hemoglobin
(heterotetramer, (αβ)2)
| ||
| ||
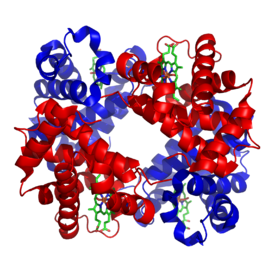
| Structure of human hemoglobin. α and β subunits are in red and blue, and the iron-containing heme groups in green. From PDB: 1GZX Proteopedia Hemoglobin | ||
| − | ||
| Protein type | metalloprotein, globulin | |
| Function | oxygen-transport | |
| Cofactor(s) | heme (4) | |
| − | ||
| Subunit name |
Gene | Chromosomal locus |
| Hb-α1 | HBA1 | Chr. 16 p13.3 |
| Hb-α2 | HBA2 | Chr. 16 p13.3 |
| Hb-β | HBB | Chr. 11 p15.5 |
Hemoglobin, abbreviated Hb or Hgb, is the iron-containing oxygen-transport metalloprotein in the red blood cells (erythrocytes) of almost all vertebrates (the exception being the fish family Channichthyidae) as well as the tissues of some invertebrates. Haemoglobin in the blood carries oxygen from the lungs or gills to the rest of the body (i.e. the tissues). There it releases the oxygen to permit aerobic respiration to provide energy to power the functions of the organism in the process called metabolism. A healthy individual has 12 to 16 grams of haemoglobin in every 100 ml of blood.
In mammals, the protein makes up about 96% of the red blood cells' dry content (by weight), and around 35% of the total content (including water). Hemoglobin has an oxygen-binding capacity of 1.34 mL O2 per gram, which increases the total blood oxygen capacity seventy-fold compared to dissolved oxygen in blood. The mammalian hemoglobin molecule can bind (carry) up to four oxygen molecules.
Hemoglobin is involved in the transport of other gases: It carries some of the body's respiratory carbon dioxide (about 20–25% of the total) as carbaminohemoglobin, in which CO2 is bound to the heme protein. The molecule also carries the important regulatory molecule nitric oxide bound to a globin protein thiol group, releasing it at the same time as oxygen.
Hemoglobin is also found outside red blood cells and their progenitor lines. Other cells that contain hemoglobin include the A9 dopaminergic neurons in the substantia nigra, macrophages, alveolar cells, lungs, retinal pigment epithelium, hepatocytes, mesangial cells in the kidney, endometrial cells, cervical cells and vaginal epithelial cells. In these tissues, hemoglobin has a non-oxygen-carrying function as an antioxidant and a regulator of iron metabolism.
Hemoglobin and hemoglobin-like molecules are also found in many invertebrates, fungi, and plants. In these organisms, hemoglobins may carry oxygen, or they may act to transport and regulate other small molecules and ions such as carbon dioxide, nitric oxide, hydrogen sulfide and sulfide. A variant of the molecule, called leghemoglobin, is used to scavenge oxygen away from anaerobic systems, such as the nitrogen-fixing nodules of leguminous plants, before the oxygen can poison (deactivate) the system.
Research history
Max Perutz, one of the founding fathers of molecular biology
In 1825 J. F. Engelhard discovered that the ratio of iron to protein is identical in the hemoglobins of several species. From the known atomic mass of iron he calculated the molecular mass of hemoglobin to n × 16000 (n
= number of iron atoms per hemoglobin, now known to be 4), the first
determination of a protein's molecular mass. This "hasty conclusion"
drew a lot of ridicule at the time from scientists who could not believe
that any molecule could be that big. Gilbert Smithson Adair confirmed Engelhard's results in 1925 by measuring the osmotic pressure of hemoglobin solutions.
The oxygen-carrying property of hemoglobin was discovered by Hünefeld in 1840. In 1851, German physiologist Otto Funke
published a series of articles in which he described growing hemoglobin
crystals by successively diluting red blood cells with a solvent such
as pure water, alcohol or ether, followed by slow evaporation of the
solvent from the resulting protein solution. Hemoglobin's reversible oxygenation was described a few years later by Felix Hoppe-Seyler.
In 1959, Max Perutz determined the molecular structure of hemoglobin by X-ray crystallography. This work resulted in his sharing with John Kendrew the 1962 Nobel Prize in Chemistry for their studies of the structures of globular proteins.
The role of hemoglobin in the blood was elucidated by French physiologist Claude Bernard.
The name hemoglobin is derived from the words heme and globin, reflecting the fact that each subunit of hemoglobin is a globular protein with an embedded heme group. Each heme group contains one iron atom, that can bind one oxygen molecule through ion-induced dipole forces. The most common type of hemoglobin in mammals contains four such subunits.
Genetics
Hemoglobin consists of protein subunits (the "globin" molecules), and these proteins, in turn, are folded chains of a large number of different amino acids called polypeptides.
The amino acid sequence of any polypeptide created by a cell is in turn
determined by the stretches of DNA called genes. In all proteins, it is
the amino acid sequence that determines the protein's chemical
properties and function.
There is more than one hemoglobin gene: in humans, hemoglobin A
(the main form of hemoglobin present) is coded for by the genes, HBA1, HBA2, and HBB.
The amino acid sequences of the globin proteins in hemoglobins usually
differ between species. These differences grow with evolutionary
distance between species. For example, the most common hemoglobin
sequences in humans and chimpanzees are nearly identical, differing by
only one amino acid in both the alpha and the beta globin protein
chains. These differences grow larger between less closely related species.
Even within a species, different variants of hemoglobin always
exist, although one sequence is usually a "most common" one in each
species. Mutations in the genes for the hemoglobin protein in a species result in hemoglobin variants. Many of these mutant forms of hemoglobin cause no disease. Some of these mutant forms of hemoglobin, however, cause a group of hereditary diseases termed the hemoglobinopathies. The best known hemoglobinopathy is sickle-cell disease, which was the first human disease whose mechanism was understood at the molecular level. A (mostly) separate set of diseases called thalassemias involves underproduction of normal and sometimes abnormal hemoglobins, through problems and mutations in globin gene regulation. All these diseases produce anemia.
Protein
alignment of human hemoglobin proteins, alpha, beta, and delta subunits
respectively. The alignments were created using Uniprot's alignment
tool available online.
