| Schizophrenia | |
|---|---|
 |
|
| Self-portrait of a person with schizophrenia, representing that individual's perception of the distorted experience of reality in the disorder | |
| Pronunciation | |
| Specialty | Psychiatry, Psychology |
| Symptoms | False beliefs, confused thinking, hearing voices others do not[2][3] |
| Usual onset | Typically early adulthood[3] |
| Duration | Chronic[3] |
| Causes | Environmental and genetic factors[4] |
| Risk factors | Family history, cannabis use, problems during pregnancy, being raised in a city, older father[4] |
| Diagnostic method | Based on observed behavior, reported experiences, and reports of others familiar with the person[5] |
| Differential diagnosis | Substance misuse, Huntington's disease, mood disorders, autism[6] |
| Treatment | Counselling, job training[4][2] |
| Medication | Antipsychotics[4] |
| Prognosis | 18–20 years shorter life expectancy[7][8] due to increases in suicide, heart and lifestyle disease[8] |
| Frequency | ~0.5%[9] |
| Deaths | ~17,000 (2015)[10] |
Schizophrenia is a mental disorder characterized by abnormal social behavior and failure to understand reality.[2] Common symptoms include false beliefs, unclear or confused thinking, hearing voices that others do not, reduced social engagement and emotional expression, and a lack of motivation.[2][3] People with schizophrenia often have additional mental health problems such as anxiety, depressive, or substance-use disorders.[11] Symptoms typically come on gradually, begin in young adulthood, and last a long time.[3][5]
The causes of schizophrenia include environmental and genetic factors.[4] Possible environmental factors include being raised in a city, cannabis use during adolescence, certain infections, parental age and poor nutrition during pregnancy.[4][12] Genetic factors include a variety of common and rare genetic variants.[13] Diagnosis is based on observed behavior, the person's reported experiences and reports of others familiar with the person.[5] During diagnosis a person's culture must also be taken into account.[5] As of 2013 there is no objective test.[5] Schizophrenia does not imply a "split personality" or "dissociative identity disorder" – conditions with which it is often confused in public perception.[14]
The mainstay of treatment is antipsychotic medication, along with counselling, job training and social rehabilitation.[2][4] It is unclear whether typical or atypical antipsychotics are better.[15] In those who do not improve with other antipsychotics clozapine may be tried.[4] In more serious situations where there is risk to self or others involuntary hospitalization may be necessary, although hospital stays are now shorter and less frequent than they once were.[16]
About 0.3–0.7% of people are affected by schizophrenia during their lifetimes.[9] In 2013 there were an estimated 23.6 million cases globally.[17] Males are more often affected, and on average experience more severe symptoms.[2] About 20% of people do well and a few recover completely.[5] About 50% have lifelong impairment.[18] Social problems, such as long-term unemployment, poverty and homelessness are common.[5][19] The average life expectancy of people with the disorder is ten to twenty-five years less than for the general population.[7] This is the result of increased physical health problems and a higher suicide rate (about 5%).[9][20] In 2015 an estimated 17,000 people worldwide died from behavior related to, or caused by, schizophrenia.[10]
Signs and symptoms
My Eyes at the Moment of the Apparitions by German artist August Natterer, who had schizophrenia
Cloth embroidered by a person diagnosed with schizophrenia
Individuals with schizophrenia may experience hallucinations (most reported are hearing voices), delusions (often bizarre or persecutory in nature), and disorganized thinking and speech. The last may range from loss of train of thought, to sentences only loosely connected in meaning, to speech that is not understandable known as word salad. Social withdrawal, sloppiness of dress and hygiene, and loss of motivation and judgment are all common in schizophrenia.[21]
Distortions of self-experience such as feeling as if one's thoughts or feelings are not really one's own to believing thoughts are being inserted into one's mind, sometimes termed passivity phenomena, are also common.[22] There is often an observable pattern of emotional difficulty, for example lack of responsiveness.[23] Impairment in social cognition is associated with schizophrenia,[24] as are symptoms of paranoia. Social isolation commonly occurs.[25] Difficulties in working and long-term memory, attention, executive functioning, and speed of processing also commonly occur.[9] In one uncommon subtype, the person may be largely mute, remain motionless in bizarre postures, or exhibit purposeless agitation, all signs of catatonia.[26] People with schizophrenia often find facial emotion perception to be difficult.[27] It is unclear if the phenomenon called "thought blocking", where a talking person suddenly becomes silent for a few seconds to minutes, occurs in schizophrenia.[28][29]
About 30 to 50 percent of people with schizophrenia fail to accept that they have an illness or comply with their recommended treatment.[30] Treatment may have some effect on insight.[31]
People with schizophrenia may have a high rate of irritable bowel syndrome but they often do not mention it unless specifically asked.[32] Psychogenic polydipsia, or excessive fluid intake in the absence of physiological reasons to drink, is relatively common in people with schizophrenia.[33]
Symptom organization
Schizophrenia is often described in terms of positive and negative (or deficit) symptoms.[34] Positive symptoms are those that most individuals do not normally experience, but are present in people with schizophrenia. They can include delusions, disordered thoughts and speech, and tactile, auditory, visual, olfactory and gustatory hallucinations, typically regarded as manifestations of psychosis.[35] Hallucinations are also typically related to the content of the delusional theme.[36] Positive symptoms generally respond well to medication.[36]Negative symptoms are deficits of normal emotional responses or of other thought processes, and are less responsive to medication.[21] They commonly include flat expressions or little emotion, poverty of speech, inability to experience pleasure, lack of desire to form relationships, and lack of motivation. Negative symptoms appear to contribute more to poor quality of life, functional ability, and the burden on others than positive symptoms do.[18][37] People with greater negative symptoms often have a history of poor adjustment before the onset of illness, and response to medication is often limited.[21][38]
