From Wikipedia, the free encyclopedia
Preterm birth, also known as premature birth, is the birth of a baby at fewer than 37 weeks' gestational age. These babies are known as preemies or premies. Symptoms of preterm labor include uterine contractions which occur more often than every ten minutes or the leaking of fluid from the vagina. Premature infants are at greater risk for cerebral palsy, delays in development, hearing problems and sight problems. These risks are greater the earlier a baby is born.
The cause of preterm birth is often not known. Risk factors include diabetes, high blood pressure, being pregnant with more than one baby, being either obese or underweight, a number of vaginal infections, tobacco smoking and psychological stress, among others. It is recommended that labor not be medically induced before 39 weeks unless required for other medical reasons. The same recommendation applies to cesarean section. Medical reasons for early delivery include preeclampsia.
In those at risk, the hormone progesterone, if taken during pregnancy, may prevent preterm birth. Evidence does not support the usefulness of bed rest. It is estimated that at least 75% of preterm infants would survive with appropriate treatment, and the survival rate is highest among the infants born the latest. In women who might deliver between 24 and 37 weeks, corticosteroids improve outcomes. A number of medications, including nifedipine, may delay delivery so that a mother can be moved to where more medical care is available and the corticosteroids have a greater chance to work. Once the baby is born, care includes keeping the baby warm through skin to skin contact, supporting breastfeeding, treating infections and supporting breathing.
Preterm birth is the most common cause of death among infants worldwide. About 15 million babies are preterm each year (5% to 18% of all deliveries). Approximately 0.5% of births are extremely early periviable births, and these account for most of the deaths. In many countries, rates of premature births have increased between the 1990s and 2010s. Complications from preterm births resulted in 0.81 million deaths in 2015 down from 1.57 million in 1990. The chance of survival at 22 weeks is about 6%, while at 23 weeks it is 26%, 24 weeks 55% and 25 weeks about 72%. The chances of survival without any long-term difficulties are lower.
| Preterm birth | |
|---|---|
| Other names | Premature birth, preemies, premmies |
 | |
| Intubated preterm baby in an incubator | |
| Specialty | Obstetrics, pediatrics |
| Symptoms | Birth of a baby at younger than 37 weeks' gestational age |
| Complications | Cerebral palsy, delays in development, hearing problems, sight problems |
| Causes | Often unknown |
| Risk factors | Diabetes, high blood pressure, being pregnant with more than one baby, obesity or underweight, a number of vaginal infections, celiac disease, tobacco smoking, psychological stress |
| Prevention | Progesterone |
| Treatment | Corticosteroids, keeping the baby warm through skin to skin contact, supporting breastfeeding, treating infections, supporting breathing |
| Frequency | ~15 million a year (12% of deliveries) |
| Deaths | 805,800 |
Preterm birth, also known as premature birth, is the birth of a baby at fewer than 37 weeks' gestational age. These babies are known as preemies or premies. Symptoms of preterm labor include uterine contractions which occur more often than every ten minutes or the leaking of fluid from the vagina. Premature infants are at greater risk for cerebral palsy, delays in development, hearing problems and sight problems. These risks are greater the earlier a baby is born.
The cause of preterm birth is often not known. Risk factors include diabetes, high blood pressure, being pregnant with more than one baby, being either obese or underweight, a number of vaginal infections, tobacco smoking and psychological stress, among others. It is recommended that labor not be medically induced before 39 weeks unless required for other medical reasons. The same recommendation applies to cesarean section. Medical reasons for early delivery include preeclampsia.
In those at risk, the hormone progesterone, if taken during pregnancy, may prevent preterm birth. Evidence does not support the usefulness of bed rest. It is estimated that at least 75% of preterm infants would survive with appropriate treatment, and the survival rate is highest among the infants born the latest. In women who might deliver between 24 and 37 weeks, corticosteroids improve outcomes. A number of medications, including nifedipine, may delay delivery so that a mother can be moved to where more medical care is available and the corticosteroids have a greater chance to work. Once the baby is born, care includes keeping the baby warm through skin to skin contact, supporting breastfeeding, treating infections and supporting breathing.
Preterm birth is the most common cause of death among infants worldwide. About 15 million babies are preterm each year (5% to 18% of all deliveries). Approximately 0.5% of births are extremely early periviable births, and these account for most of the deaths. In many countries, rates of premature births have increased between the 1990s and 2010s. Complications from preterm births resulted in 0.81 million deaths in 2015 down from 1.57 million in 1990. The chance of survival at 22 weeks is about 6%, while at 23 weeks it is 26%, 24 weeks 55% and 25 weeks about 72%. The chances of survival without any long-term difficulties are lower.
Signs and symptoms
A new mother holds her premature baby at Kapiolani Medical Center NICU in Honolulu, Hawaii
Preterm birth causes a range of problems.
The main categories of causes of preterm birth are preterm labor induction and spontaneous preterm labor. Signs and symptoms of preterm labor include four or more uterine contractions in one hour. In contrast to false labour, true labor is accompanied by cervical dilatation and effacement.