Variations in hemoglobin amino acid sequences, as with other
proteins, may be adaptive. For example, hemoglobin has been found to
adapt in different ways to high altitudes. Organisms living at high
elevations experience lower partial pressures of oxygen compared to
those at sea level. This presents a challenge to the organisms that
inhabit such environments because hemoglobin, which normally binds
oxygen at high partial pressures of oxygen, must be able to bind oxygen
when it is present at a lower pressure. Different organisms have adapted
to such a challenge. For example, recent studies have suggested genetic
variants in deer mice that help explain how deer mice that live in the
mountains are able to survive in the thin air that accompanies high
altitudes. A researcher from the University of Nebraska-Lincoln found
mutations in four different genes that can account for differences
between deer mice that live in lowland prairies versus the mountains.
After examining wild mice captured from both highlands and lowlands, it
was found that: the genes of the two breeds are "virtually
identical—except for those that govern the oxygen-carrying capacity of
their hemoglobin". "The genetic difference enables highland mice to make
more efficient use of their oxygen", since less is available at higher
altitudes, such as those in the mountains. Mammoth
hemoglobin featured mutations that allowed for oxygen delivery at lower
temperatures, thus enabling mammoths to migrate to higher latitudes
during the Pleistocene.
This was also found in hummingbirds that inhabit the Andes.
Hummingbirds already expend a lot of energy and thus have high oxygen
demands and yet Andean hummingbirds have been found to thrive in high
altitudes. Non-synonymous mutations in the hemoglobin gene of multiple
species living at high elevations (Oreotrochilus, A. castelnaudii, C. violifer, P. gigas, and A. viridicuada) have caused the protein to have less of an affinity for inositol hexaphosphate
(IHP), a molecule found in birds that has a similar role as 2,3-BPG in
humans; this results in the ability to bind oxygen in lower partial
pressures.
Birds' unique circulatory lungs also promote efficient use of oxygen at low partial pressures of O2. These two adaptations reinforce each other and account for birds' remarkable high-altitude performance.
Hemoglobin adaptation extends to humans, as well. Studies have
found that a small number of native Tibetan women have a genotype which
codes for hemoglobin to be more highly saturated with oxygen.
Natural selection seems to be the main force working on this gene
because the mortality rate of offspring is significantly lower for women
with higher hemoglobin-oxygen affinity when compared to the mortality
rate of offspring from women with low hemoglobin-oxygen affinity. While
the exact genotype and mechanism by which this occurs is not yet clear,
selection is acting on these women's ability to bind oxygen in low
partial pressures, which overall allows them to better sustain crucial
metabolic processes.
Synthesis
Hemoglobin (Hb) is synthesized in a complex series of steps. The heme part is synthesized in a series of steps in the mitochondria and the cytosol of immature red blood cells, while the globin protein parts are synthesized by ribosomes in the cytosol. Production of Hb continues in the cell throughout its early development from the proerythroblast to the reticulocyte in the bone marrow. At this point, the nucleus is lost in mammalian red blood cells, but not in birds and many other species. Even after the loss of the nucleus in mammals, residual ribosomal RNA allows further synthesis of Hb until the reticulocyte loses its RNA soon after entering the vasculature (this hemoglobin-synthetic RNA in fact gives the reticulocyte its reticulated appearance and name).
Structure
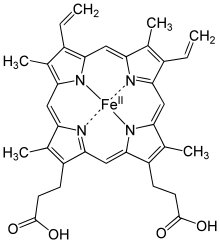
Heme b group
Hemoglobin has a quaternary structure characteristic of many multi-subunit globular proteins.
Most of the amino acids in hemoglobin form alpha helices, and these
helices are connected by short non-helical segments. Hydrogen bonds
stabilize the helical sections inside this protein, causing attractions
within the molecule, which then causes each polypeptide chain to fold
into a specific shape. Hemoglobin's quaternary structure comes from its four subunits in roughly a tetrahedral arrangement.
In most vertebrates, the hemoglobin molecule is an assembly of four globular protein subunits. Each subunit is composed of a protein chain tightly associated with a non-protein prosthetic heme group. Each protein chain arranges into a set of alpha-helix structural segments connected together in a globin fold
arrangement. Such a name is given because this arrangement is the same
folding motif used in other heme/globin proteins such as myoglobin. This folding pattern contains a pocket that strongly binds the heme group.
A heme group consists of an iron (Fe) ion (charged atom) held in a heterocyclic ring, known as a porphyrin. This porphyrin ring consists of four pyrrole molecules cyclically linked together (by methine bridges) with the iron ion bound in the center. The iron ion, which is the site of oxygen binding, coordinates with the four nitrogen
atoms in the center of the ring, which all lie in one plane. The iron
is bound strongly (covalently) to the globular protein via the N atoms
of the imidazole ring of F8 histidine residue (also known as the proximal histidine) below the porphyrin ring. A sixth position can reversibly bind oxygen by a coordinate covalent bond,
completing the octahedral group of six ligands. Oxygen binds in an
"end-on bent" geometry where one oxygen atom binds to Fe and the other
protrudes at an angle. When oxygen is not bound, a very weakly bonded
water molecule fills the site, forming a distorted octahedron.
Even though carbon dioxide is carried by hemoglobin, it does not
compete with oxygen for the iron-binding positions but is bound to the
protein chains of the structure.
The iron ion may be either in the Fe2+ or in the Fe3+ state, but ferrihemoglobin (methemoglobin) (Fe3+) cannot bind oxygen. In binding, oxygen temporarily and reversibly oxidizes (Fe2+) to (Fe3+) while oxygen temporarily turns into the superoxide ion, thus iron must exist in the +2 oxidation state to bind oxygen. If superoxide ion associated to Fe3+ is protonated, the hemoglobin iron will remain oxidized and incapable of binding oxygen. In such cases, the enzyme methemoglobin reductase will be able to eventually reactivate methemoglobin by reducing the iron center.
In adult humans, the most common hemoglobin type is a tetramer (which contains four subunit proteins) called hemoglobin A,
consisting of two α and two β subunits non-covalently bound, each made
of 141 and 146 amino acid residues, respectively. This is denoted as α2β2. The subunits are structurally similar and about the same size. Each subunit has a molecular weight of about 16,000 daltons, for a total molecular weight of the tetramer of about 64,000 daltons (64,458 g/mol). Thus, 1 g/dL = 0.1551 mmol/L. Hemoglobin A is the most intensively studied of the hemoglobin molecules.
