, astriction-promoting or securing and astringing, vomiting-inducing, and substances for external application.
Efficacy
As of 2007 there were not enough good-quality trials of herbal therapies to allow their effectiveness to be determined.
A high percentage of relevant studies on traditional Chinese medicine
are in Chinese databases. Fifty percent of systematic reviews on TCM did
not search Chinese databases, which could lead to a bias in the
results.
Many systematic reviews of TCM interventions published in Chinese
journals are incomplete, some contained errors or were misleading. The herbs recommended by traditional Chinese practitioners in the US are unregulated.
- A 2013 review found the data too weak to support use of Chinese herbal medicine (CHM) for benign prostatic hyperplasia.
- A 2013 review found the research on the benefit and safety of CHM for idiopathic sudden sensorineural hearing loss is of poor quality and cannot be relied upon to support their use.
- A 2013 Cochrane review found inconclusive evidence that CHM reduces the severity of eczema.
- The traditional medicine ginger, which has shown anti-inflammatory properties in laboratory experiments, has been used to treat rheumatism, headache and digestive and respiratory issues, though there is no firm evidence supporting these uses.
- A 2012 Cochrane review found no difference in mortality rate among 640 SARS patients when Chinese herbs were used alongside Western medicine versus Western medicine exclusively, although they concluded some herbs may have improved symptoms and decreased corticosteroid dosages.
- A 2012 Cochrane review found insufficient evidence to support the use of TCM for people with adhesive small bowel obstruction.
- A 2011 review found low quality evidence that suggests CHM improves the symptoms of Sjogren's syndrome.
- A 2010 review found TCM seems to be effective for the treatment of fibromyalgia but the findings were of insufficient methodological rigor.
- A 2009 Cochrane review found insufficient evidence to recommend the use of TCM for the treatment of epilepsy.
- A 2008 Cochrane review found promising evidence for the use of Chinese herbal medicine in relieving painful menstruation, but the trials assessed were of such low methodological quality that no conclusion could be drawn about the remedies' suitability as a recommendable treatment option.
- Turmeric has been used in traditional Chinese medicine for centuries to treat various conditions. This includes jaundice and hepatic disorders, rheumatism, anorexia, diabetic wounds, and menstrual complications. Most of its effects have been attributed to curcumin. Research that curcumin shows strong anti-inflammatory and antioxidant activities have instigated mechanism of action studies on the possibility for cancer and inflammatory diseases prevention and treatment. It also exhibits immunomodulatory effects.
- A 2005 Cochrane review found insufficient evidence for the use of CHM in HIV-infected people and people with AIDS. A 2010 Cochrane review found insufficient evidence to support the use of Traditional Chinese Herbal Products (THCP) in the treatment of angina. A 2010 Cochrane review found no evidence supporting the use of TCHM for stopping bleeding from haemorrhoids. There was some weak evidence of pain relief.
Drug research
Artemisia annua is traditionally used to treat fever. It has been found to have antimalarial properties.
With an eye to the enormous Chinese market, pharmaceutical companies
have explored the potential for creating new drugs from traditional
remedies. A Nature editorial described TCM as "fraught with pseudoscience", and stated that having "no rational mechanism of action
for most of its therapies" is the "most obvious answer" to why its
study didn't provide a "flood of cures", while advocates responded that
"researchers are missing aspects of the art, notably the interactions
between different ingredients in traditional therapies."
One of the successes was the development in the 1970s of the antimalarial drug artemisinin, which is a processed extract of Artemisia annua, a herb traditionally used as a fever treatment.
Artemisia annua has been used by Chinese herbalists in traditional
Chinese medicines for 2,000 years. In 1596, Li Shizhen recommended tea
made from qinghao specifically to treat malaria symptoms in his Compendium of Materia Medica. Researcher Tu Youyou discovered that a low-temperature extraction process could isolate an effective antimalarial substance from the plant. Tu says she was influenced by a traditional Chinese herbal medicine source, The Handbook of Prescriptions for Emergency Treatments, written in 340 by Ge Hong, which states that this herb should be steeped in cold water. The extracted substance, once subject to detoxification and purification processes, is a usable antimalarial drug – a 2012 review found that artemisinin-based remedies were the most effective drugs for the treatment of malaria. For her work on malaria, Tu received the 2015 Nobel Prize in Physiology or Medicine. Despite global efforts in combating malaria, it remains a large burden for the population. Although WHO recommends artemisinin-based remedies for treating uncomplicated malaria, artemisinin resistance can no longer be ignored.
