From Wikipedia, the free encyclopedia
Caesarean section, also known as
C-section, or
caesarean delivery, is the use of
surgery to
deliver babies. A caesarean section is often necessary when a
vaginal delivery would put the baby or mother at risk. This may include
obstructed labor,
twin pregnancy,
high blood pressure in the mother,
breech birth, or problems with the
placenta or
umbilical cord. A caesarean delivery may be performed based upon the shape of the mother's
pelvis or history of a previous C-section. A trial of
vaginal birth after C-section may be possible. The
World Health Organization recommends that caesarean section be performed only when medically necessary. Some C-sections are performed
without a medical reason, upon request by someone, usually the mother.
A C-section typically takes 45 minutes to an hour. It may be done with a
spinal block, where the woman is awake or under
general anesthesia. A
urinary catheter is used to drain the
bladder, and the skin of the
abdomen is then cleaned with an
antiseptic. An
incision of about 15 cm (6 inches) is then typically made through the mother's lower abdomen. The
uterus is then opened with a second incision and the baby delivered. The incisions are then
stitched closed. A woman can typically begin
breastfeeding as soon as she is out of the
operating room and awake. Often, several days are required in the hospital to recover sufficiently to return home.
C-sections result in a small overall increase in poor outcomes in low-risk pregnancies. They also typically take longer to heal from, about six weeks, than vaginal birth. The increased risks include breathing problems in the baby and
amniotic fluid embolism and
postpartum bleeding in the mother. Established guidelines recommend that caesarean sections not be used before 39
weeks of pregnancy without a medical reason. The method of delivery does not appear to have an effect on subsequent
sexual function.
In 2012, about 23 million C-sections were done globally. The international healthcare community has previously considered the rate of 10% and 15% to be ideal for caesarean sections. Some evidence finds a higher rate of 19% may result in better outcomes. More than 45 countries globally have C-section rates less than 7.5%, while more than 50 have rates greater than 27%. Efforts are being made to both improve access to and reduce the use of C-section. In the United States as of 2017, about 32% of deliveries are by C-section.
The surgery has been performed at least as far back as 715 BC following
the death of the mother, with the baby occasionally surviving. Descriptions of mothers surviving date back to 1500. With the introduction of
antiseptics and
anesthetics in the 19th century, survival of both the mother and baby became common.
Uses

A 7-week old caesarean section scar and linea nigra visible on a 31-year-old mother: Longitudinal incisions are still sometimes used.
Caesarean section is recommended when
vaginal delivery might pose a risk to the mother or baby. C-sections are also carried out for personal and social reasons on
maternal request in some countries.
Medical uses
Complications of labor and factors increasing the risk associated with vaginal delivery include:
Other complications of pregnancy, pre-existing conditions, and concomitant disease, include:
Other
- Decreasing experience of accoucheurs with the management of
breech presentation. Although obstetricians and midwives are extensively
trained in proper procedures for breech presentation deliveries using
simulation mannequins, there is decreasing experience with actual
vaginal breech delivery, which may increase the risk.
Prevention
The
prevalence of caesarean section is generally agreed to be higher than
needed in many countries, and physicians are encouraged to actively
lower the rate, as a caesarean rate higher than 10-15% is not associated
with reductions in maternal or infant mortality rates. Some evidence supports a higher rate of 19% may result in better outcomes.
Some of these efforts are: emphasizing a long
latent phase
of labor is not abnormal and not a justification for C-section; a new
definition of the start of active labor from a cervical dilatation of
4 cm to a dilatation of 6 cm; and allowing women who have previously
given birth to push for at least 2 hours, with 3 hours of pushing for
women who have not previously given birth, before
labor arrest is considered.
Physical exercise during pregnancy decreases the risk.
Risks
Adverse outcomes in low-risk pregnancies occur in 8.6% of vaginal deliveries and 9.2% of caesarean section deliveries.
Mother
In those who are low risk, the
risk of death for caesarean sections is 13 per 100,000 vs. for vaginal birth 3.5 per 100,000 in the developed world—a numerically very small risk of death in either situation in resource-rich settings. The United Kingdom
National Health Service gives the risk of death for the mother as three times that of a vaginal birth.
In Canada, the difference in serious morbidity or mortality for
the mother (e.g. cardiac arrest, wound hematoma, or hysterectomy) was
1.8 additional cases per 100. The difference in in-hospital maternal death was not significant.
A caesarean section is associated with risks of postoperative
adhesions, incisional hernias (which may require surgical correction), and wound infections.
If a caesarean is performed in an emergency, the risk of the surgery
may be increased due to a number of factors. The patient's stomach may
not be empty, increasing the risk of anaesthesia. Other risks include severe blood loss (which may require a blood transfusion) and
postdural-puncture spinal headaches.