In human infants, the hemoglobin molecule is made up of 2 α
chains and 2 γ chains. The gamma chains are gradually replaced by β
chains as the infant grows.
The four polypeptide chains are bound to each other by salt bridges, hydrogen bonds, and the hydrophobic effect.
Oxygen saturation
In
general, hemoglobin can be saturated with oxygen molecules
(oxyhemoglobin), or desaturated with oxygen molecules (deoxyhemoglobin).
Oxyhemoglobin
Oxyhemoglobin is formed during physiological respiration when oxygen binds to the heme component of the protein hemoglobin in red blood cells. This process occurs in the pulmonary capillaries adjacent to the alveoli
of the lungs. The oxygen then travels through the blood stream to be
dropped off at cells where it is utilized as a terminal electron
acceptor in the production of ATP by the process of oxidative phosphorylation. It does not, however, help to counteract a decrease in blood pH. Ventilation, or breathing, may reverse this condition by removal of carbon dioxide, thus causing a shift up in pH.
Hemoglobin exists in two forms, a taut (tense) form (T) and a relaxed form (R). Various factors such as low pH, high CO2 and high 2,3 BPG
at the level of the tissues favor the taut form, which has low oxygen
affinity and releases oxygen in the tissues. Conversely, a high pH, low
CO2, or low 2,3 BPG favors the relaxed form, which can better bind oxygen. The partial pressure of the system also affects O2
affinity where, at high partial pressures of oxygen (such as those
present in the alveoli), the relaxed (high affinity, R) state is
favored. Inversely, at low partial pressures (such as those present in
respiring tissues), the (low affinity, T) tense state is favored.
Additionally, the binding of oxygen to the iron(II) heme pulls the iron
into the plane of the porphyrin ring, causing a slight conformational
shift. The shift encourages oxygen to bind to the three remaining heme
units within hemoglobin (thus, oxygen binding is cooperative).
Deoxygenated hemoglobin
Deoxygenated hemoglobin is the form of hemoglobin without the bound oxygen. The absorption spectra of oxyhemoglobin and deoxyhemoglobin differ. The oxyhemoglobin has significantly lower absorption of the 660 nm wavelength
than deoxyhemoglobin, while at 940 nm its absorption is slightly
higher. This difference is used for the measurement of the amount of
oxygen in a patient's blood by an instrument called a pulse oximeter. This difference also accounts for the presentation of cyanosis, the blue to purplish color that tissues develop during hypoxia.
Deoxygenated hemoglobin is paramagnetic; it is weakly attracted to magnetic fields. In contrast, oxygenated hemoglobin exhibits diamagnetism, a weak repulsion from a magnetic field.
Evolution of vertebrate hemoglobin
Scientists agree that the event that separated myoglobin from hemoglobin occurred after lampreys diverged from jawed vertebrates.
This separation of myoglobin and hemoglobin allowed for the different
functions of the two molecules to arise and develop: myoglobin has more
to do with oxygen storage while hemoglobin is tasked with oxygen
transport. The α- and β-like globin genes encode the individual subunits of the protein.
The predecessors of these genes arose through another duplication event
also after the gnathosome common ancestor derived from jawless fish,
approximately 450–500 million years ago.
The development of α and β genes created the potential for hemoglobin
to be composed of multiple subunits, a physical composition central to
hemoglobin's ability to transport oxygen. Having multiple subunits
contributes to hemoglobin's ability to bind oxygen cooperatively as well
as be regulated allosterically. Subsequently, the α gene also underwent a duplication event to form the HBA1 and HBA2 genes.
These further duplications and divergences have created a diverse range
of α- and β-like globin genes that are regulated so that certain forms
occur at different stages of development.
Most ice fish of the family Channichthyidae have lost their hemoglobin genes as an adaptation to cold water.
Iron's oxidation state in oxyhemoglobin
Assigning oxygenated hemoglobin's oxidation state is difficult because oxyhemoglobin (Hb-O2),
by experimental measurement, is diamagnetic (no net unpaired
electrons), yet the lowest-energy (ground-state) electron configurations
in both oxygen and iron are paramagnetic
(suggesting at least one unpaired electron in the complex). The
lowest-energy form of oxygen, and the lowest energy forms of the
relevant oxidation states of iron, are these:
- Triplet oxygen, the lowest-energy molecular oxygen species, has two unpaired electrons in antibonding π* molecular orbitals.
- Iron(II) tends to exist in a high-spin 3d6 configuration with four unpaired electrons.
- Iron(III) (3d5) has an odd number of electrons, and thus must have one or more unpaired electrons, in any energy state.
All of these structures are paramagnetic (have unpaired electrons),
not diamagnetic. Thus, a non-intuitive (e.g., a higher-energy for at
least one species) distribution of electrons in the combination of iron
and oxygen must exist, in order to explain the observed diamagnetism and
no unpaired electrons.
The two logical possibilities to produce diamagnetic (no net spin) Hb-O2 are:
- Low-spin Fe2+ binds to singlet oxygen. Both low-spin iron and singlet oxygen are diamagnetic. However, the singlet form of oxygen is the higher-energy form of the molecule.
- Low-spin Fe2+ binds to O2•− (the superoxide ion) and the two unpaired electrons couple antiferromagnetically, giving observed diamagnetic properties. Here, the iron has been oxidized (has lost one electron), and the oxygen has been reduced (has gained one electron).
Another possible model in which low-spin Fe4+ binds to peroxide, O22−,
can be ruled out by itself, because the iron is paramagnetic (although
the peroxide ion is diamagnetic). Here, the iron has been oxidized by
two electrons, and the oxygen reduced by two electrons.
Direct experimental data:
- X-ray photoelectron spectroscopy suggests iron has an oxidation state of approximately 3.2.
- Infrared vibrational frequencies of the O-O bond suggests a bond length fitting with superoxide (a bond order of about 1.6, with superoxide being 1.5).