The validity of the positive and negative construct has been challenged by factor analysis studies observing a three dimension grouping of symptoms. While different terminology is used, a dimension for hallucinations, a dimension for disorganization, and a dimension for negative symptoms are usually described.[39]
Cognitive dysfunction
Deficits in cognitive abilities are widely recognized as a core feature of schizophrenia.[40][41][42] The extent of the cognitive deficits an individual experiences is a predictor of how functional an individual will be, the quality of occupational performance, and how successful the individual will be in maintaining treatment.[43] The presence and degree of cognitive dysfunction in individuals with schizophrenia has been reported to be a better indicator of functionality than the presentation of positive or negative symptoms.[40] The deficits impacting the cognitive function are found in a large number of areas: working memory, long-term memory,[44][45] verbal declarative memory,[46] semantic processing,[47] episodic memory,[43] attention,[18] learning (particularly verbal learning).[44] Deficits in verbal memory are the most pronounced in individuals with schizophrenia, and are not accounted for by deficit in attention. Verbal memory impairment has been linked to a decreased ability in individuals with schizophrenia to semantically encode (process information relating to meaning), which is cited as a cause for another known deficit in long-term memory.[44] When given a list of words, healthy individuals remember positive words more frequently (known as the Pollyanna principle); however, individuals with schizophrenia tend to remember all words equally regardless of their connotations, suggesting that the experience of anhedonia impairs the semantic encoding of the words.[44] These deficits have been found in individuals before the onset of the illness to some extent.[40][42][48] First-degree family members of individuals with schizophrenia and other high-risk individuals also show a degree of deficit in cognitive abilities, and specifically in working memory.[48] A review of the literature on cognitive deficits in individuals with schizophrenia shows that the deficits may be present in early adolescence, or as early as childhood.[40] The deficits which an individual with schizophrenia presents tend to remain the same over time in most patients, or follow an identifiable course based upon environmental variables.[40][44]Although the evidence that cognitive deficits remain stable over time is reliable and abundant,[43][44] much of the research in this domain focuses on methods to improve attention and working memory.[44][45] Efforts to improve learning ability in individuals with schizophrenia using a high- versus low-reward condition and an instruction-absent or instruction-present condition revealed that increasing reward leads to poorer performance while providing instruction leads to improved performance, highlighting that some treatments may exist to increase cognitive performance.[44] Training individuals with schizophrenia to alter their thinking, attention, and language behaviors by verbalizing tasks, engaging in cognitive rehearsal, giving self-instructions, giving coping statements to the self to handle failure, and providing self-reinforcement for success, significantly improves performance on recall tasks.[44] This type of training, known as self-instructional (SI) training, produced benefits such as lower number of nonsense verbalizations and improved recall while distracted.[44]
Onset
Late adolescence and early adulthood are peak periods for the onset of schizophrenia,[9] critical years in a young adult's social and vocational development.[49] In 40% of men and 23% of women diagnosed with schizophrenia, the condition manifested itself before the age of 19.[50] The onset of the disease is usually later in women than in men.[51] To minimize the developmental disruption associated with schizophrenia, much work has recently been done to identify and treat the prodromal (pre-onset) phase of the illness, which has been detected up to 30 months before the onset of symptoms.[49] Those who go on to develop schizophrenia may experience transient or self-limiting psychotic symptoms[52] and the non-specific symptoms of social withdrawal, irritability, dysphoria,[53] and clumsiness before the onset of the disease.[54] Children who go on to develop schizophrenia may also demonstrate decreased intelligence, decreased motor development (reaching milestones such as walking slowly), isolated play preference, social anxiety, and poor school performance.[55][56][57]Causes
A combination of genetic and environmental factors play a role in the development of schizophrenia.[9][14] People with a family history of schizophrenia who have a transient psychosis have a 20–40% chance of being diagnosed one year later.[58]Genetic
Estimates of the heritability of schizophrenia is around 80%, which implies that 80% of the individual differences in risk to schizophrenia is explained by individual differences in genetics.[59] These estimates vary because of the difficulty in separating genetic and environmental influences.[60] The greatest single risk factor for developing schizophrenia is having a first-degree relative with the disease (risk is 6.5%); more than 40% of monozygotic twins of those with schizophrenia are also affected.[14] If one parent is affected the risk is about 13% and if both are affected the risk is nearly 50%.[59]Many genes are known to be involved in schizophrenia, each of small effect and unknown transmission and expression.[13][61] The summation of these effect sizes into a polygenic risk score can explain at least 7% of the variability in liability for schizophrenia.[62] Around 5% of cases of schizophrenia are understood to be at least partially attributable to rare copy number variants (CNVs), including 22q11, 1q21 and 16p11.[63] These rare CNVs increase the risk of an individual developing the disorder by as much as 20-fold, and are frequently comorbid with autism and intellectual disabilities.[63] There is a genetic relation between the common variants which cause schizophrenia and bipolar disorder, an inverse genetic correlation with intelligence and no genetic correlation with immune disorders.[64]