Also, vaginal bleeding in the third trimester, heavy pressure in the
pelvis, or abdominal or back pain could be indicators that a preterm
birth is about to occur. A watery discharge from the vagina may indicate
premature rupture of the membranes that surround the baby. While the
rupture of the membranes may not be followed by labor, usually delivery
is indicated as infection (chorioamnionitis)
is a serious threat to both fetus and mother. In some cases, the cervix
dilates prematurely without pain or perceived contractions, so that the
mother may not have warning signs until very late in the birthing
process.
A review into using uterine monitoring at home to detect
contractions and possible preterm births in women at higher risk of
having a preterm baby found that it did not reduce the number of preterm
births.
The research included in the review was poor quality but it showed that
home monitoring may increase the number of unplanned antenatal visits
and may reduce the number of babies admitted to special care when
compared with women receiving normal antenatal care.
Complications
Mortality and morbidity
In the U.S. where many neonatal infections and other causes of neonatal death have been markedly reduced, prematurity is the leading cause of neonatal mortality at 25%. Prematurely born infants are also at greater risk for having subsequent serious chronic health problems as discussed below.
The earliest gestational age at which the infant has at least a 50% chance of survival is referred to as the limit of viability. As NICU care has improved over the last 40 years, the limit of viability has reduced to approximately 24 weeks. Most newborns who die, and 40% of older infants who die, were born between 20 and 25.9 weeks (gestational age), during the second trimester.
As risk of brain damage and developmental delay is significant at that threshold even if the infant survives, there are ethical
controversies over the aggressiveness of the care rendered to such
infants. The limit of viability has also become a factor in the abortion debate.
Specific risks for the preterm neonate
Preterm
infants usually show physical signs of prematurity in reverse
proportion to the gestational age. As a result, they are at risk for
numerous medical problems affecting different organ systems.
- Neurological problems include apnea of prematurity, hypoxic-ischemic encephalopathy (HIE), retinopathy of prematurity (ROP), developmental disability, transient hyperammonemia of the newborn, cerebral palsy and intraventricular hemorrhage, the latter affecting 25% of babies born preterm, usually before 32 weeks of pregnancy. Mild brain bleeds usually leave no or few lasting complications, but severe bleeds often result in brain damage or even death. Neurodevelopmental problems have been linked to lack of maternal thyroid hormones, at a time when their own thyroid is unable to meet postnatal needs.
- Cardiovascular complications may arise from the failure of the ductus arteriosus to close after birth: patent ductus arteriosus (PDA).
- Respiratory problems are common, specifically the respiratory distress syndrome (RDS or IRDS) (previously called hyaline membrane disease). Another problem can be chronic lung disease (previously called bronchopulmonary dysplasia or BPD).
- Gastrointestinal and metabolic issues can arise from neonatal hypoglycemia, feeding difficulties, rickets of prematurity, hypocalcemia, inguinal hernia, and necrotizing enterocolitis (NEC).
- Hematologic complications include anemia of prematurity, thrombocytopenia, and hyperbilirubinemia (jaundice) that can lead to kernicterus.
- Infection, including sepsis, pneumonia, and urinary tract infection
A study of 241 children born between 22 and 25 weeks who were
currently of school age found that 46 percent had severe or moderate
disabilities such as cerebral palsy, vision or hearing loss and learning
problems. Thirty-four percent were mildly disabled and 20 percent had
no disabilities, while 12 percent had disabling cerebral palsy.
Risk factors
The exact cause of preterm birth is difficult to determine and it may be multi-factorial.
Labor is a complex process involving many factors. Four different
pathways have been identified that can result in preterm birth and have
considerable evidence: precocious fetal endocrine activation, uterine
overdistension (placental abruption), decidual bleeding, and
intrauterine inflammation/infection.
Identifying women at high risk of giving birth early would enable
the health services to provide specialized care for these women to
delay the birth or make sure they are in the best place to give birth
(for example a hospital with a special care baby unit). Risk scoring
systems have been suggested as a possible way of identifying these
women. However, there is no research in this area so it is unclear
whether the risk scoring systems would prolong pregnancy and reduce the
numbers of preterm births or not.
Maternal factors
| Risk factor | Relative risk or odds ratio | 95% confidence interval |
|---|---|---|
| Black ethnicity/race | 2.0 | 1.8–2.2 |
| Filipino ancestry | 1.7 | 1.5–2.1 |
| High or low BMI | 0.96 | 0.66–1.4 |
| Large or small pregnancy weight gain | 1.8 | 1.5–2.3 |
| Short maternal height | 1.8 | 1.3–2.5 |
| History of spontaneous preterm birth | 3.6 | 3.2–4.0 |
| Being single/unmarried | 1.2 | 1.03–1.28 |
| Bacterial vaginosis | 2.2 | 1.5–3.1 |
| Asymptomatic bacteriuria | 1.1 | 0.8–1.5 |
| Periodontitis | 1.6 | 1.1–2.3 |
| Low socio-economic status | 1.9 | 1.7–2.2 |
| Short cervical length | 2.9 | 2.1–3.9 |
| Fetal fibronectin | 4.0 | 2.9–5.5 |
| Chlamydia | 2.2 | 1.0–4.8 |
| Celiac disease | 1.4 | 1.2–1.6 |
Percentage premature births in England and Wales 2011, by age of mother and whether single or multiple birth.