- X-ray Absorption Near Edge Structures at the iron K-edge. The energy shift of 5 eV between deoxyhemoglobin and oxyhemoglobin, as for all the methemoglobin species, strongly suggests an actual local charge closer to Fe3+ than Fe2+.
Thus, the nearest formal oxidation state of iron in Hb-O2 is the +3 state, with oxygen in the −1 state (as superoxide .O2−).
The diamagnetism in this configuration arises from the single unpaired
electron on superoxide aligning antiferromagnetically with the single
unpaired electron on iron (in a low-spin d5 state), to give no net spin to the entire configuration, in accordance with diamagnetic oxyhemoglobin from experiment.
The second choice of the logical possibilities above for
diamagnetic oxyhemoglobin being found correct by experiment, is not
surprising: singlet oxygen (possibility #1) is an unrealistically high
energy state. Model 3 leads to unfavorable separation of charge (and
does not agree with the magnetic data), although it could make a minor
contribution as a resonance form. Iron's shift to a higher oxidation state in Hb-O2
decreases the atom's size, and allows it into the plane of the
porphyrin ring, pulling on the coordinated histidine residue and
initiating the allosteric changes seen in the globulins.
Early postulates by bio-inorganic chemists claimed that
possibility #1 (above) was correct and that iron should exist in
oxidation state II. This conclusion seemed likely, since the iron
oxidation state III as methemoglobin, when not accompanied by superoxide .O2− to "hold" the oxidation electron, was known to render hemoglobin incapable of binding normal triplet O2
as it occurs in the air. It was thus assumed that iron remained as
Fe(II) when oxygen gas was bound in the lungs. The iron chemistry in
this previous classical model was elegant, but the required presence of
the diamagnetic, high-energy, singlet oxygen molecule was never
explained. It was classically argued that the binding of an oxygen
molecule placed high-spin iron(II) in an octahedral field of
strong-field ligands; this change in field would increase the crystal field splitting energy,
causing iron's electrons to pair into the low-spin configuration, which
would be diamagnetic in Fe(II). This forced low-spin pairing is indeed
thought to happen in iron when oxygen binds, but is not enough to
explain iron's change in size. Extraction of an additional electron from
iron by oxygen is required to explain both iron's smaller size and
observed increased oxidation state, and oxygen's weaker bond.
The assignment of a whole-number oxidation state is a formalism,
as the covalent bonds are not required to have perfect bond orders
involving whole electron transfer. Thus, all three models for
paramagnetic Hb-O2 may contribute to some small degree (by resonance) to the actual electronic configuration of Hb-O2. However, the model of iron in Hb-O2 being Fe(II) is more correct than the classical idea that it remains Fe(II).
Cooperativity
A schematic visual model of oxygen-binding process, showing all four monomers and hemes, and protein chains only as diagrammatic coils, to facilitate visualization into the molecule. Oxygen is not shown in this model, but, for each of the iron atoms, it binds to the iron (red sphere) in the flat heme.
For example, in the upper-left of the four hemes shown, oxygen binds at
the left of the iron atom shown in the upper-left of diagram. This
causes the iron atom to move backward into the heme that holds it (the
iron moves upward as it binds oxygen, in this illustration), tugging the
histidine
residue (modeled as a red pentagon on the right of the iron) closer, as
it does. This, in turn, pulls on the protein chain holding the histidine.
When oxygen binds to the iron complex, it causes the iron atom to move back toward the center of the plane of the porphyrin ring (see moving diagram). At the same time, the imidazole
side-chain of the histidine residue interacting at the other pole of
the iron is pulled toward the porphyrin ring. This interaction forces
the plane of the ring sideways toward the outside of the tetramer, and
also induces a strain in the protein helix containing the histidine as
it moves nearer to the iron atom. This strain is transmitted to the
remaining three monomers in the tetramer, where it induces a similar
conformational change in the other heme sites such that binding of
oxygen to these sites becomes easier.
As oxygen binds to one monomer of hemoglobin, the tetramer's
conformation shifts from the T (tense) state to the R (relaxed) state.
This shift promotes the binding of oxygen to the remaining three
monomer's heme groups, thus saturating the hemoglobin molecule with
oxygen.
In the tetrameric form of normal adult hemoglobin, the binding of oxygen is, thus, a cooperative process.
The binding affinity of hemoglobin for oxygen is increased by the
oxygen saturation of the molecule, with the first molecules of oxygen
bound influencing the shape of the binding sites for the next ones, in a
way favorable for binding. This positive cooperative binding is
achieved through steric
conformational changes of the hemoglobin protein complex as discussed
above; i.e., when one subunit protein in hemoglobin becomes oxygenated, a
conformational or structural change in the whole complex is initiated,
causing the other subunits to gain an increased affinity for oxygen. As a
consequence, the oxygen binding curve of hemoglobin is sigmoidal, or S-shaped, as opposed to the normal hyperbolic curve associated with noncooperative binding.
The dynamic mechanism of the cooperativity in hemoglobin and its relation with the low-frequency resonance has been discussed.
Binding for ligands other than oxygen
Besides the oxygen ligand, which binds to hemoglobin in a cooperative manner, hemoglobin ligands also include competitive inhibitors such as carbon monoxide (CO) and allosteric ligands such as carbon dioxide (CO2) and nitric oxide (NO). The carbon dioxide is bound to amino groups of the globin proteins to form carbaminohemoglobin; this mechanism is thought to account for about 10% of carbon dioxide transport in mammals. Nitric oxide can also be transported by hemoglobin; it is bound to specific thiol
groups in the globin protein to form an S-nitrosothiol, which
dissociates into free nitric oxide and thiol again, as the hemoglobin
releases oxygen from its heme site. This nitric oxide transport to
peripheral tissues is hypothesized to assist oxygen transport in
tissues, by releasing vasodilatory nitric oxide to tissues in which oxygen levels are low.