Environment
Environmental factors associated with the development of schizophrenia include the living environment, drug use, and prenatal stressors.[9]Maternal stress has been associated with an increased risk of schizophrenia, possibly in association with reelin. Maternal Stress has been observed to lead to hypermethylation and therefore under-expression of reelin, which in animal models leads to reduction in GABAergic neurons, a common finding in schizophrenia.[65] Maternal nutritional deficiencies, such as those observed during a famine, as well as maternal obesity have also been identified as possible risk factors for schizophrenia. Both maternal stress and infection have been demonstrated to alter fetal neurodevelopment through pro-inflammatory proteins such as IL-8 and TNF.[66][67]
Parenting style seems to have no major effect, although people with supportive parents do better than those with critical or hostile parents.[14] Childhood trauma, death of a parent, and being bullied or abused increase the risk of psychosis.[68] Living in an urban environment during childhood or as an adult has consistently been found to increase the risk of schizophrenia by a factor of two,[9][14] even after taking into account drug use, ethnic group, and size of social group.[69] Other factors that play an important role include social isolation and immigration related to social adversity, racial discrimination, family dysfunction, unemployment, and poor housing conditions.[14][70]
It has been hypothesized that in some people, development of schizophrenia is related to intestinal tract dysfunction such as seen with non-celiac gluten sensitivity or abnormalities in the intestinal flora.[71] A subgroup of persons with schizophrenia present an immune response to gluten different from that found in people with celiac, with elevated levels of certain serum biomarkers of gluten sensitivity such as anti-gliadin IgG or anti-gliadin IgA antibodies.[72]
Substance use
About half of those with schizophrenia use drugs or alcohol excessively.[73] Amphetamine, cocaine, and to a lesser extent alcohol, can result in a transient stimulant psychosis or alcohol-related psychosis that presents very similarly to schizophrenia.[14][74] Although it is not generally believed to be a cause of the illness, people with schizophrenia use nicotine at much higher rates than the general population.[75]Alcohol abuse can occasionally cause the development of a chronic, substance-induced psychotic disorder via a kindling mechanism.[76] Alcohol use is not associated with an earlier onset of psychosis.[77]
Cannabis can be a contributory factor in schizophrenia,[12][78][79] potentially causing the disease in those who are already at risk.[79] The increased risk may require the presence of certain genes within an individual[79] or may be related to preexisting psychopathology.[12] Early exposure is strongly associated with an increased risk.[12] The size of the increased risk is not clear,[80] but appears to be in the range of two to three times greater for psychosis.[78] Higher dosage and greater frequency of use are indicators of increased risk of chronic psychoses.[78]
Other drugs may be used only as coping mechanisms by individuals who have schizophrenia, to deal with depression, anxiety, boredom, and loneliness.[73][81]
Developmental factors
Factors such as hypoxia and infection, or stress and malnutrition in the mother during fetal development, may result in a slight increase in the risk of schizophrenia later in life.[9] People diagnosed with schizophrenia are more likely to have been born in winter or spring (at least in the northern hemisphere), which may be a result of increased rates of viral exposures in utero.[14] The increased risk is about five to eight percent.[82] Other infections during pregnancy or around the time of birth that may increase the risk include Toxoplasma gondi and Chlamydia.[83]Mechanisms
A number of attempts have been made to explain the link between altered brain function and schizophrenia.[9] One of the most common is the dopamine hypothesis, which attributes psychosis to the mind's faulty interpretation of the misfiring of dopaminergic neurons.[9]Psychological
Many psychological mechanisms have been implicated in the development and maintenance of schizophrenia. Cognitive biases have been identified in those with the diagnosis or those at risk, especially when under stress or in confusing situations.[84] Some cognitive features may reflect global neurocognitive deficits such as memory loss, while others may be related to particular issues and experiences.[85][86]Despite a demonstrated appearance of blunted affect, recent findings indicate that many individuals diagnosed with schizophrenia are emotionally responsive, particularly to stressful or negative stimuli, and that such sensitivity may cause vulnerability to symptoms or to the disorder.[87][88] Some evidence suggests that the content of delusional beliefs and psychotic experiences can reflect emotional causes of the disorder, and that how a person interprets such experiences can influence symptomatology.[89][90][91] The use of "safety behaviors" (acts such as gestures or the use of words in specific contexts) to avoid or neutralize imagined threats may actually contribute to the chronicity of delusions.[92] Further evidence for the role of psychological mechanisms comes from the effects of psychotherapies on symptoms of schizophrenia.[93]
Neurological
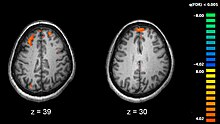
Functional magnetic resonance imaging
(fMRI) showing two levels of the brain; areas in orange were more
active in healthy controls than in medicated people with schizophrenia.