A number of factors have been identified that are linked to a higher
risk of a preterm birth such as being less than 18 years of age. Maternal height and weight can play a role.
Further, in the U.S. and the UK, black women have preterm birth rates of 15–18%, more than double than that of the white population. Filipinos
are also at high risk of premature birth, and it is believed that
nearly 11–15% of Filipinos born in the U.S. (compared to other Asians at
7.6% and whites at 7.8%) are premature. Filipinos being a big risk factor is evidenced with the Philippines being the 8th highest ranking in the world for preterm births, the only non-African country in the top 10. This discrepancy is not seen in comparison to other Asian groups or Hispanic immigrants and remains unexplained.
Pregnancy interval makes a difference as women with a six-month
span or less between pregnancies have a two-fold increase in preterm
birth.
Studies on type of work and physical activity have given conflicting
results, but it is opined that stressful conditions, hard labor, and
long hours are probably linked to preterm birth.
A history of spontaneous (i.e., miscarriage) or surgical abortion
has been associated with a small increase in the risk of preterm birth,
with an increased risk with increased number of abortions, although it
is unclear whether the increase is caused by the abortion or by
confounding risk factors (e.g., socioeconomic status). Increased risk has not been shown in women who terminated their pregnancies medically. Pregnancies that are unwanted or unintended are also a risk factor for preterm birth.
Adequate maternal nutrition is important. Women with a low BMI are at increased risk for preterm birth. Further, women with poor nutrition status may also be deficient in vitamins and minerals. Adequate nutrition is critical for fetal development and a diet low in saturated fat and cholesterol may help reduce the risk of a preterm delivery. Obesity does not directly lead to preterm birth; however, it is associated with diabetes and hypertension which are risk factors by themselves.
To some degree those individuals may have underlying conditions (i.e.,
uterine malformation, hypertension, diabetes) that persist.
Women with celiac disease have an increased risk of the development of preterm birth. The risk of preterm birth is more elevated when celiac disease remains undiagnosed and untreated.
Marital status is associated with risk for preterm birth. A study
of 25,373 pregnancies in Finland revealed that unmarried mothers had
more preterm deliveries than married mothers (P=0.001).
Pregnancy outside of marriage was associated overall with a 20%
increase in total adverse outcomes, even at a time when Finland provided
free maternity care. A study in Quebec of 720,586 births from 1990 to
1997 revealed less risk of preterm birth for infants with legally
married mothers compared with those with common-law wed or unwed
parents.
Genetic make-up is a factor in the causality of preterm birth.
Genetics has been a big factor into why Filipinos have a high risk of
premature birth as the Filipinos have a large prevalence of mutations
that help them be predisposed to premature births. An intra- and transgenerational increase in the risk of preterm delivery has been demonstrated. No single gene has been identified.
Subfertility
is associated with preterm birth. Couples who have tried more than 1
year versus those who have tried less than 1 year before achieving a
spontaneous conception have an adjusted odds ratio of 1.35 (95% confidence interval 1.22-1.50) of preterm birth. Pregnancies after IVF
confers a greater risk of preterm birth than spontaneous conceptions
after more than 1 year of trying, with an adjusted odds ratio of 1.55
(95% CI 1.30-1.85).
Factors during pregnancy
The use of fertility medication that stimulates the ovary to release multiple eggs and of IVF with embryo transfer
of multiple embryos has been implicated as an important factor in
preterm birth. Maternal medical conditions increase the risk of preterm
birth. Often labor has to be induced for medical reasons; such
conditions include high blood pressure, pre-eclampsia, maternal diabetes, asthma, thyroid disease, and heart disease.
In a number of women anatomical issues prevent the baby from being carried to term. Some women have a weak or short cervix (the strongest predictor of premature birth).
Women with vaginal bleeding during pregnancy are at higher risk for
preterm birth. While bleeding in the third trimester may be a sign of placenta previa or placental abruption
– conditions that occur frequently preterm – even earlier bleeding that
is not caused by these conditions is linked to a higher preterm birth
rate. Women with abnormal amounts of amniotic fluid, whether too much (polyhydramnios) or too little (oligohydramnios), are also at risk.
The mental status of the women is of significance. Anxiety and depression have been linked to preterm birth.
Finally, the use of tobacco, cocaine, and excessive alcohol
during pregnancy increases the chance of preterm delivery. Tobacco is
the most commonly abused drug during pregnancy and contributes
significantly to low birth weight delivery. Babies with birth defects are at higher risk of being born preterm.
Passive smoking and/or smoking before the pregnancy influences the probability of a preterm birth. The World Health Organization published an international study in March 2014.
Presence of anti-thyroid antibodies is associated with an increased risk preterm birth with an odds ratio of 1.9 and 95% confidence interval of 1.1–3.5.
A 2004 systematic review of 30 studies on the association between
intimate partner violence and birth outcomes concluded that preterm
birth and other adverse outcomes, including death, are higher among
abused pregnant women than among non-abused women.
The Nigerian cultural method of abdominal massage has been shown
to result in 19% preterm birth among women in Nigeria, plus many other
adverse outcomes for the mother and baby.