Wound infections occur after caesarean sections at a rate of 3-15%.
Women who had caesarean sections are more likely to have problems
with later pregnancies, and women who want larger families should not
seek an elective caesarean unless medical indications to do so exist.
The risk of
placenta accreta,
a potentially life-threatening condition which is more likely to
develop where a woman has had a previous caesarean section, is 0.13%
after two caesarean sections, but increases to 2.13% after four and then
to 6.74% after six or more. Along with this is a similar rise in the
risk of emergency hysterectomies at delivery.
Mothers can experience an increased incidence of
postnatal depression, and can experience significant psychological trauma and ongoing
birth-related post-traumatic stress disorder after obstetric intervention during the birthing process.
Factors like pain in the first stage of labor, feelings of
powerlessness, intrusive emergency obstetric intervention are important
in the subsequent development of psychological issues related to labor
and delivery.
Subsequent pregnancies
Women who have had a caesarean for any reason are somewhat less
likely to become pregnant again as compared to women who have previously
delivered only vaginally, but the effect is small.
- Vaginal birth after caesarean section (VBAC)
- Elective repeat caesarean section (ERCS)
Both have higher risks than a vaginal birth with no previous
caesarean section. There are many issues which must be taken into
account when planning the mode of delivery for every pregnancy, not just
those complicated by a previous caesarean section and there is a list
of some of these issues in the list of indications for section in the
first part of this article. A vaginal birth after caesarean section
(VBAC) confers a higher risk of
uterine rupture (5 per 1,000), blood transfusion or
endometritis (10 per 1,000), and
perinatal death of the child (0.25 per 1,000).
Furthermore, 20% to 40% of planned VBAC attempts end in caesarean
section being needed, with greater risks of complications in an
emergency repeat caesarean section than in an elective repeat caesarean
section. On the other hand, VBAC confers less
maternal morbidity and a decreased risk of complications in future pregnancies than elective repeat caesarean section.
Adhesions
Suturing of the uterus after extraction
Closed incision for low transverse abdominal incision after stapling has been completed
There are several steps that can be taken during abdominal or pelvic
surgery to minimize postoperative complications, such as the formation
of
adhesions. Such techniques and principles may include:
- • Handling all tissue with absolute care
- • Using powder-free surgical gloves
- • Controlling bleeding
- • Choosing sutures and implants carefully
- • Keeping tissue moist
- • Preventing infection with antibiotics given intravenously to the mother before skin incision
Despite these proactive measures, adhesion formation is a recognized
complication of any abdominal or pelvic surgery. To prevent adhesions
from forming after caesarean section,
adhesion barrier
can be placed during surgery to minimize the risk of adhesions between
the uterus and ovaries, the small bowel, and almost any tissue in the
abdomen or pelvis. This is not current UK practice, as there is no
compelling evidence to support the benefit of this intervention.
Adhesions can cause long-term problems, such as:
- • Infertility,
which may end when adhesions distort the tissues of the ovaries and
tubes, impeding the normal passage of the egg (ovum) from the ovary to
the uterus. One in five infertility cases may be adhesion related
(stoval)
- • Chronic pelvic pain, which may result when adhesions are present
in the pelvis. Almost 50% of chronic pelvic pain cases are estimated to
be adhesion related (stoval)
- • Small bowel obstruction: the disruption of normal bowel flow, which can result when adhesions twist or pull the small bowel.
The risk of adhesion formation is one reason why vaginal delivery is
usually considered safer than elective caesarean section where there is
no medical indication for section for either maternal or fetal reasons.
Child
Non-medically
indicated (elective) childbirth before 39 weeks gestation "carry
significant risks for the baby with no known benefit to the mother."
Complications from elective caesarean before 39 weeks include: newborn
mortality at 37 weeks may be up to 3 times the number at 40 weeks, and
was elevated compared to 38 weeks gestation. These “early term” births
were associated with more death during infancy, compared to those
occurring at 39 to 41 weeks ("full term").
Researchers in one study and another review found many benefits to
going full term, but “no adverse effects” in the health of the mothers
or babies.
The
American Congress of Obstetricians and Gynecologists and medical policy makers review research studies and find more incidence of suspected or proven
sepsis,
RDS, hypoglycemia, need for respiratory support, need for NICU
admission, and need for hospitalization > 4–5 days. In the case of
caesarean sections, rates of respiratory death were 14 times higher in
pre-labor at 37 compared with 40 weeks gestation, and 8.2 times higher
for pre-labor caesarean at 38 weeks. In this review, no studies found
decreased neonatal morbidity due to non-medically indicated (elective)
delivery before 39 weeks.