Also in the 1970s Chinese researcher Zhang TingDong and colleagues investigated the potential use of the traditionally used substance arsenic trioxide to treat acute promyelocytic leukemia (APL). Building on his work, research both in China and the West eventually led to the development of the drug Trisenox, which was approved for leukemia treatment by the FDA in 2000.
Huperzine A, which is extracted from traditional herb Huperzia serrata, has attracted the interest of medical science because of alleged neuroprotective properties. Despite earlier promising results,
a 2013 systematic review and meta-analysis found "Huperzine A appears
to have beneficial effects on improvement of cognitive function, daily
living activity, and global clinical assessment in participants with
Alzheimer’s disease. However, the findings should be interpreted with
caution due to the poor methodological quality of the included trials."
Ephedrine in its natural form, known as má huáng (麻黄) in traditional Chinese medicine, has been documented in China since the Han dynasty (206 BC – 220 AD) as an antiasthmatic and stimulant. In 1885, the chemical synthesis of ephedrine was first accomplished by Japanese organic chemist Nagai Nagayoshi based on his research on Japanese and Chinese traditional herbal medicines.
Pien tze huang was first documented in the Ming dynasty.
Cost-effectiveness
A 2012 systematic review found there is a lack of available cost-effectiveness evidence in TCM.
Safety
Galena (lead ore) is part of historical TCM. Standard American TCM practice considers lead-containing herbs obsolete.
From the earliest records regarding the use of medicinals to today,
the toxicity of certain substances has been described in all Chinese
materiae medicae.
Since TCM has become more popular in the Western world, there are
increasing concerns about the potential toxicity of many traditional
Chinese medicinals including plants, animal parts and minerals.
Traditional Chinese herbal remedies are conveniently available from
grocery stores in most Chinese neighborhoods; some of these items may
contain toxic ingredients, are imported into the U.S. illegally, and are
associated with claims of therapeutic benefit without evidence. For most medicinals, efficacy and toxicity testing are based on traditional knowledge rather than laboratory analysis. The toxicity in some cases could be confirmed by modern research (i.e., in scorpion); in some cases it couldn't (i.e., in Curculigo).
Traditional herbal medicines can contain extremely toxic chemicals and
heavy metals, and naturally occurring toxins, which can cause illness,
exacerbate pre-existing poor health or result in death. Botanical misidentification of plants can cause toxic reactions in humans.
The description on some plants used in traditional Chinese medicine
have changed, leading to unintended intoxication of the wrong plants. A concern is also contaminated herbal medicines with microorganisms and fungal toxins, including aflatoxin.
Traditional herbal medicines are sometimes contaminated with toxic
heavy metals, including lead, arsenic, mercury and cadmium, which
inflict serious health risks to consumers.
Also, adulteration of some herbal medicine preparations with
conventional drugs which may cause serious adverse effects, such as corticosteroids, phenylbutazone, phenytoin, and glibenclamide, has been reported.
Substances known to be potentially dangerous include Aconitum, secretions from the Asiatic toad, powdered centipede, the Chinese beetle (Mylabris phalerata), certain fungi, Aristolochia, Arsenic sulfide (Realgar), mercury sulfide, and cinnabar. Asbestos ore (Actinolite, Yang Qi Shi, 阳起石) is used to treat impotence in TCM. Due to galena's (litharge, lead(II) oxide) high lead content, it is known to be toxic. Lead, mercury, arsenic, copper, cadmium, and thallium have been detected in TCM products sold in the U.S. and China.
To avoid its toxic adverse effects Xanthium sibiricum must be processed. Hepatotoxicity has been reported with products containing Polygonum multiflorum, glycyrrhizin, Senecio and Symphytum. The herbs indicated as being hepatotoxic included Dictamnus dasycarpus, Astragalus membranaceous, and Paeonia lactiflora. Contrary to popular belief, Ganoderma lucidum mushroom extract, as an adjuvant for cancer immunotherapy, appears to have the potential for toxicity. A 2013 review suggested that although the antimalarial herb Artemisia annua
may not cause hepatotoxicity, haematotoxicity, or hyperlipidemia, it
should be used cautiously during pregnancy due to a potential risk of
embryotoxicity at a high dose.
However, many adverse reactions are due to misuse or abuse of Chinese medicine. For example, the misuse of the dietary supplement Ephedra (containing ephedrine) can lead to adverse events including gastrointestinal problems as well as sudden death from cardiomyopathy. Products adulterated with pharmaceuticals for weight loss or erectile dysfunction are one of the main concerns. Chinese herbal medicine has been a major cause of acute liver failure in China.
