 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˈfɛntənɪl/ or /ˈfɛntənəl/ |
| Trade names | Actiq, Duragesic, Fentora, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a605043 |
| License data | |
| Pregnancy category |
|
| Dependence liability | High |
| Routes of administration | Buccal, epidural, IM, IT, IV, sublingual, skin patch |
| Drug class | Opioid |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 92% (transdermal) 89% (intranasal) 50% (buccal) 33% (ingestion) 100% (intramuscular) 55% (inhaled) |
| Protein binding | 80–85% |
| Metabolism | Liver, primarily by CYP3A4 |
| Onset of action | 5 minutes |
| Elimination half-life | IV: 6 mins (T1/2 α) 1 hours (T1/2 β) 16 hours (T1/2 ɣ) Intranasal: 6.5 hours Transdermal: 20–27 hours Sublingual/buccal (single dose): 2.6–13.5 hours |
| Duration of action | IV: 30–60 minutes |
| Excretion | Mostly urinary (metabolites, <10% unchanged drug) |
| Identifiers | |
| CAS Number | |
|---|---|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.006.468 |
| Chemical and physical data | |
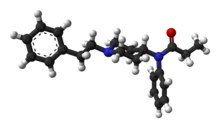
| Formula | C22H28N2O |
| Molar mass | 336.479 g·mol−1 |
| 3D model (JSmol) | |
| Density | 1.1 g/cm3 |
| Melting point | 87.5 °C (189.5 °F) |
| (verify) |
Fentanyl, also spelled fentanil, is an opioid used as a pain medication and together with other medications for anesthesia. It is also used as a recreational drug, often mixed with heroin or cocaine. It has a rapid onset and its effects generally last under two hours. Medically, it is used by injection, nasal spray, skin patch, or absorbed through the cheek (transmucosal) as a lozenge or tablet.
Common side effects include vomiting, constipation, sedation, confusion, hallucinations, nausea, and injuries related to poor coordination. Serious side effects may include decreased breathing (respiratory depression), serotonin syndrome, low blood pressure, addiction, or coma. Fentanyl works primarily by activating μ-opioid receptors. It is around 100 times stronger than morphine, about 50 times stronger than heroin. Some fentanyl analogues such as carfentanil are up to ~10,000 times stronger than morphine.
Fentanyl was first made by Paul Janssen in 1960 and approved for medical use in the United States in 1968. In 2015, 1,600 kilograms (3,500 lb) were used in healthcare globally. As of 2017, fentanyl was the most widely used synthetic opioid in medicine. Fentanyl patches for cancer pain are on the World Health Organization's List of Essential Medicines. In 2016, fentanyl and analogues were the most common cause of overdose deaths in the United States at more than 20,000, about half of all opioid-related deaths. Most of these overdose deaths were due to illegally made fentanyl.
In recent years fentanyl has disrupted the North American drug market, capitalizing on pre-existing demand for opiates such as heroin and prescription pharmaceuticals. In 2017, it was the 250th most commonly prescribed medication in the United States, with more than 1.7 million prescriptions. At the same time, there is concern that the growing demand may prove highly attractive to organized crime and aspiring criminals, especially those operating in areas around the Golden Triangle in Southeast Asia and Shan State in Myanmar where production of synthetic drugs has expanded dramatically over the last decade. Compared to heroin, it is more potent, has higher profit margins and, because it is compact, has simpler logistics. It can be cut into, or even replace entirely, the supply of heroin and other opiates.
Medical uses
Anesthesia
Intravenous fentanyl is often used for anesthesia and to treat pain. To induce anesthesia, it is given with a sedative-hypnotic, like propofol or thiopental, and a muscle relaxant. To maintain anesthesia, inhaled anesthetics and additional fentanyl may be used. These are often given in 15–30 minute intervals throughout procedures such as endoscopy, surgeries, and in emergency rooms.
For pain relief after surgery, use can decrease the amount of inhalational anesthetic needed for emergence from anesthesia. Balancing this medication and titrating the drug based on expected stimuli and the person's responses can result in a stable blood pressure and heart rate throughout a procedure and a faster emergence from anesthesia with minimal pain.