For otherwise healthy
twin pregnancies where both twins are head down a trial of
vaginal delivery is recommended at between 37 and 38 weeks. Vaginal delivery, in this case, does not worsen the outcome for either infant as compared with caesarean section.
There is some controversy on the best method of delivery where the
first twin is head first and the second is not, but most obstetricians
will recommend normal delivery unless there are other reasons to avoid
vaginal birth. When the first twin is not head down, a caesarean section is often recommended.
Regardless of whether the twins are delivered by section or vaginally,
the medical literature recommends delivery of dichorionic twins at 38
weeks, and monochorionic twins (identical twins sharing a placenta) by
37 weeks due to the increased risk of stillbirth in monochorionic twins
who remain in utero after 37 weeks.
The consensus is that late preterm delivery of monochorionic twins is
justified because the risk of stillbirth for post-37 week delivery is
significantly higher than the risks posed by delivering monochorionic
twins near term (i.e., 36–37 weeks).
The consensus concerning monoamniotic twins (identical twins sharing an
amniotic sac), the highest risk type of twins, is that they should be
delivered by caesarean section at or shortly after 32 weeks, since the
risks of intrauterine death of one or both twins is higher after this
gestation than the risk of complications of prematurity.
In a research study widely publicized, singleton children born
earlier than 39 weeks may have developmental problems, including slower
learning in reading and math.
Other risks include:
- Wet lung: Retention of fluid in the lungs can occur if not expelled by the pressure of contractions during labor.
- Potential for early delivery and complications: Preterm delivery may
be inadvertently carried out if the due-date calculation is inaccurate.
One study found an increased complication risk if a repeat elective
caesarean section is performed even a few days before the recommended 39
weeks.
- Higher infant mortality risk: In caesarean sections performed with
no indicated medical risk (singleton at full term in a head-down
position with no other obstetric or medical complications), the risk of
death in the first 28 days of life has been cited as 1.77 per 1,000 live
births among women who had caesarean sections, compared to 0.62 per
1,000 for women who delivered vaginally.
Birth by caesarean section also seems to be associated with worse
health outcomes later in life, including overweight or obesity and
problems in the immune system.
Classification
Caesarean sections have been classified in various ways by different perspectives.
One way to discuss all classification systems is to group them by their
focus either on the urgency of the procedure, characteristics of the
mother, or as a group based on other, less commonly discussed factors.
It is most common to classify caesarean sections by the urgency of performing them.
By urgency
Conventionally, caesarean sections are classified as being either an
elective surgery or an
emergency operation.
Classification is used to help communication between the obstetric,
midwifery and anaesthetic team for discussion of the most appropriate
method of anaesthesia. The decision whether to perform
general anesthesia or
regional anesthesia
(spinal or epidural anaesthetic) is important and is based on many
indications, including how urgent the delivery needs to be as well as
the medical and obstetric history of the woman.
Regional anaesthetic is almost always safer for the woman and the baby
but sometimes general anaesthetic is safer for one or both, and the
classification of urgency of the delivery is an important issue
affecting this decision.
A planned caesarean (or elective/scheduled caesarean), arranged
ahead of time, is most commonly arranged for medical indications which
have developed before or during the pregnancy, and ideally after 39
weeks of gestation. In the UK, this is classified as a 'grade 4' section
(delivery timed to suit the mother or hospital staff) or as a 'grade 3'
section (no maternal or fetal compromise but early delivery needed).
Emergency caesarean sections are performed in pregnancies in which a
vaginal delivery was planned initially, but an indication for caesarean
delivery has since developed. In the UK they are further classified as
grade 2 (delivery required within 90 minutes of the decision but no
immediate threat to the life of the woman or the fetus) or grade 1
(delivery required within 30 minutes of the decision: immediate threat
to the life of the mother or the baby or both.)
Elective caesarean sections may be performed on the basis of an
obstetrical or medical indication, or because of a medically
non-indicated
maternal request. Among women in the United Kingdom, Sweden and Australia, about 7% preferred caesarean section as a method of delivery. In cases without medical indications the
American Congress of Obstetricians and Gynecologists and the UK Royal College of Obstetricians and Gynaecologists recommend a planned vaginal delivery. The
National Institute for Health and Care Excellence
recommends that if after a woman has been provided information on the
risk of a planned caesarean section and she still insists on the
procedure it should be provided. If provided this should be done at 39 weeks of gestation or later. There is no evidence that ECS can reduce mother-to-child
hepatitis B and
hepatitis C virus transmission.
By characteristics of the mother
Caesarean delivery on maternal request
Caesarean delivery on maternal request (CDMR) is a medically unnecessary caesarean section, where the conduct of a
childbirth via a caesarean section is requested by the
pregnant patient even though there is not a medical
indication to have the surgery. Systematic reviews have found no strong evidence about the impact of caesareans for nonmedical reasons.