People with schizophrenia who are medication compliant have an association with enlarged lateral ventricles in the brain.[94]
Schizophrenia is associated with subtle differences in brain structures, found in forty to fifty percent of cases, and in brain chemistry during acute psychotic states.[9] Studies using neuropsychological tests and brain imaging technologies such as fMRI and PET to examine functional differences in brain activity have shown that differences seem to occur most commonly in the frontal lobes, hippocampus and temporal lobes.[95] Reductions in brain volume are most pronounced in grey matter structures, and correlate with duration of illness, although white matter abnormalities have also been found. A progressive increase in ventricular volume as well as a progressive reduction in grey matter in the frontal, parietal, and temporal lobes has also been observed.[96][97] These differences have been linked to the neurocognitive deficits often associated with schizophrenia.[98] Because neural circuits are altered, it has alternatively been suggested that schizophrenia could be thought of as a neurodevelopmental disorder with psychosis occurring as a possibly preventable late stage.[99] There has been debate on whether treatment with antipsychotics can itself cause reduction of brain volume.[100]
Particular attention has been paid to the function of dopamine in the mesolimbic pathway of the brain. This focus largely resulted from the accidental finding that phenothiazine drugs, which block dopamine function, could reduce psychotic symptoms. It is also supported by the fact that amphetamines, which trigger the release of dopamine, may exacerbate the psychotic symptoms in schizophrenia.[101] The influential dopamine hypothesis of schizophrenia proposed that excessive activation of D2 receptors was the cause of (the positive symptoms of) schizophrenia. Although postulated for about 20 years based on the D2 blockade effect common to all antipsychotics, it was not until the mid-1990s that PET and SPET imaging studies provided supporting evidence. While dopamine D2/D3 receptors are elevated in schizophrenia, the effect size is small, and only evident in medication naive schizophrenics. On the other hand, presynaptic dopamine metabolism and release is elevated despite no difference in dopamine transporter.[102] The altered synthesis of dopamine in the nigrostriatal system have been confirmed in several human studies.[103][104] Hypoactivity of dopamine D1 receptor activation in the prefrontal cortex has also been observed.[105] The hyperactivity of D2 receptor stimulation and relative hypoactivity of D1 receptor stimulation is thought to contribute to cognitive dysfunction by disrupting signal to noise ratio in cortical microcircuits.[106] The dopamine hypothesis is now thought to be simplistic, partly because newer antipsychotic medication (atypical antipsychotic medication) can be just as effective as older medication (typical antipsychotic medication), but also affects serotonin function and may have slightly less of a dopamine blocking effect.[107]
Interest has also focused on the neurotransmitter glutamate and the reduced function of the NMDA glutamate receptor in schizophrenia, largely because of the abnormally low levels of glutamate receptors found in the postmortem brains of those diagnosed with schizophrenia,[108] and the discovery that glutamate-blocking drugs such as phencyclidine and ketamine can mimic the symptoms and cognitive problems associated with the condition.[109] Reduced glutamate function is linked to poor performance on tests requiring frontal lobe and hippocampal function, and glutamate can affect dopamine function, both of which have been implicated in schizophrenia; this has suggested an important mediating (and possibly causal) role of glutamate pathways in the condition.[110] But positive symptoms fail to respond to glutamatergic medication.[111] Closely related to evidence of glutamate dysfunction in schizophrenia is the observed changes GABAergic transmission. Post-Mortem studies demonstrate decreased expression of GAD67, GAT-1 and GABAA receptor subunits in the prefrontal cortex, although this appears to be restricted to a certain subsets of parvalbumin containing GABAergic neurons. While in vivo imaging of GABAergic signaling appears to be moderately reduced, this may be dependent upon treatment and disease stage.[112]
Diagnosis
Schizophrenia is diagnosed based on criteria in either the American Psychiatric Association's (APA) fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM 5), or the World Health Organization's International Statistical Classification of Diseases and Related Health Problems (ICD-10). These criteria use the self-reported experiences of the person and reported abnormalities in behavior, followed by a clinical assessment by a mental health professional. Symptoms associated with schizophrenia occur along a continuum in the population and must reach a certain severity and level of impairment, before a diagnosis is made.[14] As of 2013 there is no objective test.[5]Criteria
In 2013, the American Psychiatric Association released the fifth edition of the DSM (DSM-5). To be diagnosed with schizophrenia, two diagnostic criteria have to be met over much of the time of a period of at least one month, with a significant impact on social or occupational functioning for at least six months. The person had to be suffering from delusions, hallucinations, or disorganized speech. A second symptom could be negative symptoms, or severely disorganized or catatonic behaviour.[113] The definition of schizophrenia remained essentially the same as that specified by the 2000 version of DSM (DSM-IV-TR), but DSM-5 makes a number of changes.- Subtype classifications – such as catatonic and paranoid schizophrenia – are removed. These were retained in previous revisions largely for reasons of tradition, but had subsequently proved to be of little worth.[114]
- Catatonia is no longer so strongly associated with schizophrenia.[115]
- In describing a person's schizophrenia, it is recommended that a better distinction be made between the current state of the condition and its historical progress, to achieve a clearer overall characterization.[114]