This ought not be confused with massage conducted by a fully trained
and licensed massage therapist or by significant others trained to
provide massage during pregnancy, which has been shown to have numerous
positive results during pregnancy, including the reduction of preterm
birth, less depression, lower cortisol, and reduced anxiety.
Infection
The frequency of infection in preterm birth is inversely related to the gestational age. Mycoplasma genitalium infection is associated with increased risk of preterm birth, and spontaneous abortion.
Infectious microorganisms can be ascending, hematogeneous,
iatrogenic by a procedure, or retrograde through the Fallopian tubes.
From the deciduas they may reach the space between the amnion and chorion, the amniotic fluid, and the fetus. A chorioamnionitis also may lead to sepsis of the mother. Fetal infection is linked to preterm birth and to significant long-term handicap including cerebral palsy.
It has been reported that asymptomatic colonization of the decidua occurs in up to 70% of women at term using a DNA probe suggesting that the presence of micro-organism alone may be insufficient to initiate the infectious response.
As the condition is more prevalent in black women in the US and
the UK, it has been suggested to be an explanation for the higher rate
of preterm birth in these populations. It is opined that bacterial
vaginosis before or during pregnancy may affect the decidual
inflammatory response that leads to preterm birth. The condition known
as aerobic vaginitis
can be a serious risk factor for preterm labor; several previous
studies failed to acknowledge the difference between aerobic vaginitis
and bacterial vaginosis, which may explain some of the contradiction in
the results.
Untreated yeast infections are associated with preterm birth.
A review into prophylactic antibiotics (given to prevent
infection) in the second and third trimester of pregnancy (13–42 weeks
of pregnancy) found a reduction in the number of preterm births in women
with bacterial vaginosis. These antibiotics also reduced the number of
waters breaking before labor in full-term pregnancies, reduced the risk
of infection of the lining of the womb after delivery (endometritis),
and rates of gonococcal infection. However, the women without bacterial
vaginosis did not have any reduction in preterm births or pre-labor
preterm waters breaking. Much of the research included in this review
lost participants during follow-up so did not report the long-term
effects of the antibiotics on mothers or babies. More research in this
area is needed to find the full effects of giving antibiotics throughout
the second and third trimesters of pregnancy.
A number of maternal bacterial infections are associated with preterm birth including pyelonephritis, asymptomatic bacteriuria, pneumonia, and appendicitis.
A review into giving antibiotics in pregnancy for asymptomatic
bacteriuria (urine infection with no symptoms) found the research was of
very low quality but that it did suggest that taking antibiotics
reduced the numbers of preterm births and babies with low birth weight.
Another review found that one dose of antibiotics did not seem as
effective as a course of antibiotics but fewer women reported side
effects from one dose. This review recommended that more research is needed to discover the best way of treating asymptomatic bacteriuria.
A different review found that preterm births happened less for
pregnant women who had routine testing for low genital tract infections
than for women who only had testing when they showed symptoms of low
genital tract infections.
The women being routinely tested also gave birth to fewer babies with a
low birth weight. Even though these results look promising, the review
was only based on one study so more research is needed into routine
screening for low genital tract infections.
Also periodontal disease has been shown repeatedly to be linked to preterm birth.
In contrast, viral infections, unless accompanied by a significant
febrile response, are considered not to be a major factor in relation to
preterm birth.
Genetics
There is believed to be a maternal genetic component in preterm birth.
Estimated heritability of timing-of-birth in women was 34%. However,
the occurrence of preterm birth in families does not follow a clear
inheritance pattern, thus supporting the idea that preterm birth is a
non-Mendelian trait with a polygenic nature.
Diagnosis
Placental alpha microglobulin-1
Placental alpha microglobulin-1
(PAMG-1) has been the subject of several investigations evaluating its
ability to predict imminent spontaneous preterm birth in women with
signs, symptoms, or complaints suggestive of preterm labor. In one investigation comparing this test to fetal fibronectin testing and cervical length measurement via transvaginal ultrasound,
the test for PAMG-1 (commercially known as the PartoSure test) has been
reported to be the single best predictor of imminent spontaneous
delivery within 7 days of a patient presenting with signs, symptoms, or
complaints of preterm labor. Specifically, the PPV, or positive predictive value, of the tests were 76%, 29%, and 30% for PAMG-1, fFN and CL, respectively (P less than 0.01).
Fetal fibronectin
Fetal fibronectin
(fFN) has become an important biomarker—the presence of this
glycoprotein in the cervical or vaginal secretions indicates that the
border between the chorion and deciduas has been disrupted. A positive
test indicates an increased risk of preterm birth, and a negative test
has a high predictive value.
It has been shown that only 1% of women in questionable cases of
preterm labor delivered within the next week when the test was negative.
Ultrasound
Obstetric ultrasound has become useful in the assessment of the cervix
in women at risk for premature delivery. A short cervix preterm is
undesirable: A cervical length of less than 25 mm at or before 24 weeks
of gestational age is the most common definition of cervical incompetence.
Classification
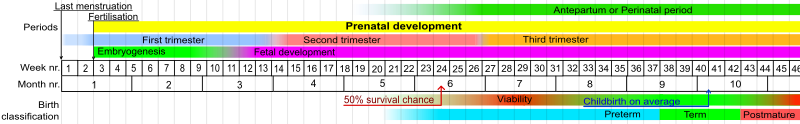
Stages in prenatal development, with weeks and months numbered from last menstruation.