Recommendations encourage counseling to identify the reasons for the
request, addressing anxieties and information, and encouraging vaginal
birth. Elective caesareans at 38 weeks in some studies showed increased health complications in the newborn. For this reason
ACOG and
NICE recommend that elective caesarean sections should not be scheduled before 39 weeks gestation unless there is a medical reason.
Planned caesarean sections may be scheduled earlier if there is a medical reason.
After previous caesarean
Mothers who have previously had a caesarean section are more likely
to have a caesarean section for future pregnancies than mothers who have
never had a caesarean section. There is discussion about the
circumstances under which women should have a vaginal birth after a
previous caesarean.
Vaginal birth after caesarean (VBAC) is the practice of
birthing a baby vaginally after a previous baby has been delivered by caesarean section (surgically). According to
The American College of Obstetricians and Gynecologists
(ACOG), successful VBAC is associated with decreased maternal morbidity
and a decreased risk of complications in future pregnancies. According to the American Pregnancy Association, 90% of women who have undergone caesarean deliveries are candidates for VBAC.
Approximately 60-80% of women opting for VBAC will successfully give
birth vaginally, which is comparable to the overall vaginal delivery
rate in the United States in 2010.
Twins
For
otherwise healthy twin pregnancies where both twins are head down a
trial of vaginal delivery is recommended at between 37 and 38 weeks. Vaginal delivery in this case does not worsen the outcome for either infant as compared with caesarean section. There is controversy on the best method of delivery where the first twin is head first and the second is not. When the first twin is not head down at the point of labor starting, a caesarean section should be recommended.
Although the second twin typically has a higher frequency of problems,
it is not known if a planned caesarean section affects this. It is estimated that 75% of twin pregnancies in the United States were delivered by caesarean section in 2008.
Breech birth
A breech birth is the birth of a baby from a breech
presentation, in which the baby exits the pelvis with the
buttocks or
feet first as opposed to the normal
head-first presentation. In breech presentation, fetal heart sounds are heard just above the umbilicus.
Babies are usually born head first. If the baby is in another
position the birth may be complicated. In a ‘breech presentation’, the
unborn baby is bottom-down instead of head-down. Babies born
bottom-first are more likely to be harmed during a normal (vaginal)
birth than those born head-first. For instance, the baby might not get
enough oxygen during the birth. Having a planned caesarean may reduce
these problems. A review looking at planned caesarean section for
singleton breech presentation with planned vaginal birth, concludes that
in the short term, births with a planned caesarean were safer for
babies than vaginal births. Fewer babies died or were seriously hurt
when they were born by caesarean. There was tentative evidence that
children who were born by caesarean had more health problems at age two.
Caesareans caused some short-term problems for mothers such as more
abdominal pain. They also had some benefits, such as less urinary
incontinence and less perineal pain.
The bottom-down position presents some hazards to the baby during
the process of birth, and the mode of delivery (vaginal versus
caesarean) is controversial in the fields of
obstetrics and
midwifery.
Though vaginal
birth
is possible for the breech baby, certain fetal and maternal factors
influence the safety of vaginal breech birth. The majority of breech
babies born in the United States and the UK are delivered by caesarean
section as studies have shown increased risks of morbidity and mortality
for vaginal breech delivery, and most obstetricians counsel against
planned vaginal breech birth for this reason. As a result of reduced
numbers of actual vaginal breech deliveries, obstetricians and midwives
are at risk of de-skilling in this important skill. All those involved
in delivery of obstetric and midwifery care in the UK undergo mandatory
training in conducting breech deliveries in the simulation environment
(using dummy pelvises and mannequins to allow practice of this important
skill) and this training is carried out regularly to keep skills up to
date.
Resuscitative hysterotomy
A resuscitative
hysterotomy, also known as a peri-mortem caesarean delivery, is an emergency caesarean delivery carried out where maternal
cardiac arrest has occurred, to assist in
resuscitation of the mother by removing the
aortocaval compression
generated by the gravid uterus. Unlike other forms of caesarean
section, the welfare of the fetus is a secondary priority only, and the
procedure may be performed even prior to the limit of
fetal viability if it is judged to be of benefit to the mother.
Other ways, including the surgery technique
There
are several types of caesarean section (CS). An important distinction
lies in the type of incision (longitudinal or transverse) made on the
uterus, apart from the incision on the skin: the vast majority of skin incisions are a transverse suprapubic approach known as a
Pfannenstiel incision but there is no way of knowing from the skin scar which way the uterine incision was conducted.