- Special treatment of Schneider's first-rank symptoms is no longer recommended.[114]
- Schizoaffective disorder is better defined to demarcate it more cleanly from schizophrenia.[114]
- An assessment covering eight domains of psychopathology – such as whether hallucination or mania is experienced – is recommended to help clinical decision-making.[116]
If signs of disturbance are present for more than a month but less than six months, the diagnosis of schizophreniform disorder is applied. Psychotic symptoms lasting less than a month may be diagnosed as brief psychotic disorder, and various conditions may be classed as psychotic disorder not otherwise specified, while schizoaffective disorder is diagnosed if symptoms of mood disorder are substantially present alongside psychotic symptoms. If the psychotic symptoms are the direct physiological result of a general medical condition or a substance, then the diagnosis is one of a psychosis secondary to that condition.[113] Schizophrenia is not diagnosed if symptoms of pervasive developmental disorder are present unless prominent delusions or hallucinations are also present.[113]
Subtypes
With the publication of DSM-5, the APA removed all sub-classifications of schizophrenia.[118] The five sub-classifications included in DSM-IV-TR were:[119][120]- Paranoid type: Delusions or auditory hallucinations are present, but thought disorder, disorganized behavior, or affective flattening are not. Delusions are persecutory and/or grandiose, but in addition to these, other themes such as jealousy, religiosity, or somatization may also be present. (DSM code 295.3/ICD code F20.0)
- Disorganized type: Named hebephrenic schizophrenia in the ICD. Where thought disorder and flat affect are present together. (DSM code 295.1/ICD code F20.1)
- Catatonic type: The subject may be almost immobile or exhibit agitated, purposeless movement. Symptoms can include catatonic stupor and waxy flexibility. (DSM code 295.2/ICD code F20.2)
- Undifferentiated type: Psychotic symptoms are present but the criteria for paranoid, disorganized, or catatonic types have not been met. (DSM code 295.9/ICD code F20.3)
- Residual type: Where positive symptoms are present at a low intensity only. (DSM code 295.6/ICD code F20.5)
- Post-schizophrenic depression: A depressive episode arising in the aftermath of a schizophrenic illness where some low-level schizophrenic symptoms may still be present. (ICD code F20.4)
- Simple schizophrenia: Insidious and progressive development of prominent negative symptoms with no history of psychotic episodes. (ICD code F20.6)
- Other schizophrenia include cenesthopathic schizophrenia and schizophreniform disorder NOS (ICD code F20.8).[121]
Differential diagnosis
Psychotic symptoms may be present in several other mental disorders, including bipolar disorder,[122] borderline personality disorder,[123] drug intoxication, and drug-induced psychosis. Delusions ("non-bizarre") are also present in delusional disorder, and social withdrawal in social anxiety disorder, avoidant personality disorder and schizotypal personality disorder. Schizotypal personality disorder has symptoms that are similar but less severe than those of schizophrenia.[5] Schizophrenia occurs along with obsessive-compulsive disorder (OCD) considerably more often than could be explained by chance, although it can be difficult to distinguish obsessions that occur in OCD from the delusions of schizophrenia.[124] A few people withdrawing from benzodiazepines experience a severe withdrawal syndrome which may last a long time. It can resemble schizophrenia and be misdiagnosed as such.[125]A more general medical and neurological examination may be needed to rule out medical illnesses which may rarely produce psychotic schizophrenia-like symptoms, such as metabolic disturbance, systemic infection, syphilis, AIDS dementia complex, epilepsy, limbic encephalitis, and brain lesions. Stroke, multiple sclerosis, hyperthyroidism, hypothyroidism, and dementias such as Alzheimer's disease, Huntington's disease, frontotemporal dementia, and the Lewy body dementias may also be associated with schizophrenia-like psychotic symptoms.[126] It may be necessary to rule out a delirium, which can be distinguished by visual hallucinations, acute onset and fluctuating level of consciousness, and indicates an underlying medical illness. Investigations are not generally repeated for relapse unless there is a specific medical indication or possible adverse effects from antipsychotic medication. In children hallucinations must be separated from typical childhood fantasies.[5]
Prevention
Prevention of schizophrenia is difficult as there are no reliable markers for the later development of the disorder.[127] There is tentative evidence for the effectiveness of early interventions to prevent schizophrenia.[128] While there is some evidence that early intervention in those with a psychotic episode may improve short-term outcomes, there is little benefit from these measures after five years.[9] Attempting to prevent schizophrenia in the prodrome phase is of uncertain benefit and therefore as of 2009 is not recommended.[129] Cognitive behavioral therapy may reduce the risk of psychosis in those at high risk after a year[130] and is recommended in this group, by the National Institute for Health and Care Excellence (NICE).[131] Another preventative measure is to avoid drugs that have been associated with development of the disorder, including cannabis, cocaine, and amphetamines.[14]Management
The primary treatment of schizophrenia is antipsychotic medications, often in combination with psychological and social supports.[9] Hospitalization may occur for severe episodes either voluntarily or (if mental health legislation allows it) involuntarily. Long-term hospitalization is uncommon since deinstitutionalization beginning in the 1950s, although it still occurs.[16] Community support services including drop-in centers, visits by members of a community mental health team, supported employment[132] and support groups are common. Some evidence indicates that regular exercise has a positive effect on the physical and mental health of those with schizophrenia.[133]Medication
Risperidone (trade name Risperdal) is a common atypical antipsychotic medication.