Competitive
The binding of oxygen is affected by molecules such as carbon monoxide (for example, from tobacco smoking, exhaust gas,
and incomplete combustion in furnaces). CO competes with oxygen at the
heme binding site. Hemoglobin's binding affinity for CO is 250 times
greater than its affinity for oxygen,
meaning that small amounts of CO dramatically reduce hemoglobin's
ability to transport oxygen. Since carbon monoxide is a colorless,
odorless and tasteless gas, and poses a potentially fatal threat, carbon monoxide detectors
have become commercially available to warn of dangerous levels in
residences. When hemoglobin combines with CO, it forms a very bright red
compound called carboxyhemoglobin, which may cause the skin of CO poisoning
victims to appear pink in death, instead of white or blue. When
inspired air contains CO levels as low as 0.02%, headache and nausea
occur; if the CO concentration is increased to 0.1%, unconsciousness
will follow. In heavy smokers, up to 20% of the oxygen-active sites can
be blocked by CO.
In similar fashion, hemoglobin also has competitive binding affinity for cyanide (CN−), sulfur monoxide (SO), and sulfide (S2−), including hydrogen sulfide (H2S).
All of these bind to iron in heme without changing its oxidation state,
but they nevertheless inhibit oxygen-binding, causing grave toxicity.
The iron atom in the heme group must initially be in the ferrous (Fe2+)
oxidation state to support oxygen and other gases' binding and
transport (it temporarily switches to ferric during the time oxygen is
bound, as explained above). Initial oxidation to the ferric (Fe3+) state without oxygen converts hemoglobin into "hemiglobin" or methemoglobin,
which cannot bind oxygen. Hemoglobin in normal red blood cells is
protected by a reduction system to keep this from happening. Nitric
oxide is capable of converting a small fraction of hemoglobin to
methemoglobin in red blood cells. The latter reaction is a remnant
activity of the more ancient nitric oxide dioxygenase function of globins.
Allosteric
Carbon dioxide occupies a different binding site on the
hemoglobin. Carbon dioxide is more readily dissolved in deoxygenated
blood, facilitating its removal from the body after the oxygen has been
released to tissues undergoing metabolism. This increased affinity for
carbon dioxide by the venous blood is known as the Haldane effect. Through the enzyme carbonic anhydrase, carbon dioxide reacts with water to give carbonic acid, which decomposes into bicarbonate and protons:
- CO2 + H2O → H2CO3 → HCO3− + H+
The sigmoidal shape of hemoglobin's oxygen-dissociation curve results from cooperative binding of oxygen to hemoglobin.
Hence, blood with high carbon dioxide levels is also lower in pH (more acidic).
Hemoglobin can bind protons and carbon dioxide, which causes a
conformational change in the protein and facilitates the release of
oxygen. Protons bind at various places on the protein, while carbon
dioxide binds at the α-amino group. Carbon dioxide binds to hemoglobin and forms carbaminohemoglobin. This decrease in hemoglobin's affinity for oxygen by the binding of carbon dioxide and acid is known as the Bohr effect. The Bohr effect favors the T state rather than the R state. (shifts the O2-saturation curve to the right).
Conversely, when the carbon dioxide levels in the blood decrease (i.e.,
in the lung capillaries), carbon dioxide and protons are released from
hemoglobin, increasing the oxygen affinity of the protein. A reduction
in the total binding capacity of hemoglobin to oxygen (i.e. shifting the
curve down, not just to the right) due to reduced pH is called the root effect. This is seen in bony fish.
It is necessary for hemoglobin to release the oxygen that it
binds; if not, there is no point in binding it. The sigmoidal curve of
hemoglobin makes it efficient in binding (taking up O2 in lungs), and efficient in unloading (unloading O2 in tissues).
In people acclimated to high altitudes, the concentration of 2,3-Bisphosphoglycerate
(2,3-BPG) in the blood is increased, which allows these individuals to
deliver a larger amount of oxygen to tissues under conditions of lower oxygen tension. This phenomenon, where molecule Y affects the binding of molecule X to a transport molecule Z, is called a heterotropic
allosteric effect. Hemoglobin in organisms at high altitudes has also
adapted such that it has less of an affinity for 2,3-BPG and so the
protein will be shifted more towards its R state. In its R state,
hemoglobin will bind oxygen more readily, thus allowing organisms to
perform the necessary metabolic processes when oxygen is present at low
partial pressures.
Animals other than humans use different molecules to bind to hemoglobin and change its O2 affinity under unfavorable conditions. Fish use both ATP and GTP.
These bind to a phosphate "pocket" on the fish hemoglobin molecule,
which stabilizes the tense state and therefore decreases oxygen
affinity. GTP reduces hemoglobin oxygen affinity much more than ATP, which is thought to be due to an extra hydrogen bond formed that further stabilizes the tense state. Under hypoxic conditions, the concentration of both ATP and GTP is reduced in fish red blood cells to increase oxygen affinity.
A variant hemoglobin, called fetal hemoglobin (HbF, α2γ2), is found in the developing fetus,
and binds oxygen with greater affinity than adult hemoglobin. This
means that the oxygen binding curve for fetal hemoglobin is left-shifted
(i.e., a higher percentage of hemoglobin has oxygen bound to it at
lower oxygen tension), in comparison to that of adult hemoglobin. As a
result, fetal blood in the placenta is able to take oxygen from maternal blood.
Hemoglobin also carries nitric oxide
(NO) in the globin part of the molecule. This improves oxygen delivery
in the periphery and contributes to the control of respiration. NO binds
reversibly to a specific cysteine residue in globin; the binding
depends on the state (R or T) of the hemoglobin. The resulting
S-nitrosylated hemoglobin influences various NO-related activities such
as the control of vascular resistance, blood pressure and respiration.
NO is not released in the cytoplasm of red blood cells but transported
out of them by an anion exchanger called AE1.
Types in humans
Hemoglobin variants are a part of the normal embryonic and fetal development. They may also be pathologic mutant forms of hemoglobin in a population, caused by variations in genetics. Some well-known hemoglobin variants, such as sickle-cell anemia, are responsible for diseases and are considered hemoglobinopathies. Other variants cause no detectable pathology, and are thus considered non-pathological variants.
In the embryo:
- Gower 1 (ζ2ε2)
- Gower 2 (α2ε2) (PDB: 1A9W)
- Hemoglobin Portland I (ζ2γ2)
- Hemoglobin Portland II (ζ2β2).
In the fetus:
- Hemoglobin F (α2γ2) (PDB: 1FDH).