- The classical caesarean section involves a longitudinal
midline incision on the uterus which allows a larger space to deliver
the baby. It is performed at very early gestations where the lower
segment of the uterus is unformed as it is safer in this situation for
the baby: but it is rarely performed other than at these early
gestations, as the operation is more prone to complications than a low
transverse uterine incision. Any woman who has had a classical section
will be recommended to have an elective repeat section in subsequent
pregnancies as the vertical incision is much more likely to rupture in
labor than the transverse incision.
- The lower uterine segment section is the procedure most commonly used today; it involves a transverse cut just above the edge of the bladder. It results in less blood loss
and has fewer early and late complications for the mother, as well as
allowing her to consider a vaginal birth in the next pregnancy.
- A caesarean hysterectomy consists of a caesarean section followed by the removal of the uterus. This may be done in cases of intractable bleeding or when the placenta cannot be separated from the uterus.
The
EXIT procedure is a specialized surgical delivery procedure used to deliver babies who have airway compression.
The Misgav Ladach method is a modified caesarean section which
has been used nearly all over the world since the 1990s. It was
described by Michael Stark, the president of the New European Surgical
Academy, at the time he was the director of
Misgav Ladach, a general hospital in Jerusalem. The method was presented during a FIGO conference in Montréal in 1994
and then distributed by the University of Uppsala, Sweden, in more than
100 countries. This method is based on minimalistic principles. He
examined all steps in caesarean sections in use, analyzed them for their
necessity and, if found necessary, for their optimal way of
performance. For the abdominal incision he used the modified Joel Cohen
incision and compared the longitudinal abdominal structures to strings
on musical instruments. As blood vessels and muscles have lateral sway,
it is possible to stretch rather than cut them. The peritoneum is opened
by repeat stretching, no abdominal swabs are used, the uterus is closed
in one layer with a big needle to reduce the amount of foreign body as
much as possible, the peritoneal layers remain unsutured and the abdomen
is closed with two layers only. Women undergoing this operation recover
quickly and can look after the newborns soon after surgery. There are
many publications showing the advantages over traditional caesarean
section methods. There is also an increased risk of abruptio placentae
and uterine rupture in subsequent pregnancies for women who underwent
this method in prior deliveries.
Technique
Several caesarean sections:
Is: supra-umbilical incision
Im: median incision
IM: Maylard incision
IP: Pfannenstiel incision
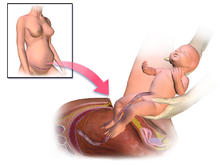
Illustration depicting caesarean section
Antibiotic prophylaxis is used before an incision. The
uterus is incised, and this incision is extended with blunt pressure along a cephalad-caudad axis. The infant is delivered, and the
placenta is then removed. The surgeon then makes a decision about uterine exteriorization. Single-layer uterine closure is used when the mother does not want a future pregnancy. When subcutaneous tissue is 2 cm thick or more,
surgical suture is used. Discouraged practices include manual
cervical dilation, any subcutaneous
drain, or supplemental
oxygen therapy with intent to prevent infection.
Caesarean section can be performed with
single or
double layer suturing of the uterine incision.
Single layer closure compared with double layer closure has been
observed to result in reduced blood loss during the surgery. It is
uncertain whether this is the direct effect of the suturing technique or
if other factors such as the type and site of abdominal incision
contribute to reduced blood loss. Standard procedure includes the closure of the
peritoneum.
Research questions whether this is needed, with some studies indicating
peritoneal closure is associated with longer operative time and
hospital stay.
The Misgave Ladach method is a surgery technical that may have fewer
secondary complications and faster healing, due to the insertion into
the muscle.
Anesthesia
Both
general and
regional anaesthesia (
spinal,
epidural or
combined spinal and epidural anaesthesia)
are acceptable for use during caesarean section. Evidence does not show
a difference between regional anaesthesia and general anaesthesia with
respect to major outcomes in the mother or baby. Regional anaesthesia may be preferred as it allows the mother to be awake and interact immediately with her baby. Compared to general anaesthesia, regional anaesthesia is better at preventing
persistent postoperative pain 3 to 8 months after caesarean section. Other advantages of regional anesthesia may include the absence of typical risks of general anesthesia:
pulmonary aspiration (which has a relatively high incidence in patients undergoing anesthesia in late pregnancy) of gastric contents and
esophageal intubation. One trial found no difference in satisfaction when general anaesthesia was compared with either spinal anaesthesia.
Regional anaesthesia is used in 95% of deliveries, with spinal
and combined spinal and epidural anaesthesia being the most commonly
used regional techniques in scheduled caesarean section. Regional anaesthesia during caesarean section is different from the
analgesia
(pain relief) used in labor and vaginal delivery. The pain that is
experienced because of surgery is greater than that of labor and
therefore requires a more intense
nerve block.