In humans, the usual definition of preterm birth is birth before a gestational age of 37 complete weeks.
In the normal human fetus, several organ systems mature between 34 and
37 weeks, and the fetus reaches adequate maturity by the end of this
period. One of the main organs greatly affected by premature birth is
the lungs. The lungs are one of the last organs to mature in the womb;
because of this, many premature babies spend the first days and weeks of
their lives on ventilators.
Therefore, a significant overlap exists between preterm birth and
prematurity. Generally, preterm babies are premature and term babies are
mature. Preterm babies born near 37 weeks often have no problems
relating to prematurity if their lungs have developed adequate surfactant,
which allows the lungs to remain expanded between breaths. Sequelae of
prematurity can be reduced to a small extent by using drugs to
accelerate maturation of the fetus, and to a greater extent by
preventing preterm birth.
Prevention
Historically
efforts have been primarily aimed to improve survival and health of
preterm infants (tertiary intervention). Such efforts, however, have not
reduced the incidence of preterm birth. Increasingly primary
interventions that are directed at all women, and secondary intervention
that reduce existing risks are looked upon as measures that need to be
developed and implemented to prevent the health problems of premature
infants and children. Smoking bans are effective in decreasing preterm births.
Before pregnancy
Adoption
of specific professional policies can immediately reduce risk of
preterm birth as the experience in assisted reproduction has shown when
the number of embryos during embryo transfer was limited.
Many countries have established specific programs to protect pregnant
women from hazardous or night-shift work and to provide them with time
for prenatal visits and paid pregnancy-leave. The EUROPOP study showed
that preterm birth is not related to type of employment, but to
prolonged work (over 42 hours per week) or prolonged standing (over 6
hours per day). Also, night work has been linked to preterm birth. Health policies that take these findings into account can be expected to reduce the rate of preterm birth.
Preconceptional intake of folic acid
is recommended to reduce birth defects. There is significant evidence
that long-term (more than one year) use of folic acid supplement
preconceptionally may reduce premature birth. Reducing smoking is expected to benefit pregnant women and their offspring.
During pregnancy
Healthy
eating can be instituted at any stage of the pregnancy including
nutritional adjustments, use of vitamin supplements, and smoking cessation.
Calcium supplementation in women who have low dietary calcium may
reduce the number of negative outcomes including preterm birth,
pre-eclampsia, and maternal death.
The World Health Organization (WHO) suggests 1.5–2 g of calcium
supplements daily, for pregnant women who have low levels calcium in
their diet. Supplemental intake of C and E vitamins have not been found to reduce preterm birth rates.
Different strategies are used in the administration of prenatal care,
and future studies need to determine if the focus can be on screening
for high-risk women, or widened support for low-risk women, or to what
degree these approaches can be merged.
While periodontal infection has been linked with preterm birth,
randomized trials have not shown that periodontal care during pregnancy
reduces preterm birth rates.
Screening of low risk women
Screening
for asymptomatic bacteriuria followed by appropriate treatment reduces
pyelonephritis and reduces the risk of preterm birth.
Extensive studies have been carried out to determine if other forms of
screening in low-risk women followed by appropriate intervention are
beneficial, including: Screening for and treatment of Ureaplasma
urealyticum, group B streptococcus, Trichomonas vaginalis, and bacterial
vaginosis did not reduce the rate of preterm birth. Routine ultrasound examination of the length of the cervix identifies patients at risk, but cerclage is not proven useful, and the application of a progestogen is under study. Screening for the presence of fibronectin in vaginal secretions is not recommended at this time in women at low risk.
Self-care
Self-care
methods to reduce the risk of preterm birth include proper nutrition,
avoiding stress, seeking appropriate medical care, avoiding infections,
and the control of preterm birth risk factors (e.g. working long hours
while standing on feet, carbon monoxide exposure, domestic abuse, and
other factors). Self-monitoring vaginal pH followed by yogurt treatment
or clindamycin treatment if the pH was too high all seem to be effective
at reducing the risk of preterm birth. Additional support during pregnancy does not appear to prevent low birthweight or preterm birth.
Reducing existing risks
Women
are identified to be at increased risk for preterm birth on the basis
of their past obstetrical history or the presence of known risk factors.
Preconception intervention can be helpful in selected patients in a
number of ways. Patients with certain uterine anomalies may have a
surgical correction (i.e. removal of a uterine septum),
and those with certain medical problems can be helped by optimizing
medical therapies prior to conception, be it for asthma, diabetes,
hypertension and others.
Multiple pregnancies
In multiple pregnancies, which often result from use of assisted reproductive technology, there is a high risk of preterm birth. Selective reduction is used to reduce the number of fetuses to two or three.
Reducing indicated preterm birth
A number of agents have been studied for the secondary prevention of indicated preterm birth. Trials using low-dose aspirin, fish oil,
vitamin C and E, and calcium to reduce preeclampsia demonstrated some
reduction in preterm birth only when low-dose aspirin was used. Even if agents such as calcium or antioxidants were able to reduce preeclampsia, a resulting decrease in preterm birth was not observed.