After birth:
- Hemoglobin A (α2β2) (PDB: 1BZ0) – The most common with a normal amount over 95%
- Hemoglobin A2 (α2δ2) – δ chain synthesis begins late in the third trimester and, in adults, it has a normal range of 1.5–3.5%
- Hemoglobin F (α2γ2) – In adults Hemoglobin F is restricted to a limited population of red cells called F-cells. However, the level of Hb F can be elevated in persons with sickle-cell disease and beta-thalassemia.
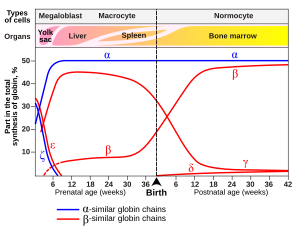
Gene
expression of hemoglobin before and after birth. Also identifies the
types of cells and organs in which the gene expression (data on Wood W.G., (1976). Br. Med. Bull. 32, 282.)
Variant forms that cause disease:
- Hemoglobin D-Punjab – (α2βD2) – A variant form of hemoglobin.
- Hemoglobin H (β4) – A variant form of hemoglobin, formed by a tetramer of β chains, which may be present in variants of α thalassemia.
- Hemoglobin Barts (γ4) – A variant form of hemoglobin, formed by a tetramer of γ chains, which may be present in variants of α thalassemia.
- Hemoglobin S (α2βS2) – A variant form of hemoglobin found in people with sickle cell disease. There is a variation in the β-chain gene, causing a change in the properties of hemoglobin, which results in sickling of red blood cells.
- Hemoglobin C (α2βC2) – Another variant due to a variation in the β-chain gene. This variant causes a mild chronic hemolytic anemia.
- Hemoglobin E (α2βE2) – Another variant due to a variation in the β-chain gene. This variant causes a mild chronic hemolytic anemia.
- Hemoglobin AS – A heterozygous form causing sickle cell trait with one adult gene and one sickle cell disease gene
- Hemoglobin SC disease – A compound heterozygous form with one sickle gene and another encoding Hemoglobin C.
- Hemoglobin Hopkins-2 - A variant form of hemoglobin that is sometimes viewed in combination with Hemoglobin S to produce sickle cell disease.
Degradation in vertebrate animals
When red blood cells
reach the end of their life due to aging or defects, they are removed
from the circulation by the phagocytic activity of macrophages in the
spleen or the liver or hemolyze within the circulation. Free hemoglobin
is then cleared from the circulation via the hemoglobin transporter CD163,
which is exclusively expressed on monocytes or macrophages. Within
these cells the hemoglobin molecule is broken up, and the iron gets
recycled. This process also produces one molecule of carbon monoxide for
every molecule of heme degraded.
Heme degradation is one of the few natural sources of carbon monoxide
in the human body, and is responsible for the normal blood levels of
carbon monoxide even in people breathing pure air. The other major final
product of heme degradation is bilirubin.
Increased levels of this chemical are detected in the blood if red
blood cells are being destroyed more rapidly than usual. Improperly
degraded hemoglobin protein or hemoglobin that has been released from
the blood cells too rapidly can clog small blood vessels, especially the
delicate blood filtering vessels of the kidneys, causing kidney damage.
Iron is removed from heme and salvaged for later use, it is stored as hemosiderin or ferritin in tissues and transported in plasma by beta globulins as transferrins.
When the porphyrin ring is broken up, the fragments are normally
secreted as a yellow pigment called bilirubin, which is secreted into
the intestines as bile. Intestines metabolise bilirubin into
urobilinogen. Urobilinogen leaves the body in feces, in a pigment
called stercobilin. Globulin is metabolized into amino acids that are
then released into circulation.
Role in disease
Hemoglobin deficiency can be caused either by a decreased amount of hemoglobin molecules, as in anemia, or by decreased ability of each molecule to bind oxygen at the same partial pressure of oxygen. Hemoglobinopathies (genetic defects resulting in abnormal structure of the hemoglobin molecule) may cause both. In any case, hemoglobin deficiency decreases blood oxygen-carrying capacity. Hemoglobin deficiency is, in general, strictly distinguished from hypoxemia, defined as decreased partial pressure of oxygen in blood, although both are causes of hypoxia (insufficient oxygen supply to tissues).
Other common causes of low hemoglobin include loss of blood,
nutritional deficiency, bone marrow problems, chemotherapy, kidney
failure, or abnormal hemoglobin (such as that of sickle-cell disease).
The ability of each hemoglobin molecule to carry oxygen is normally modified by altered blood pH or CO2, causing an altered oxygen–hemoglobin dissociation curve. However, it can also be pathologically altered in, e.g., carbon monoxide poisoning.
Decrease of hemoglobin, with or without an absolute decrease of
red blood cells, leads to symptoms of anemia. Anemia has many different
causes, although iron deficiency and its resultant iron deficiency anemia
are the most common causes in the Western world. As absence of iron
decreases heme synthesis, red blood cells in iron deficiency anemia are hypochromic (lacking the red hemoglobin pigment) and microcytic (smaller than normal). Other anemias are rarer. In hemolysis (accelerated breakdown of red blood cells), associated jaundice is caused by the hemoglobin metabolite bilirubin, and the circulating hemoglobin can cause renal failure.
Some mutations in the globin chain are associated with the hemoglobinopathies, such as sickle-cell disease and thalassemia. Other mutations, as discussed at the beginning of the article, are benign and are referred to merely as hemoglobin variants.
There is a group of genetic disorders, known as the porphyrias that are characterized by errors in metabolic pathways of heme synthesis. King George III of the United Kingdom was probably the most famous porphyria sufferer.
To a small extent, hemoglobin A slowly combines with glucose at the terminal valine (an alpha aminoacid) of each β chain. The resulting molecule is often referred to as Hb A1c, a glycosylated hemoglobin.
The binding of glucose to amino acids in the hemoglobin takes place
spontaneously (without the help of an enzyme) in many proteins, and is
not known to serve a useful purpose. However, as the concentration of
glucose in the blood increases, the percentage of Hb A that turns into
Hb A1c increases. In diabetics whose glucose usually runs high, the percent Hb A1c also runs high. Because of the slow rate of Hb A combination with glucose, the Hb A1c percentage reflects a weighted average of blood glucose levels over the lifetime of red cells, which is approximately 120 days.