The first-line psychiatric treatment for schizophrenia is antipsychotic medication,[134] which can reduce the positive symptoms of psychosis in about 7 to 14 days. Antipsychotics, however, fail to significantly improve the negative symptoms and cognitive dysfunction.[38][135] In those on antipsychotics, continued use decreases the risk of relapse.[136][137] There is little evidence regarding effects from their use beyond two or three years.[137] However use of anti-psychotics can lead to dopamine hypersensitivity increasing the risk of symptoms if antipsychotics are stopped.[138]
The choice of which antipsychotic to use is based on benefits, risks, and costs.[9] It is debatable whether, as a class, typical or atypical antipsychotics are better.[15][139] Amisulpride, olanzapine, risperidone, and clozapine may be more effective but are associated with greater side effects.[140] Typical antipsychotics have equal drop-out and symptom relapse rates to atypicals when used at low to moderate dosages.[141] There is a good response in 40–50%, a partial response in 30–40%, and treatment resistance (failure of symptoms to respond satisfactorily after six weeks to two or three different antipsychotics) in 20% of people.[38] Clozapine is an effective treatment for those who respond poorly to other drugs ("treatment-resistant" or "refractory" schizophrenia),[142] but it has the potentially serious side effect of agranulocytosis (lowered white blood cell count) in less than 4% of people.[9][14][143]
Most people on antipsychotics have side effects. People on typical antipsychotics tend to have a higher rate of extrapyramidal side effects, while some atypicals are associated with considerable weight gain, diabetes and risk of metabolic syndrome; this is most pronounced with olanzapine, while risperidone and quetiapine are also associated with weight gain.[140] Risperidone has a similar rate of extrapyramidal symptoms to haloperidol.[140] It remains unclear whether the newer antipsychotics reduce the chances of developing neuroleptic malignant syndrome or tardive dyskinesia, a rare but serious neurological disorder.[144]
For people who are unwilling or unable to take medication regularly, long-acting depot preparations of antipsychotics may be used to achieve control.[145] They reduce the risk of relapse to a greater degree than oral medications.[136] When used in combination with psychosocial interventions, they may improve long-term adherence to treatment.[145] The American Psychiatric Association suggests considering stopping antipsychotics in some people if there are no symptoms for more than a year.[137]
Psychosocial
A number of psychosocial interventions may be useful in the treatment of schizophrenia including: family therapy,[146] assertive community treatment, supported employment, cognitive remediation,[147] skills training, token economic interventions, and psychosocial interventions for substance use and weight management.[148] Family therapy or education, which addresses the whole family system of an individual, may reduce relapses and hospitalizations.[146] Evidence for the effectiveness of cognitive-behavioral therapy (CBT) in either reducing symptoms or preventing relapse is minimal.[149][150] Evidence for metacognitive training is mixed with some reviews finding benefit and another not.[151][152][153] Art or drama therapy have not been well-researched.[154][155]Prognosis
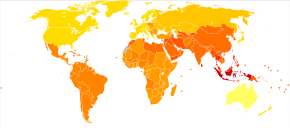
Disability-adjusted life years lost due to schizophrenia per 100,000 inhabitants in 2004.