Acupuncture and moxibustion
Needles being inserted into the skin.
Traditional moxibustion set from Ibuki (Japan)
Acupuncture is the insertion of needles into superficial structures
of the body (skin, subcutaneous tissue, muscles) – usually at
acupuncture points (acupoints) – and their subsequent manipulation; this
aims at influencing the flow of qi. According to TCM it relieves pain and treats (and prevents) various diseases. The US FDA classifies single-use acupuncture needles as Class II medical devices, under CFR 21.
Acupuncture is often accompanied by moxibustion – the Chinese characters for acupuncture (simplified Chinese: 针灸; traditional Chinese: 針灸; pinyin: zhēnjiǔ) literally meaning "acupuncture-moxibustion" – which involves burning mugwort on or near the skin at an acupuncture point. According to the American Cancer Society,
"available scientific evidence does not support claims that moxibustion
is effective in preventing or treating cancer or any other disease".
In electroacupuncture,
an electric current is applied to the needles once they are inserted,
in order to further stimulate the respective acupuncture points.
Efficacy
A 2013 editorial by Steven P. Novella and David Colquhoun
found that the inconsistency of results of acupuncture studies (i.e.
acupuncture relieved pain in some conditions but had no effect in other
very similar conditions) suggests false positive results,
which may be caused by factors like biased study designs, poor
blinding, and the classification of electrified needles (a type of TENS) as a form of acupuncture.
The same editorial suggested that given the inability to find
consistent results despite more than 3,000 studies of acupuncture, the
treatment seems to be a placebo effect and the existing equivocal positive results are noise one expects to see after a large number of studies are performed on an inert therapy.
The editorial concluded that the best controlled studies showed a clear
pattern, in which the outcome does not rely upon needle location or
even needle insertion, and since "these variables are those that define
acupuncture, the only sensible conclusion is that acupuncture does not
work."
According to the US NIH National Cancer Institute, a review of 17,922
patients reported that real acupuncture relieved muscle and joint pain,
caused by aromatase inhibitors, much better than sham acupuncture.
Regarding cancer patients, The US NIH National Cancer Institute states
that acupuncture may cause physical responses in nerve cells, the
pituitary gland, and the brain - releasing proteins, hormones, and
chemicals that are proposed to affect blood pressure, body temperature,
immune activity, and endorphin release.
A 2012 meta-analysis concluded that the mechanisms of acupuncture
"are clinically relevant, but that an important part of these total
effects is not due to issues considered to be crucial by most
acupuncturists, such as the correct location of points and depth of
needling ... [but are] ... associated with more potent placebo or
context effects". Commenting on this meta-analysis, both Edzard Ernst and David Colquhoun said the results were of negligible clinical significance.
A 2011 overview of Cochrane reviews found high quality evidence that suggests acupuncture is effective for some but not all kinds of pain.
A 2010 systematic review found that there is evidence "that acupuncture
provides a short-term clinically relevant effect when compared with a
waiting list control or when acupuncture is added to another
intervention" in the treatment of chronic low back pain.
Two review articles discussing the effectiveness of acupuncture, from
2008 and 2009, have concluded that there is not enough evidence to
conclude that it is effective beyond the placebo effect.
Acupuncture is generally safe when administered using Clean Needle Technique (CNT). Although serious adverse effects are rare, acupuncture is not without risk. Severe adverse effects, including death, have continued to be reported.
Tui na
An example of a Traditional Chinese medicine used in Tui Na
Tui na (推拿) is a form of massage akin to acupressure (from which shiatsu evolved). Asian massage is typically administered with the person fully clothed, without the application of grease or oils.[182] Techniques employed may include thumb presses, rubbing, percussion, and assisted stretching.
Qigong
Qìgōng (气功 or 氣功) is a TCM system of exercise and meditation that
combines regulated breathing, slow movement, and focused awareness,
purportedly to cultivate and balance qi.
One branch of qigong is qigong massage, in which the practitioner
combines massage techniques with awareness of the acupuncture channels
and points.
Other therapies
Cupping
Acupuncture and moxibustion after cupping in Japan
Cupping (Chinese: 拔罐; pinyin: báguàn) is a type of Chinese massage,
consisting of placing several glass "cups" (open spheres) on the body. A
match is lit and placed inside the cup and then removed before placing
the cup against the skin. As the air in the cup is heated, it expands,
and after placing in the skin, cools, creating lower pressure inside the
cup that allows the cup to stick to the skin via suction. When combined with massage oil, the cups can be slid around the back, offering "reverse-pressure massage".