The levels of glycosylated hemoglobin are therefore measured in order
to monitor the long-term control of the chronic disease of type 2
diabetes mellitus (T2DM). Poor control of T2DM results in high levels of
glycosylated hemoglobin in the red blood cells. The normal reference
range is approximately 4.0–5.9%. Though difficult to obtain, values less
than 7% are recommended for people with T2DM. Levels greater than 9%
are associated with poor control of the glycosylated hemoglobin, and
levels greater than 12% are associated with very poor control. Diabetics
who keep their glycosylated hemoglobin levels close to 7% have a much
better chance of avoiding the complications that may accompany diabetes
(than those whose levels are 8% or higher).
In addition, increased glycosylation of hemoglobin increases its
affinity for oxygen, therefore preventing its release at the tissue and
inducing a level of hypoxia in extreme cases.
Elevated levels of hemoglobin are associated with increased numbers or sizes of red blood cells, called polycythemia. This elevation may be caused by congenital heart disease, cor pulmonale, pulmonary fibrosis, too much erythropoietin, or polycythemia vera.
High hemoglobin levels may also be caused by exposure to high
altitudes, smoking, dehydration (artificially by concentrating Hb),
advanced lung disease and certain tumors.
A recent study done in Pondicherry, India, shows its importance in coronary artery disease.
Diagnostic uses
A hemoglobin concentration measurement being administered before a blood donation at the American Red Cross Boston Blood Donation Center.
Hemoglobin concentration measurement is among the most commonly performed blood tests, usually as part of a complete blood count. For example, it is typically tested before or after blood donation. Results are reported in g/L, g/dL or mol/L.
1 g/dL equals about 0.6206 mmol/L, although the latter units are not
used as often due to uncertainty regarding the polymeric state of the
molecule. This conversion factor, using the single globin unit molecular weight of 16,000 Da,
is more common for hemoglobin concentration in blood. For MCHC (mean
corpuscular hemoglobin concentration) the conversion factor 0.155, which
uses the tetramer weight of 64,500 Da, is more common. Normal levels are:
- Men: 13.8 to 18.0 g/dL (138 to 180 g/L, or 8.56 to 11.17 mmol/L)
- Women: 12.1 to 15.1 g/dL (121 to 151 g/L, or 7.51 to 9.37 mmol/L)
- Children: 11 to 16 g/dL (110 to 160 g/L, or 6.83 to 9.93 mmol/L)
- Pregnant women: 11 to 14 g/dL (110 to 140 g/L, or 6.83 to 8.69 mmol/L) (9.5 to 15 usual value during pregnancy)
Normal values of hemoglobin in the 1st and 3rd trimesters of pregnant
women must be at least 11 g/dL and at least 10.5 g/dL during the 2nd
trimester.
Dehydration or hyperhydration can greatly influence measured hemoglobin levels. Albumin can indicate hydration status.
If the concentration is below normal, this is called anemia.
Anemias are classified by the size of red blood cells, the cells that
contain hemoglobin in vertebrates. The anemia is called "microcytic" if
red cells are small, "macrocytic" if they are large, and "normocytic"
otherwise.
Hematocrit,
the proportion of blood volume occupied by red blood cells, is
typically about three times the hemoglobin concentration measured in
g/dL. For example, if the hemoglobin is measured at 17 g/dL, that
compares with a hematocrit of 51%.
Laboratory hemoglobin test methods require a blood sample
(arterial, venous, or capillary) and analysis on hematology analyzer and
CO-oximeter. Additionally, a new noninvasive hemoglobin (SpHb) test
method called Pulse CO-Oximetry is also available with comparable
accuracy to invasive methods.
Concentrations of oxy- and deoxyhemoglobin can be measured continuously, regionally and noninvasively using NIRS.
NIRS can be used both on the head and on muscles. This technique is
often used for research in e.g. elite sports training, ergonomics,
rehabilitation, patient monitoring, neonatal research, functional brain
monitoring, brain computer interface, urology (bladder contraction),
neurology (Neurovascular coupling) and more.
Long-term control of blood sugar concentration can be measured by the concentration of Hb A1c. Measuring it directly would require many samples because blood sugar levels vary widely through the day. Hb A1c is the product of the irreversible reaction of hemoglobin A with glucose. A higher glucose concentration results in more Hb A1c. Because the reaction is slow, the Hb A1c proportion represents glucose level in blood averaged over the half-life of red blood cells, is typically 50–55 days. An Hb A1c
proportion of 6.0% or less show good long-term glucose control, while
values above 7.0% are elevated. This test is especially useful for
diabetics.
The functional magnetic resonance imaging
(fMRI) machine uses the signal from deoxyhemoglobin, which is sensitive
to magnetic fields since it is paramagnetic. Combined measurement with NIRS shows good correlation with both the oxy- and deoxyhemoglobin signal compared to the BOLD signal.
Athletic tracking and self tracking uses
Hemoglobin
can be tracked noninvasively, to build an individual data set tracking
the hemoconcentration and hemodilution effects of daily activities for
better understanding of sports performance and training. Athletes are
often concerned about endurance and intensity of exercise. The sensor
uses light-emitting diodes that emit red and infrared light through the
tissue to a light detector, which then sends a signal to a processor to
calculate the absorption of light by the hemoglobin protein.
This sensor is similar to a pulse oximeter, which consists of a small sensing device that clips to the finger.
Analogues in non-vertebrate organisms
A
variety of oxygen-transport and -binding proteins exist in organisms
throughout the animal and plant kingdoms. Organisms including bacteria, protozoans, and fungi all have hemoglobin-like proteins whose known and predicted roles include the reversible binding of gaseous ligands. Since many of these proteins contain globins and the heme moiety
(iron in a flat porphyrin support), they are often called hemoglobins,
even if their overall tertiary structure is very different from that of
vertebrate hemoglobin. In particular, the distinction of "myoglobin" and
hemoglobin in lower animals is often impossible, because some of these
organisms do not contain muscles. Or, they may have a recognizable separate circulatory system but not one that deals with oxygen transport (for example, many insects and other arthropods).
In all these groups, heme/globin-containing molecules (even monomeric
globin ones) that deal with gas-binding are referred to as
oxyhemoglobins. In addition to dealing with transport and sensing of
oxygen, they may also deal with NO, CO2, sulfide compounds, and even O2 scavenging in environments that must be anaerobic.