Reducing spontaneous preterm birth
Reduction
in activity by the mother—pelvic rest, limited work, bed rest—may be
recommended although there is no evidence it is useful with some
concerns it is harmful. Increasing medical care by more frequent visits and more education has not been shown to reduce preterm birth rates. Use of nutritional supplements such as omega-3 polyunsaturated fatty acids
is based on the observation that populations who have a high intake of
such agents are at low risk for preterm birth, presumably as these
agents inhibit production of proinflammatory cytokines. A randomized
trial showed a significant decline in preterm birth rates, and further studies are in the making.
Antibiotics
While antibiotics can get rid of bacterial vaginosis in pregnancy, this does not appear to change the risk of preterm birth.
It has been suggested that chronic chorioamnionitis is not sufficiently
treated by antibiotics alone (and therefore they cannot ameliorate the
need for preterm delivery in this condition).
Progestogens
Progestogens, often given in the form of progesterone or hydroxyprogesterone caproate,
relaxes the uterine musculature, maintains cervical length, and has
anti-inflammatory properties, and thus exerts activities expected to be
beneficial in reducing preterm birth. Two meta-analyses demonstrated a
reduction in the risk of preterm birth in women with recurrent preterm
birth by 40–55%.
Progestogen supplementation also reduces the frequency of preterm birth in pregnancies where there is a short cervix. However, progestogens are not effective in all populations, as a study involving twin gestations failed to see any benefit.
Cervical cerclage
In preparation for childbirth, the woman's cervix shortens. Preterm cervical shortening is linked to preterm birth and can be detected by ultrasonography. Cervical cerclage
is a surgical intervention that places a suture around the cervix to
prevent its shortening and widening. Numerous studies have been
performed to assess the value of cervical cerclage and the procedure
appears helpful primarily for women with a short cervix and a history of
preterm birth.
Instead of a prophylactic cerclage, women at risk can be monitored
during pregnancy by sonography, and when shortening of the cervix is
observed, the cerclage can be performed.
Management
Preterm birth at 32 weeks and 4 days with a weight of 2,000 g attached to medical equipment
About 75% of nearly a million deaths due to preterm deliver would
survive if provided warmth, breastfeeding, treatments for infection, and
breathing support. If a baby has cardiac arrest at birth and is before 23 weeks or less than 400 g attempts at resuscitation are not indicated.
Tertiary interventions are aimed at women who are about to go
into preterm labor, or rupture the membranes or bleed preterm. The use
of the fibronectin test
and ultrasonography improves the diagnostic accuracy and reduces
false-positive diagnosis. While treatments to arrest early labor where
there is progressive cervical dilatation and effacement will not be
effective to gain sufficient time to allow the fetus to grow and mature
further, it may defer delivery sufficiently to allow the mother to be
brought to a specialized center that is equipped and staffed to handle
preterm deliveries. In a hospital setting women are hydrated via intravenous infusion (as dehydration can lead to premature uterine contractions).
Steroids
Severely premature infants may have underdeveloped lungs because they are not yet producing their own surfactant. This can lead directly to respiratory distress syndrome,
also called hyaline membrane disease, in the neonate. To try to reduce
the risk of this outcome, pregnant mothers with threatened premature
delivery prior to 34 weeks are often administered at least one course of
glucocorticoids, a steroid that crosses the placental barrier and stimulates the production of surfactant in the lungs of the baby. Steroid use up to 37 weeks is also recommended by the American Congress of Obstetricians and Gynecologists. Typical glucocorticoids that would be administered in this context are betamethasone or dexamethasone, often when the pregnancy has reached viability at 23 weeks.
In cases where premature birth is imminent, a second "rescue"
course of steroids may be administered 12 to 24 hours before the
anticipated birth. There are still some concerns about the efficacy and
side effects of a second course of steroids, but the consequences of RDS
are so severe that a second course is often viewed as worth the risk. A
2015 Cochrane
review supports the use of repeat dose(s) of prenatal corticosteroids
for women still at risk of preterm birth seven days or more after an
initial course.
Beside reducing respiratory distress, other neonatal
complications are reduced by the use of glucocorticosteroids, namely
intraventricular bleeding, necrotising enterocolitis, and patent ductus arteriosus.
A single course of antenatal corticosteroids could be considered
routine for preterm delivery, but there are some concerns about
applicability of this recommendation to low-resource settings with high
rates of infections. It remains unclear whether one corticosteroid (or one particular regimen) has advantages over another.
Concerns about adverse effects of prenatal corticosteroids
include increased risk for maternal infection, difficulty with diabetic
control, and possible long-term effects on neurodevelopmental outcomes
for the infants. There is ongoing discussion about when steroids should
be given (i.e. only antenatally or postnatally too) and for how long
(i.e. single course or repeated administration). Despite these unknowns,
there is a consensus that the benefits of a single course of prenatal
glucocorticosteroids vastly outweigh the potential risks.
Antibiotics
The
routine administration of antibiotics to all women with threatened
preterm labor reduces the risk of the baby to get infected with group B streptococcus and has been shown to reduce related mortality rates.