no data
≤ 185
185–197
197–207
207–218
218–229
229–240
|
240–251
251–262
262–273
273–284
284–295
≥ 295
|
Schizophrenia has great human and economic costs.[9] It results in a decreased life expectancy by 10–25 years.[7] This is primarily because of its association with obesity, poor diet, sedentary lifestyles, and smoking, with an increased rate of suicide playing a lesser role.[9][7][156] Antipsychotic medications may also increase the risk.[7] These differences in life expectancy increased between the 1970s and 1990s.[157]
Schizophrenia is a major cause of disability, with active psychosis ranked as the third-most-disabling condition after quadriplegia and dementia and ahead of paraplegia and blindness.[158] Approximately three-fourths of people with schizophrenia have ongoing disability with relapses[38] and 16.7 million people globally are deemed to have moderate or severe disability from the condition.[159] Some people do recover completely and others function well in society.[160] Most people with schizophrenia live independently with community support.[9] About 85% are unemployed.[4] Some evidence suggests that paranoid schizophrenia may have a better prospect than other types of schizophrenia for independent living and occupational functioning.[161] In people with a first episode of psychosis a good long-term outcome occurs in 42%, an intermediate outcome in 35% and a poor outcome in 27%.[162] Outcomes for schizophrenia appear better in the developing than the developed world.[163] These conclusions, however, have been questioned.[164][165]
There is a higher than average suicide rate associated with schizophrenia. This has been cited at 10%, but a more recent analysis revises the estimate to 4.9%, most often occurring in the period following onset or first hospital admission.[20][166] Several times more (20 to 40%) attempt suicide at least once.[5][167] There are a variety of risk factors, including male gender, depression, and a high intelligence quotient.[167]
Schizophrenia and smoking have shown a strong association in studies worldwide.[168][169] Use of cigarettes is especially high in individuals diagnosed with schizophrenia, with estimates ranging from 80 to 90% being regular smokers, as compared to 20% of the general population.[169] Those who smoke tend to smoke heavily, and additionally smoke cigarettes with high nicotine content.[170] Among people with schizophrenia use of cannabis is also common.[73]
Epidemiology
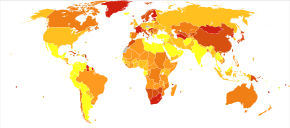
Deaths per million persons due to schizophrenia in 2012.
0–0
1–1
2–2
3–3
4–6
7–20
Schizophrenia affects around 0.3–0.7% of people at some point in their life,[9] or 24 million people worldwide as of 2011.[171] It occurs 1.4 times more frequently in males than females and typically appears earlier in men[14]—the peak ages of onset are 25 years for males and 27 years for females.[172] Onset in childhood is much rarer,[173] as is onset in middle or old age.[174]
Despite the prior belief that schizophrenia occurs at similar rates worldwide, its frequency varies across the world,[5][175] within countries,[176] and at the local and neighborhood level.[177] This variation has been estimated to be fivefold.[4] It causes approximately one percent of worldwide disability adjusted life years[14] and resulted in 20,000 deaths in 2010.[178] The rate of schizophrenia varies up to threefold depending on how it is defined.[9]
In 2000, the World Health Organization found the percentage of people affected and the number of new cases that develop each year is roughly similar around the world, with age-standardized prevalence per 100,000 ranging from 343 in Africa to 544 in Japan and Oceania for men, and from 378 in Africa to 527 in Southeastern Europe for women.[179] About 1.1% of adults have schizophrenia in the United States.[180]
History

The term "schizophrenia" was coined by Eugen Bleuler.
In the early 20th century, the psychiatrist Kurt Schneider listed the forms of psychotic symptoms that he thought distinguished schizophrenia from other psychotic disorders. These are called first-rank symptoms or Schneider's first-rank symptoms. They include delusions of being controlled by an external force, the belief that thoughts are being inserted into or withdrawn from one's conscious mind, the belief that one's thoughts are being broadcast to other people, and hearing hallucinatory voices that comment on one's thoughts or actions or that have a conversation with other hallucinated voices.[181] Although they have significantly contributed to the current diagnostic criteria, the specificity of first-rank symptoms has been questioned. A review of the diagnostic studies conducted between 1970 and 2005 found that they allow neither a reconfirmation nor a rejection of Schneider's claims, and suggested that first-rank symptoms should be de-emphasized in future revisions of diagnostic systems.[182] The absence of first-rank symptoms should raise suspicion of a medical disorder, however.[22]
The history of schizophrenia is complex and does not lend itself easily to a linear narrative.[183] Accounts of a schizophrenia-like syndrome are thought to be rare in historical records before the 19th century, although reports of irrational, unintelligible, or uncontrolled behavior were common. A detailed case report in 1797 concerning James Tilly Matthews, and accounts by Philippe Pinel published in 1809, are often regarded as the earliest cases of the illness in the medical and psychiatric literature.[184] The Latinized term dementia praecox was first used by German alienist Heinrich Schule in 1886 and then in 1891 by Arnold Pick in a case report of a psychotic disorder (hebephrenia). In 1893 Emil Kraepelin borrowed the term from Schule and Pick and in 1899 introduced a broad new distinction in the classification of mental disorders between dementia praecox and mood disorder (termed manic depression and including both unipolar and bipolar depression).[185] Kraepelin believed that dementia praecox was probably caused by a long-term, smouldering systemic or "whole body" disease process that affected many organs and peripheral nerves in the body but which affected the brain after puberty in a final decisive cascade.[186] His use of the term "praecox" distinguished it from other forms of dementia such as Alzheimer's disease which typically occur later in life.[187] It is sometimes argued that the use of the term démence précoce in 1852 by the French physician Bénédict Morel constitutes the medical discovery of schizophrenia. However, this account ignores the fact that there is little to connect Morel's descriptive use of the term and the independent development of the dementia praecox disease concept at the end of the nineteenth century.[188]