General anesthesia may be necessary because of specific risks to
mother or child. Patients with heavy, uncontrolled bleeding may not
tolerate the hemodynamic effects of regional anesthesia. General
anesthesia is also preferred in very urgent cases, such as severe fetal
distress, when there is no time to perform a regional anesthesia.
Prevention of complications
Postpartum infection is one of the main causes of maternal death and may account for 10% of maternal deaths globally.
A caesarean section greatly increases the risk of infection and
associated morbidity, estimated to be between 5 and 20 times as high,
and routine use of antibiotic prophylaxis to prevent infections was
found by a
meta-analysis to substantially reduce the incidence of febrile morbidity. Infection can occur in around 8% of women who have caesareans, largely
endometritis,
urinary tract infections
and wound infections. The use of preventative antibiotics in women
undergoing caesarean section decreased wound infection, endometritis,
and serious infectious complications by about 65%. Side effects and effect on the baby is unclear.
Women who have caesareans can recognize the signs of fever that indicate the possibility of wound infection. Taking antibiotics before skin incision rather than after
cord clamping reduces the risk for the mother, without increasing adverse effects for the baby. Whether a particular type of skin cleaner improves outcomes is unclear.
Some doctors believe that during a caesarean section, mechanical
cervical dilation with a finger or forceps will prevent the obstruction of blood and
lochia drainage, and thereby benefit the mother by reducing the risk of death. The evidence as of 2018 neither supported nor refuted this practice for reducing postoperative morbidity, pending further large studies.
Recovery
It is
common for women who undergo caesarean section to have reduced or
absent bowel movements for hours to days. During this time, women may
experience abdominal cramps, nausea and vomiting. This usually resolves
without treatment. Poorly controlled pain following non-emergent caesarean section occurs in between 13% to 78% of women. Abdominal, wound and back pain can continue for months after a caesarean section.
Non-steroidal anti-inflammatory drugs can be helpful.
For the first couple of weeks after a cesarean, women should avoid
lifting anything heavier than their baby. To minimize pain during
breastfeeding, women should experiment with different breastfeeding
holds including the football hold and side-lying hold. Women who have had a caesarean are more likely to experience pain that
interferes with their usual activities than women who have vaginal
births, although by six months there is generally no longer a
difference. Pain during sexual intercourse is less likely than after vaginal birth; by six months there is no difference.
There may be a somewhat higher incidence of postnatal depression
in the first weeks after childbirth for women who have caesarean
sections, but this difference does not persist. Some women who have had caesarean sections, especially emergency caesareans, experience
post-traumatic stress disorder.
Usage
In Italy, the incidence of caesarean sections is particularly high, although it varies from region to region. In
Campania, 60% of 2008 births reportedly occurred via caesarean sections. In the
Rome region, the mean incidence is around 44%, but can reach as high as 85% in some private clinics.
With nearly 1.3 million stays, caesarean section was one of the
most common procedures performed in U.S. hospitals in 2011. It was the
second-most common procedure performed for people ages 18 to 44 years
old. Caesarean rates in the U.S. have risen considerably since 1996.
The procedure increased 60% from 1996 to 2009. In 2010, the caesarean
delivery rate was 32.8% of all births (a slight decrease from 2009's
high of 32.9% of all births).
A study found that in 2011, women covered by private insurance were 11%
more likely to have a caesarean section delivery than those covered by
Medicaid.
China has been cited as having the highest rates of C-sections in the world at 46% as of 2008.
Studies have shown that continuity of care with a known carer may significantly decrease the rate of caesarean delivery
but there is also research that appears to show that there is no
significant difference in Caesarean rates when comparing midwife
continuity care to conventional fragmented care.
More emergency caesareans—about 66%—are performed during the day rather than the night.
The rate has risen to 46% in
China and to levels of 25% and above in many Asian, European and Latin American countries. The rate has increased in the United States, to 33% of all births in 2012, up from 21% in 1996. Across Europe, there are differences between countries: in Italy the caesarean section rate is 40%, while in the
Nordic countries it is 14%. In Brazil and Iran the caesarean section rate is greater than 40%.
Increasing use
In the United States, C-section rates have increased from just over 20% in 1996 to 33% in 2011. This increase has not resulted in improved outcomes resulting in the position that C-sections may be done too frequently.
The World Health Organization officially withdrew its previous
recommendation of a 15% C-section rate in June 2010. Their official
statement read, "There is no empirical evidence for an optimum
percentage. What matters most is that all women who need caesarean
sections receive them."
Speculation explaining a relationship between birth weight and
maternal pelvis size has been proposed. The explanation, based on
Darwinian-inspired logic, states that since the advent of successful
caesarean birth more mothers with small pelvises and babies with large
birth weights survive. This hypothesis would predict an increased
average birth weight, which has been observed. It is unclear what
component contributes more to this effect; evolution or environment.