When membranes rupture prematurely, obstetrical management looks
for development of labor and signs of infection. Prophylactic antibiotic
administration has been shown to prolong pregnancy and reduced neonatal
morbidity with rupture of membranes at less than 34 weeks. Because of concern about necrotizing enterocolitis, amoxicillin or erythromycin has been recommended, but not amoxicillin + clavulanic acid (co-amoxiclav).
Tocolysis
A number of medications may be useful to delay delivery including: nonsteroidal anti-inflammatory drugs, calcium channel blockers, beta mimetics, and atosiban. Tocolysis rarely delays delivery beyond 24–48 hours.
This delay, however, may be sufficient to allow the pregnant woman to
be transferred to a center specialized for management of preterm
deliveries and give administered corticosteroids to reduce neonatal
organ immaturity. Meta-analyses indicate that calcium-channel blockers
and an oxytocin antagonist can delay delivery by 2–7 days, and β2-agonist drugs delay by 48 hours but carry more side effects. Magnesium sulfate does not appear to be useful to prevent preterm birth. Its use before delivery, however, does appear to decrease the risk of cerebral palsy.
Mode of delivery
The routine use of caesarean section for early delivery of infants expected to have very low birth weight is controversial, and a decision concerning the route and time of delivery probably needs to be made on a case by case basis.
Neonatal care
Incubator for preterm baby
After delivery, plastic wraps or warm mattresses are useful to keep the infant warm on their way to the neonatal intensive care unit (NICU).
In developed countries premature infants are usually cared for in an
NICU. The physicians who specialize in the care of very sick or
premature babies are known as neonatologists. In the NICU, premature babies are kept under radiant warmers or in incubators (also called isolettes), which are bassinets
enclosed in plastic with climate control equipment designed to keep
them warm and limit their exposure to germs. Modern neonatal intensive
care involves sophisticated measurement of temperature, respiration,
cardiac function, oxygenation, and brain activity. Treatments may include fluids and nutrition through intravenous catheters, oxygen supplementation, mechanical ventilation support,
and medications. In developing countries where advanced equipment and
even electricity may not be available or reliable, simple measures such
as kangaroo care (skin to skin warming), encouraging breastfeeding, and basic infection control measures can significantly reduce preterm morbidity and mortality. Bili lights may also be used to treat newborn jaundice (hyperbilirubinemia).
Water can be carefully provided to prevent dehydration but no so much to increase risks of side effects.
In a 2012 policy statement, the American Academy of Pediatrics recommended feeding preterm infants human milk, finding "significant short- and long-term beneficial effects," including lower rates of necrotizing enterocolitis (NEC). It is unclear if fortification of breast milk improves outcomes in preterm babies, though it may speed growth. There is limited evidence to support prescribing a preterm formula for the preterm babies after hospital discharge.
Prognosis
Preterm infants survival rates
The chance of survival at 22 weeks is about 6%, while at 23 weeks it is 26%, 24 weeks 55% and 25 weeks about 72%. The chances of survival without long-term difficulties is less. In the developed world overall survival is about 90% while in low-income countries survival rates are about 10%.
Some children will adjust well during childhood and adolescence,
although disability is more likely nearer the limits of viability. A
large study followed children born between 22 and 25 weeks until the age
of 6 years old. Of these children, 46 percent had moderate to severe
disabilities such as cerebral palsy, vision or hearing loss and learning
disabilities, 34 percent had mild disabilities, and 20 percent had no
disabilities. Twelve percent had disabling cerebral palsy.
As survival has improved, the focus of interventions directed at
the newborn has shifted to reduce long-term disabilities, particularly
those related to brain injury.
Some of the complications related to prematurity may not be apparent
until years after the birth. A long-term study demonstrated that the
risks of medical and social disabilities extend into adulthood and are
higher with decreasing gestational age at birth and include cerebral palsy, intellectual disability, disorders of psychological development, behavior, and emotion, disabilities of vision and hearing, and epilepsy.
Standard intelligence tests showed that 41 percent of children born
between 22 and 25 weeks had moderate or severe learning disabilities
when compared to the test scores of a group of similar classmates who
were born at full-term. It is also shown that higher levels of education were less likely to be obtained with decreasing gestational age at birth. People born prematurely may be more susceptible to developing depression as teenagers.
Some of these problems can be described as being within the executive domain and have been speculated to arise due to decreased myelinization of the frontal lobes. Studies of people born premature and investigated later with MRI brain imaging,
demonstrate qualitative anomalies of brain structure and grey matter
deficits within temporal lobe structures and the cerebellum that persist
into adolescence.
Throughout life they are more likely to require services provided by
physical therapists, occupational therapists, or speech therapists.
Despite the neurosensory, mental and educational problems studied
in school age and adolescent children born extremely preterm, the
majority of preterm survivors born during the early years of neonatal
intensive care are found to do well and to live fairly normal lives in
young adulthood.
Young adults born preterm seem to acknowledge that they have more
health problems than their peers, yet feel the same degree of
satisfaction with their quality of life.
Beyond the neurodevelopmental consequences of prematurity,
infants born preterm have a greater risk for many other health problems.
For instance, children born prematurely have an increased risk for
developing chronic kidney disease.