It has not been found to be effective for the treatment of any disease. The 2008 Trick or Treatment book said that no evidence exists of any beneficial effects of cupping for any medical condition.
Gua Sha
Gua Sha
Gua Sha
(Chinese: 刮痧; pinyin: guāshā) is abrading the skin with pieces of
smooth jade, bone, animal tusks or horns or smooth stones; until red
spots then bruising cover the area to which it is done. It is believed
that this treatment is for almost any ailment including cholera. The red spots and bruising take 3 to 10 days to heal, there is often some soreness in the area that has been treated.
Die-da
Diē-dá (跌打) or bone-setting is usually practiced by martial artists who know aspects of Chinese medicine that apply to the treatment of trauma
and injuries such as bone fractures, sprains, and bruises. Some of
these specialists may also use or recommend other disciplines of Chinese
medical therapies (or Western medicine in modern times) if serious
injury is involved. Such practice of bone-setting (整骨 or 正骨) is not
common in the West.
Chinese food therapy
Traditional Chinese characters 陰 and 陽 for the words yin and yang denote different classes of foods, and it is important to consume them in a balanced fashion. The meal sequence should also observe these classes:
- In the Orient, it is traditional to eat yang before yin. Miso soup (yang — fermented soybean protein) for breakfast; raw fish (more yang protein); and then the vegetables which are yin.
Regulations
Many governments have enacted laws to regulate TCM practice.
Australia
From
1 July 2012 Chinese medicine practitioners must be registered under the
national registration and accreditation scheme with the Chinese
Medicine Board of Australia and meet the Board's Registration Standards,
in order to practice in Australia.
Canada
TCM is regulated in five provinces in Canada: Alberta, British Columbia, Ontario, Quebec, and Newfoundland.
China
China’s
National People’s Congress Standing Committee passed the country’s first
law on TCM in 2016, scheduled to take effect July 1, 2017. The new law
standardized TCM certifications by requiring TCM practitioners to (i)
pass exams administered by provincial-level TCM authorities, and (ii)
obtain recommendations from two certified practitioners. TCM products
and services can be advertised only with approval from the local TCM
authority.
Hong Kong
The
Chinese Medicine Council of Hong Kong was established in 1999. It
regulates the medicinals and professional standards for TCM
practitioners. All TCM practitioners in Hong Kong are required to
register with the Council. The eligibility for registration includes a
recognised 5-year university degree of TCM, a 30-week minimum supervised
clinical internship, and passing the licensing exam.
Malaysia
The
Traditional and Complementary Medicine Bill was passed by Parliament in
2012 establishing the Traditional and Complementary Medicine Council to
register and regulate traditional and complementary medicine
practitioners, including traditional Chinese medicine practitioners as
well as other traditional and complementary medicine practitioners such
as those in traditional Malay medicine and traditional Indian medicine.
Singapore
The
TCM Practitioners Act was passed by Parliament in 2000 and the TCM
Practitioners Board was established in 2001 as a statutory board under
the Ministry of Health, to register and regulate TCM practitioners. The
requirements for registration include possession of a diploma or degree
from a TCM educational institution/university on a gazetted list, either
structured TCM clinical training at an approved local TCM educational
institution or foreign TCM registration together with supervised TCM
clinical attachment/practice at an approved local TCM clinic, and upon
meeting these requirements, passing the Singapore TCM Physicians
Registration Examination (STRE) conducted by the TCM Practitioners
Board.
United States
As
of July 2012, only six states do not have existing legislation to
regulate the professional practice of TCM. These six states are Alabama, Kansas, North Dakota, South Dakota, Oklahoma, and Wyoming. In 1976, California established an Acupuncture Board and became the first state licensing professional acupuncturists.
Indonesia
The Chinese traditional medicine at one of Chinese traditional medicine shop at Jagalan Road, Surabaya, Indonesia.
All traditional medicines, including TCM, are regulated on Indonesian
Minister of Health Regulation in 2013 about Traditional Medicine.
Traditional Medicine License (Surat Izin Pengobatan Tradisional
-SIPT) will be granted to the practitioners whose methods are
scientifically recognized as safe and bring the benefit for health.
The TCM clinics are registered but there is no explicit regulation for
it. The only TCM method which is accepted by medical logic and is
empirically proofed is acupuncture. The acupuncturists can get SIPT and participate on health care facilities.