Brazil has one of the highest caesarean section rates in the
world, with rates in the public sector of 35–45%, and 80–90% in the
private sector.
Epidemiology
Global rates of caesarean section rates are increasing.
It doubled from 2003 to 2018 to reach 21%, and is increasing annually
by 4%. In southern Africa it is less than 5%; the rate is almost 60% in
some parts of Latin America. In the United Kingdom, in 2008, the rate was 24%. In Ireland the rate was 26.1% in 2009. The Canadian rate was 26% in 2005–2006. Australia has a high caesarean section rate, at 31% in 2007. In the United States the rate of C-section is around 33%, varying from 23% to 40% depending on the state.
One out three women who gave birth in the US delivered by caesarean in
2011. In 2012, close to 23 million C-sections were carried out globally. At one time a rate of 10% to 15% was thought to be ideal; a rate of 19% may result in better outcomes. More than 50 nations have rates greater than 27%. Another 45 countries have rates less than 7.5%. There are efforts to both improve access to and reduce the use of C-section. In the United States about 33% of deliveries are by C-section. The rates in the UK and Australia are 26.5% and 32.3% respectively. In China, the most recent CS rate reported was 41%.
Globally, 1% of all caesarean deliveries are carried out without
medical need. Overall, the caesarean section rate was 25.7% for
2004-2008.
Wound infections occur after caesarean sections at a rate of 3-15%.
Some women are at greater risk for developing a surgical site infection
after delivery. The presence of chorioamnionitis and obesity
predisposes the woman to develop a surgical site infection.
History
A baby being removed from its dying mother's womb
Caesarean section usually resulted in the death of the mother.
It was long considered an extreme measure, performed only when the
mother was already dead or considered to be beyond help. By way of
comparison, see the
resuscitative hysterotomy or perimortem caesarean section.
The mother of
Bindusara (born c. 320 BC, ruled 298 – c. 272 BC), the second
Mauryan Samrat (
emperor) of India, accidentally consumed poison and died when she was close to delivering him.
Chanakya,
the Chandragupta's teacher and adviser, made up his mind that the baby
should survive. He cut open the belly of the queen and took out the
baby, thus saving the baby's life.
An early account of caesarean section in Iran is mentioned in the book of
Shahnameh, written around 1000 AD, and relates to the birth of
Rostam, the legendary hero of that country. According to the Shahnameh, the
Simurgh instructed
Zal upon how to perform a caesarean section, thus saving
Rudaba and the child Rostam.
The
Babylonian Talmud, an ancient
Jewish religious text, mentions a procedure similar to the caesarean section. The procedure is termed
yotzei dofen. It also discusses at length the permissibility of performing a c-section on a dying or dead mother. There is also some basis for supposing that Jewish women regularly survived the operation in Roman times.
Pliny the Elder
theorized that Julius Caesar's name came from an ancestor who was born
by caesarean section, but the truth of this is debated (see the
discussion of
the etymology of Caesar).
The Ancient Roman caesarean section was first performed to remove a
baby from the womb of a mother who died during childbirth.
The
Catalan saint
Raymond Nonnatus (1204–1240) received his surname—from the
Latin non-natus ("not born")—because he was born by caesarean section. His mother died while giving birth to him.
In an account from the 1580s, in
Siegershausen, Switzerland,
Jakob Nufer a pig gelder, is supposed to have performed the operation on his wife after a prolonged labor, with her surviving. For most of the time since the 16th century, the procedure had a high mortality rate.
In Great Britain and Ireland, the mortality rate in 1865 was 85%. Key steps in reducing mortality were:
A caesarean section performed by indigenous healers in Kahura, Uganda. As observed by medical missionary Robert William Felkin in 1879.
European travelers in the
Great Lakes region of Africa during the 19th century observed caesarean sections being performed on a regular basis.
The expectant mother was normally anesthetized with alcohol, and herbal
mixtures were used to encourage healing. From the well-developed nature
of the procedures employed, European observers concluded they had been
employed for some time.
James Barry was the first European doctor to carry out a successful caesarean in Africa, while posted to Cape Town between 1817 and 1828.
The first successful caesarean section to be performed in the
United States took place in Mason County, Virginia (now Mason County,
West Virginia), in 1794. The procedure was performed by Dr.
Jesse Bennett on his wife Elizabeth.
Caesarius of Terracina
Saint Caesarius of Terracina, invoked for the good success of Caesarean delivery
The patron saint of caesarean section is
Caesarius of Africa, a young deacon martyred at Terracina, who has replaced and Christianized the pagan figure of Caesar. The martyr (Saint Cesareo in Italian) is invoked for the good success of this surgical procedure.