They may even deal with detoxification of chlorinated materials in a
way analogous to heme-containing P450 enzymes and peroxidases.
The giant tube worm Riftia pachyptila showing red hemoglobin-containing plumes
The structure of hemoglobins varies across species. Hemoglobin occurs
in all kingdoms of organisms, but not in all organisms. Primitive
species such as bacteria, protozoa, algae, and plants often have single-globin hemoglobins. Many nematode worms, molluscs, and crustaceans contain very large multisubunit molecules, much larger than those in vertebrates. In particular, chimeric hemoglobins found in fungi and giant annelids may contain both globin and other types of proteins.
One of the most striking occurrences and uses of hemoglobin in organisms is in the giant tube worm (Riftia pachyptila, also called Vestimentifera), which can reach 2.4 meters length and populates ocean volcanic vents. Instead of a digestive tract, these worms contain a population of bacteria constituting half the organism's weight. The bacteria react with H2S from the vent and O2 from the water to produce energy to make food from H2O and CO2. The worms end with a deep-red fan-like structure ("plume"), which extends into the water and absorbs H2S and O2 for the bacteria, and CO2
for use as synthetic raw material similar to photosynthetic plants. The
structures are bright-red due to their containing several
extraordinarily complex hemoglobins that have up to 144 globin chains,
each including associated heme structures. These hemoglobins are
remarkable for being able to carry oxygen in the presence of sulfide,
and even to carry sulfide, without being completely "poisoned" or
inhibited by it as hemoglobins in most other species are.
Other oxygen-binding proteins
- Myoglobin
- Found in the muscle tissue of many vertebrates, including humans, it gives muscle tissue a distinct red or dark gray color. It is very similar to hemoglobin in structure and sequence, but is not a tetramer; instead, it is a monomer that lacks cooperative binding. It is used to store oxygen rather than transport it.
- Hemocyanin
- The second most common oxygen-transporting protein found in nature, it is found in the blood of many arthropods and molluscs. Uses copper prosthetic groups instead of iron heme groups and is blue in color when oxygenated.
- Hemerythrin
- Some marine invertebrates and a few species of annelid use this iron-containing non-heme protein to carry oxygen in their blood. Appears pink/violet when oxygenated, clear when not.
- Chlorocruorin
- Found in many annelids, it is very similar to erythrocruorin, but the heme group is significantly different in structure. Appears green when deoxygenated and red when oxygenated.
- Vanabins
- Also known as vanadium chromagens, they are found in the blood of sea squirts. They were once hypothesized to use the rare metal vanadium as an oxygen binding prosthetic group. However, although they do contain vanadium by preference, they apparently bind little oxygen, and thus have some other function, which has not been elucidated (sea squirts also contain some hemoglobin). They may act as toxins.
- Erythrocruorin
- Found in many annelids, including earthworms, it is a giant free-floating blood protein containing many dozens—possibly hundreds—of iron- and heme-bearing protein subunits bound together into a single protein complex with a molecular mass greater than 3.5 million daltons.
- Pinnaglobin
- Only seen in the mollusc Pinna nobilis. Brown manganese-based porphyrin protein.
- Leghemoglobin
- In leguminous plants, such as alfalfa or soybeans, the nitrogen fixing bacteria in the roots are protected from oxygen by this iron heme containing oxygen-binding protein. The specific enzyme protected is nitrogenase, which is unable to reduce nitrogen gas in the presence of free oxygen.
- Coboglobin
- A synthetic cobalt-based porphyrin. Coboprotein would appear colorless when oxygenated, but yellow when in veins.
Presence in nonerythroid cells
Some nonerythroid cells (i.e., cells other than the red blood cell line) contain hemoglobin. In the brain, these include the A9 dopaminergic neurons in the substantia nigra, astrocytes in the cerebral cortex and hippocampus, and in all mature oligodendrocytes.
It has been suggested that brain hemoglobin in these cells may enable
the "storage of oxygen to provide a homeostatic mechanism in anoxic
conditions, which is especially important for A9 DA neurons that have an
elevated metabolism with a high requirement for energy production". It has been noted further that "A9 dopaminergic
neurons may be at particular risk since in addition to their high
mitochondrial activity they are under intense oxidative stress caused by
the production of hydrogen peroxide via autoxidation and/or monoamine
oxidase (MAO)-mediated deamination of dopamine and the subsequent
reaction of accessible ferrous iron to generate highly toxic hydroxyl
radicals". This may explain the risk of these cells for degeneration in Parkinson's disease.
The hemoglobin-derived iron in these cells is not the cause of the
post-mortem darkness of these cells (origin of the Latin name,
substantia nigra), but rather is due to neuromelanin.
Outside the brain, hemoglobin has non-oxygen-carrying functions as an antioxidant and a regulator of iron metabolism in macrophages, alveolar cells, and mesangial cells in the kidney.
In history, art and music
Heart of Steel (Hemoglobin) (2005) by Julian Voss-Andreae.
The images show the 5-foot (1.60 m) tall sculpture right after
installation, after 10 days, and after several months of exposure to the
elements.
Historically, an association between the color of blood and rust occurs in the association of the planet Mars,
with the Roman god of war, since the planet is an orange-red, which
reminded the ancients of blood. Although the color of the planet is due
to iron compounds in combination with oxygen in the Martian soil, it is a
common misconception that the iron in hemoglobin and its oxides gives
blood its red color. The color is actually due to the porphyrin moiety of hemoglobin to which the iron is bound, not the iron itself,
although the ligation and redox state of the iron can influence the pi
to pi* or n to pi* electronic transitions of the porphyrin and hence its
optical characteristics.
Artist Julian Voss-Andreae created a sculpture called "Heart of Steel (Hemoglobin)" in 2005, based on the protein's backbone. The sculpture was made from glass and weathering steel.
The intentional rusting of the initially shiny work of art mirrors
hemoglobin's fundamental chemical reaction of oxygen binding to iron.
Montreal artist Nicolas Baier created Lustre (Hémoglobine), a
sculpture in stainless steel that shows the structure of the hemoglobin
molecule. It is displayed in the atrium of McGill University Health Centre's research centre in Montreal. The sculpture measures about 10 meeres × 10 meters × 10 meters.