A molecule of chlorpromazine (trade name Thorazine), which revolutionized treatment of schizophrenia in the 1950s
The word schizophrenia—which translates roughly as "splitting of the mind" and comes from the Greek roots schizein (σχίζειν, "to split") and phrēn, phren- (φρήν, φρεν-, "mind")[189]—was coined by Eugen Bleuler in 1908 and was intended to describe the separation of function between personality, thinking, memory, and perception. American and British interpretations of Bleuler led to the claim that he described its main symptoms as four A's: flattened affect, autism, impaired association of ideas, and ambivalence.[190][191] Bleuler realized that the illness was not a dementia, as some of his patients improved rather than deteriorated, and thus proposed the term schizophrenia instead. Treatment was revolutionized in the mid-1950s with the development and introduction of chlorpromazine.[192]
In the early 1970s, the diagnostic criteria for schizophrenia were the subject of a number of controversies which eventually led to the operational criteria used today. It became clear after the 1971 US–UK Diagnostic Study that schizophrenia was diagnosed to a far greater extent in America than in Europe.[193] This was partly due to looser diagnostic criteria in the US, which used the DSM-II manual, contrasting with Europe and its ICD-9. David Rosenhan's 1972 study, published in the journal Science under the title "On being sane in insane places", concluded that the diagnosis of schizophrenia in the US was often subjective and unreliable.[194] These were some of the factors leading to the revision not only of the diagnosis of schizophrenia, but the revision of the whole DSM manual, resulting in the publication of the DSM-III in 1980.[195]
The term schizophrenia is commonly misunderstood to mean that affected persons have a "split personality". Although some people diagnosed with schizophrenia may hear voices and may experience the voices as distinct personalities, schizophrenia does not involve a person changing among distinct, multiple personalities; the confusion arises in part due to the literal interpretation of Bleuler's term "schizophrenia" (Bleuler originally associated schizophrenia with dissociation, and included split personality in his category of schizophrenia).[196][197] Dissociative identity disorder (having a "split personality") was also often misdiagnosed as schizophrenia based on the loose criteria in the DSM-II.[197][198] The first known misuse of the term to mean "split personality" was in an article by the poet T. S. Eliot in 1933.[199] Other scholars have traced earlier roots.[200] Rather, the term means a "splitting of mental functions", reflecting the presentation of the illness.[201]
Society and culture

John Nash, an American mathematician and joint recipient of the 1994 Nobel Prize for Economics, who had schizophrenia. His life was the subject of the 2001 Academy Award-winning film A Beautiful Mind.
In 2002, the term for schizophrenia in Japan was changed from seishin-bunretsu-byō (精神分裂病, lit. "mind-split disease") to tōgō-shitchō-shō (統合失調症, lit. "integration disorder") to reduce stigma.[202] The new name was inspired by the biopsychosocial model; it increased the percentage of people who were informed of the diagnosis from 37 to 70% over three years.[203] A similar change was made in South Korea in 2012.[204] A professor of psychiatry, Jim van Os, has proposed changing the English term to "psychosis spectrum syndrome".[205]
In the United States, the cost of schizophrenia—including direct costs (outpatient, inpatient, drugs, and long-term care) and non-health care costs (law enforcement, reduced workplace productivity, and unemployment)—was estimated to be $62.7 billion in 2002.[206] The book and film A Beautiful Mind chronicles the life of John Forbes Nash, a mathematician who won the Nobel Prize for Economics and was diagnosed with schizophrenia.
Violence
Individuals with severe mental illness, including schizophrenia, are at a significantly greater risk of being victims of both violent and non-violent crime.[207] Schizophrenia has been associated with a higher rate of violent acts, but most appear to be related to associated substance abuse.[208] Rates of homicide linked to psychosis are similar to those linked to substance misuse, and parallel the overall rate in a region.[209] What role schizophrenia has on violence independent of drug misuse is controversial, but certain aspects of individual histories or mental states may be factors.[210] About 11% of people in prison for homicide have schizophrenia while 21% have mood disorders.[211] Another study found about 8-10% of people with schizophrenia had committed a violent act in the past year compared to 2% of the general population.[211]Media coverage relating to violent acts by individuals with schizophrenia reinforces public perception of an association between schizophrenia and violence.[208] In a large, representative sample from a 1999 study, 12.8% of Americans believed that individuals with schizophrenia were "very likely" to do something violent against others, and 48.1% said that they were "somewhat likely" to. Over 74% said that people with schizophrenia were either "not very able" or "not able at all" to make decisions concerning their treatment, and 70.2% said the same of money-management decisions.[212] The perception of individuals with psychosis as violent has more than doubled in prevalence since the 1950s, according to one meta-analysis.[213]