Obstetrics
Fentanyl is sometimes given intrathecally as part of spinal anesthesia or epidurally for epidural anaesthesia and analgesia. Because of fentanyl's high lipid solubility, its effects are more localized than morphine, and some clinicians prefer to use morphine to get a wider spread of analgesia. However, it is widely used in obstetrical anesthesia because of its short time to action peak (about 5 min), the rapid termination of its effect after a single dose, and the occurrence of relative cardiovascular stability. In obstetrics, the dose must be closely regulated in order to prevent large amounts of transfer from mother to fetus. At high doses, the drug may act on the fetus to cause postnatal respiratory distress. For this reason, shorter acting agents such as alfentanyl or remifentanil may be more suitable in the context of inducing general anaesthesia.
Pain management
The bioavailability of intranasal fentanyl is about 70–90%, but with some imprecision due to clotted nostrils, pharyngeal swallow and incorrect administration. For both emergency and palliative use, intranasal fentanyl is available in doses of 50, 100, and 200 µg. In emergency medicine, safe administration of intranasal fentanyl with a low rate of side effects and a promising pain reducing effect was demonstrated in a prospective observational study in about 900 out-of-hospital patients.
In children, intranasal fentanyl is useful for the treatment of moderate and severe pain and is well tolerated.
Chronic pain
It is also used in the management of chronic pain including cancer pain. Often, transdermal patches are used. The patches work by slowly releasing fentanyl through the skin into the bloodstream over 48 to 72 hours, allowing for long-lasting pain management. Dosage is based on the size of the patch, since, in general, the transdermal absorption rate is constant at a constant skin temperature. Rate of absorption is dependent on a number of factors. Body temperature, skin type, amount of body fat, and placement of the patch can have major effects. The different delivery systems used by different makers will also affect individual rates of absorption. Under normal circumstances, the patch will reach its full effect within 12 to 24 hours; thus, fentanyl patches are often prescribed with a fast-acting opioid (such as morphine or oxycodone) to handle breakthrough pain. It is unclear if fentanyl gives long-term pain relief to people with neuropathic pain.
Breakthrough pain
Sublingual fentanyl dissolves quickly and is absorbed through the sublingual mucosa to provide rapid analgesia. Fentanyl is a highly lipophilic compound, which is well absorbed sublingually and generally well tolerated. Such forms are particularly useful for breakthrough cancer pain episodes, which are often rapid in onset, short in duration and severe in intensity.
Palliative care
In palliative care, transdermal fentanyl patches have a definitive, but limited role for:
- people already stabilized on other opioids who have persistent swallowing problems and cannot tolerate other parenteral routes such as subcutaneous administration.
- people with moderate to severe kidney failure.
- troublesome side effects of oral morphine, hydromorphone, or oxycodone.
When using the transdermal patch, patients must be careful to minimize or avoid external heat sources (direct sunlight, heating pads, etc.), which can trigger the release of too much medication and cause potentially deadly complications.
Combat medicine
USAF Pararescue combat medics in Afghanistan use fentanyl lozenges in the form of lollipops on combat casualties from IED blasts and other trauma. The stick is taped to a finger and the lozenge put in the cheek of the person. When enough fentanyl has been absorbed, the (sedated) person generally lets the lollipop fall from the mouth, indicating sufficient analgesia and somewhat reducing the likelihood of overdose and associated risks.
Other
Some routes of administration such as nasal sprays and inhalers generally result in faster onset of high blood levels, which can provide more immediate analgesia but also more severe side effects, especially in overdose. The much higher cost of some of these appliances may not be justified by marginal benefit compared with buccal or oral options. Intranasal fentanyl appears to be as equally effective as IV morphine and superior to intramuscular morphine for management of acute hospital pain.
A fentanyl patient-controlled transdermal system (PCTS) is under development, which aims to allow patients to control administration of fentanyl through the skin to treat postoperative pain.
Adverse effects
Fentanyl's most common side effects, which affect more than 10% of people, include diarrhea, nausea, constipation, dry mouth, somnolence, confusion, asthenia (weakness), sweating. Less frequently, in 3-10% of people, fentanyl can cause abdominal pain, headache, fatigue, anorexia and weight loss, dizziness, nervousness, hallucinations, anxiety, depression, flu-like symptoms, dyspepsia (indigestion), shortness of breath, hypoventilation, apnoea, and urinary retention. Fentanyl use has also been associated with aphasia. Despite being a more potent analgesic, fentanyl tends to induce less nausea, as well as less histamine-mediated itching, than morphine.
The duration of action of fentanyl has sometimes been underestimated, leading to harm in a medical context. In 2006, the U.S. Food and Drug Administration (FDA) began investigating several respiratory deaths, but doctors in the United Kingdom were not warned of the risks with fentanyl until September 2008. The FDA reported in April 2012 that twelve young children had died and twelve more made seriously ill from separate accidental exposures to fentanyl skin patches.