Society and culture
Etymology
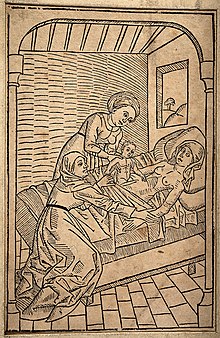
Fictional 15th-century depiction of the birth of Julius Caesar
The Roman
Lex Regia (royal law), later the
Lex Caesarea (imperial law), of
Numa Pompilius (715–673 BC), required the child of a mother dead in childbirth to be cut from her
womb.
There was a cultural taboo that mothers should not be buried pregnant, that may have reflected a way of saving some
fetuses.
Roman practice requiring a living mother to be in her tenth month of
pregnancy before resorting to the procedure, reflecting the knowledge
that she could not survive the delivery. Speculation that the Roman dictator
Julius Caesar was born by the method now known as C-section is apparently false. Although caesarean sections were performed in
Roman times, no classical source records a mother surviving such a delivery. As late as the 12th century, scholar and physician
Maimonides expresses doubt over the possibility of a woman's surviving this procedure and again falling pregnant. The term has also been explained as deriving from the verb
caedere, "to cut", with children delivered this way referred to as
caesones.
Pliny the Elder refers to a certain Julius Caesar (an ancestor of the famous Roman statesman) as
ab utero caeso, "cut from the womb" giving this as an explanation for the
cognomen "Caesar" which was then carried by his descendants. Nonetheless, even if the etymological hypothesis linking the caesarean section to Julius Caesar is a
false etymology, it has been widely believed. For example, the
Oxford English Dictionary defines caesarean birth as "the delivery of a child by cutting through the walls of the
abdomen when delivery cannot take place in the natural way, as was done in the case of Julius Caesar".
Merriam-Webster's Collegiate Dictionary
(11th edition) leaves room for etymological uncertainty with the
phrase, "from the legendary association of such a delivery with the
Roman cognomen
Caesar".
Some link with Julius Caesar or with Roman emperors exists in other languages as well. For example, the modern
German,
Norwegian,
Danish,
Dutch,
Swedish,
Finnish,
Turkish and
Hungarian terms are respectively
Kaiserschnitt,
keisersnitt,
kejsersnit,
keizersnede,
kejsarsnitt,
keisarinleikkaus,
sezaryen and
császármetszés (literally: "emperor's cut"). The German term has also been imported into
Japanese (帝王切開
teiōsekkai) and
Korean (제왕 절개
jewang jeolgae), both literally meaning "emperor incision". Similarly, in western Slavic (Polish)
cięcie cesarskie, (Czech)
císařský řez and (Slovak)
cisársky rez means "emperor's cut", whereas the south Slavic term is
Serbian царски рез and
Slovenian cárski réz, literally
tzar's cut. The
Russian term
kesarevo secheniye (Кесарево сечение
késarevo sečénije) literally means
Caesar's section. The Arabic term (ولادة قيصرية
wilaada qaySaríyya) also means "caesarean birth." The
Hebrew term ניתוח קיסרי (
nitúakh Keisári) translates literally as caesarean surgery. In Romania and Portugal, it is usually called
cesariana, meaning from (or related to)
Caesar.
Finally, the Roman
praenomen (given name)
Caeso
was said to be given to children who were born via C-section. While
this was probably just folk etymology made popular by Pliny the Elder,
it was well known by the time the term came into common use.
Spelling
The term
caesarean is spelled in various accepted ways,
as discussed at Wiktionary. The
Medical Subject Headings (MeSH) of the
United States National Library of Medicine (NLM) uses
cesarean section, while some other American medical works, e.g.
Saunders Comprehensive Veterinary Dictionary, use
caesarean, as do most British works. The online versions of the US-published
Merriam-Webster Dictionary and
American Heritage Dictionary list
cesarean first and other spellings as "variants", an etymologically anhistorical position.
Presence of father
In many hospitals, the mother's partner is encouraged to attend the surgery to support the mother and share the experience. The
anaesthetist will usually lower the drape temporarily as the child is delivered so the parents can see their newborn.
Special cases
In
Judaism, there is a dispute among the
poskim (Rabbinic authorities) as to whether the first-born son from a caesarean section has the laws of a
bechor. Traditionally, a male child delivered by caesarean is not eligible for the
Pidyon HaBen dedication ritual.
The mother may perform
a caesarean section on herself;
there have been successful cases, such as Inés Ramírez Pérez of Mexico
who, on 5 March 2000, performed a successful caesarean section on
herself. She survived, as did her son, Orlando Ruiz Ramírez.