Epidemiology
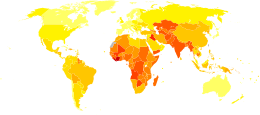
Disability-adjusted life year for prematurity and low birth weight per 100,000 inhabitants in 2004.
no data
less than 120
120-240
240-360
360-480
480-600
600-720
720-840
840-960
960-1080
1080-1200
1200-1500
more than 1500
Preterm birth complicates the births of infants worldwide affecting 5% to 18% of births.
In Europe and many developed countries the preterm birth rate is
generally 5–9%, and in the USA it has even risen to 12–13% in the last
decades.
As weight is easier to determine than gestational age, the World Health Organization tracks rates of low birth weight (less than 2,500 grams), which occurred in 16.5 percent of births in less developed regions in 2000.
It is estimated that one third of these low birth weight deliveries are
due to preterm delivery. Weight generally correlates to gestational
age, however, infants may be underweight for other reasons than a
preterm delivery. Neonates of low birth weight (LBW) have a birth weight
of less than 2500 g (5 lb 8 oz) and are mostly but not exclusively
preterm babies as they also include small for gestational age (SGA) babies. Weight-based classification further recognizes Very Low Birth Weight (VLBW) which is less than 1,500 g, and Extremely Low Birth Weight (ELBW) which is less than 1,000 g. Almost all neonates in these latter two groups are born preterm.
Complications from preterm births resulted in 740,000 deaths in 2013, down from 1.57 million in 1990.
Society and culture
Economics
Preterm
birth is a significant cost factor in healthcare, not even considering
the expenses of long-term care for individuals with disabilities due to
preterm birth. A 2003 study in the US determined neonatal costs to be
$224,400 for a newborn at 500–700 g versus $1,000 at over 3,000 g. The
costs increase exponentially with decreasing gestational age and weight.
The 2007 Institute of Medicine report Preterm Birth
found that the 550,000 premature babies born each year in the U.S. run
up about $26 billion in annual costs, mostly related to care in neonatal
intensive care units, but the real tab may top $50 billion.
Notable cases
James Elgin Gill (born on 20 May 1987 in Ottawa,
Ontario, Canada) was the earliest premature baby in the world, until
that record was broken in 2014. He was 128 days premature (21 weeks and 5
days' gestation) and weighed 1 pound 6 ounces (624 g). He survived.
In 2014, Lyla Stensrud, born in San Antonio,
Texas, U.S. became the youngest premature baby in the world. She was
born at 21 weeks 4 days and weighed 410 grams (less than a pound).
Kaashif Ahmad resuscitated the baby after she was born. As of November
2018, Lyla was attending preschool. She had a slight delay in speech,
but no other known medical issues or disabilities.
Amillia Taylor is also often cited as the most premature baby. She was born on 24 October 2006 in Miami, Florida, U.S. at 21 weeks and 6 days' gestation. This report has created some confusion as her gestation was measured from the date of conception (through in vitro
fertilization) rather than the date of her mother's last menstrual
period, making her appear 2 weeks younger than if gestation was
calculated by the more common method. At birth, she was 9 inches (22.9 cm) long and weighed 10 ounces (280 g). She suffered digestive and respiratory problems, together with a brain hemorrhage. She was discharged from the Baptist Children's Hospital on 20 February 2007.
The record for the smallest premature baby to survive was held
for a considerable amount of time by Madeline Mann, who was born in 1989
at 26 weeks, weighing 9.9 ounces (280 g) and measuring 9.5 inches
(241.3 mm) long.
This record was broken in September 2004 by Rumaisa Rahman, who was
born in the same hospital, Loyola University Medical Center in Maywood,
Illinois. at 25 weeks' gestation. At birth, she was 8 inches (200 mm) long and weighed 261 grams (9.2 oz). Her twin sister was also a small baby, weighing 563 grams (1 lb 3.9 oz) at birth. During pregnancy their mother had pre-eclampsia, requiring birth by caesarean section.
The larger twin left the hospital at the end of December, while the
smaller remained there until 10 February 2005 by which time her weight
had increased to 1.18 kg (2.6 lb). Generally healthy, the twins had to undergo laser eye surgery to correct vision problems, a common occurrence among premature babies.
In May 2019, Sharp Mary Birch Hospital for Women & Newborns in San Diego
announced that a baby nicknamed "Saybie" had been discharged almost
five months after being born at 23 weeks gestation and weighing 244
grams (8.6 oz). Saybie was confirmed by Dr. Edward Bell of the University of Iowa to be the new smallest surviving premature baby.
The world's smallest premature boy to survive was born in February 2009 at Children's Hospitals and Clinics of Minnesota in Minneapolis, Minnesota, U.S.. Jonathon Whitehill was born at 25 weeks' gestation with a weight of 310 grams (11 oz). He was hospitalized in a neonatal intensive care unit for five months, and then discharged.
Historical figures who were born prematurely include Johannes Kepler (born in 1571 at seven months' gestation), Isaac Newton (born in 1642, small enough to fit into a quart mug, according to his mother), Winston Churchill (born in 1874 at seven months' gestation), and Anna Pavlova (born in 1885 at seven months' gestation),