Fentanyl has a therapeutic index of 270.
Respiratory depression
The most dangerous adverse effect of fentanyl is respiratory depression, that is, decreased sensitivity to carbon dioxide leading to reduced rate of breath intake, which can cause complications or suffocation. This risk is decreased when the airway is secured with an endotracheal tube. This risk is higher in specific groups, like those with obstructive sleep apnea.
Other factors that increase the risk of respiratory depression are:
- High fentanyl doses
- Sleep
- Older age
- Concomitant use of CNS depressants like benzodiazepines, barbiturates, alcohol, and inhaled anesthetics
- Hyperventilation
- Decreased CO2 levels in the serum
- Respiratory acidosis
- Decreased fentanyl clearance from the body
- Decreased blood flow to the liver
- Renal insufficiency
Sustained release fentanyl preparations, such as patches, may also produce unexpected delayed respiratory depression. The precise reason for sudden respiratory depression is unclear, but there are several hypotheses:
- Saturation of the body fat compartment in people with rapid and profound body fat loss (people with cancer, cardiac or infection-induced cachexia can lose 80% of their body fat).
- Early carbon dioxide retention causing cutaneous vasodilation (releasing more fentanyl), together with acidosis, which reduces protein binding of fentanyl, releasing yet more fentanyl.
- Reduced sedation, losing a useful early warning sign of opioid toxicity and resulting in levels closer to respiratory-depressant levels.
Heart and blood vessels
- Bradycardia: Fentanyl decreases the heart rate by increasing vagal nerve tone in the brainstem, which increases the parasympathetic drive.
- Vasodilation: It also vasodilates arterial and venous blood vessels through a central mechanism, by primarily slowing down vasomotor centers in the brainstem. To a lesser extent, it does this by directly affecting blood vessels. This is much more profound in patients who have an already increased sympathetic drive, like patients who have high blood pressure or congestive heart failure. It does not affect the contractility of the heart when regular doses are administered.
Muscle rigidity
If high boluses of fentanyl are administered quickly, muscle rigidity of the vocal cords can make bag-mask ventilation very difficult. The exact mechanism of this effect is unknown, but it can be prevented and treated using neuromuscular blockers.
Overdose
Naloxone can completely or partially reverse an opioid overdose. In July 2014, the Medicines and Healthcare products Regulatory Agency (MHRA) of the UK issued a warning about the potential for life-threatening harm from accidental exposure to transdermal fentanyl patches, particularly in children, and advised that they should be folded, with the adhesive side in, before being discarded. The patches should be kept away from children, who are most at risk from fentanyl overdose. In the US, fentanyl and fentanyl analogs caused over 29,000 deaths in 2017, a large increase over the previous four years.
Death from fentanyl overdose continues to be a public health of national concern in Canada since September 2015. In 2016, deaths from fatal fentanyl overdoses in the province of British Columbia averaged two persons per day. In 2017 the death rate rose over 100% with 368 overdose related deaths in British Columbia between January and April 2017.
Fentanyl has started to make its way into heroin and oxycodone, and more recently, cocaine, ketamine and methamphetamine. A kilogram of heroin laced with fentanyl may sell for more than US$100,000, but the fentanyl itself may be produced far more cheaply for about US$6,000 per kilogram. Fentanyl was often produced in China and exported illegally to the U.S. The UK drug market is no longer reliant on China as domestic production is replacing imports.
As of 2018 fentanyl was the most commonly listed opioid in overdose drug deaths, surpassing heroin. From 2013 until 2016, overdose deaths involving fentanyl increased 113% per year.
The intravenous dose causing 50% of experimental subjects to die (LD50) is "3 mg/kg in rats, 1 mg/kg in cats, 14 mg/kg in dogs, and 0.03 mg/kg in monkeys." The LD50 in mice has been given as 6.9 mg/kg by intravenous administration, 17.5 mg/kg intraperitoneally, 27.8 mg/kg by oral administration. The LD50 in humans is unknown, but a lethal dose for the average person is estimated to be 2 mg.
Pharmacology
Classification
Fentanyl is a synthetic opioid in the phenylpiperidine family, which includes sufentanil, alfentanil, remifentanil, and carfentanil.
Structure-activity
The structures of opioids share many similarities. Whereas opioids like codeine, hydrocodone, oxycodone, and hydromorphone are synthesized by simple modifications of morphine, fentanyl and its relatives are synthesized by modifications of meperidine. Meperidine is a fully synthetic opioid, and other members of the phenylpiperidine family like alfentanil and sufentanil are complex versions of this structure.
Like other opioids, fentanyl is a weak base that is highly lipid-soluble, protein-bound, and protonated at physiological pH. All of these factors allow it to rapidly cross cellular membranes, contributing to its quick effect in the body and the central nervous system.
Mechanism of action
| Affinities, Ki | Ratio | ||
|---|---|---|---|
| MOR | DOR | KOR | MOR:DOR:KOR |
| 0.39 nM | >1,000 nM | 255 nM | 1:>2564:654 |
Fentanyl, like other opioids, acts on opioid receptors. These receptors are G-protein-coupled receptors, which contain seven transmembrane portions, intracellular loops, extracellular loops, intracellular C-terminus, and extracellular N-terminus. The extracellular N-terminus is important in differentiating different types of binding substrates. When fentanyl binds, downstream signaling leads to the inhibitory effects, such as decreased cAMP production, decreased calcium ion influx, and increased potassium efflux. This inhibits the ascending pathways in the central nervous system to increase pain threshold by changing the perception of pain; this is mediated by decreasing propagation of nociceptive signals, resulting in analgesic effects.
As a μ-receptor agonist, fentanyl binds 50 to 100 times more potently than morphine. It can also bind to the delta and kappa opioid receptors but with a lower affinity. It has high lipid solubility, allowing it to more easily penetrate the central nervous system. It attenuates "second pain" with primary effects on slow-conducting, unmyelintated C-fibers and is less effective on neuropathic pain and "first pain" signals through small, myelinated A-fibers.
Fentanyl can produce the following clinical effects strongly, through μ-receptor agonism.
- Supraspinal analgesia (μ1)
- Respiratory depression (μ2)
- Physical dependence
- Muscle rigidity
It produces sedation and spinal analgesia through Κ-receptor agonism.
Therapeutic effects
- Pain relief: Primarily, fentanyl provides the relief of pain by acting on brain and spinal μ-receptors.
- Sedation: Fentanyl produces sleep and drowsiness, as dosage is increased, and can produce the δ-waves often seen in natural sleep on electroencephalogram.
- Suppression of the cough reflex: Fentanyl can decrease the struggle against an endotracheal tube and excessive coughing by decreasing the cough reflex, becoming useful when intubating people who are awake and have compromised airways. After receiving a bolus dose of fentanyl, people can also experience paradoxical coughing, which is a phenomenon that is not well understood.
Detection in biological fluids
Fentanyl may be measured in blood or urine to monitor for abuse, confirm a diagnosis of poisoning, or assist in a medicolegal death investigation. Commercially available immunoassays are often used as initial screening tests, but chromatographic techniques are generally used for confirmation and quantitation. The Marquis Color test may also be used to detect the presence of fentanyl. Using formaldehyde and sulfuric acid, the solution will turn purple when introduced to opium drugs. Blood or plasma fentanyl concentrations are expected to be in a range of 0.3–3.0 μg/L in persons using the medication therapeutically, 1–10 μg/L in intoxicated people and 3–300 μg/L in victims of acute overdosage. Paper spray-mass spectrometry (PS-MS) may be useful for initial testing of samples.
History
Fentanyl was first synthesized in Belgium by Paul Janssen under the label of his relatively newly formed Janssen Pharmaceutica in 1959. It was developed by screening chemicals similar to pethidine (meperidine) for opioid activity. The widespread use of fentanyl triggered the production of fentanyl citrate (the salt formed by combining fentanyl and citric acid in a 1:1 stoichiometric ratio). Fentanyl citrate entered medical use as a general anaesthetic in 1968, manufactured by McNeil Laboratories under the trade name Sublimaze.
In the mid-1990s, Janssen Pharmaceutica developed and introduced into clinical trials the Duragesic patch, which is a formulation of an inert alcohol gel infused with select fentanyl doses, which are worn to provide constant administration of the opioid over a period of 48 to 72 hours. After a set of successful clinical trials, Duragesic fentanyl patches were introduced into medical practice.
Following the patch, a flavoured lollipop of fentanyl citrate mixed with inert fillers was introduced in 1998 under the brand name of Actiq, becoming the first quick-acting formation of fentanyl for use with chronic breakthrough pain.
In 2009, the US Food and Drug Administration approved Onsolis (fentanyl buccal soluble film), a fentanyl drug in a new dosage form for cancer pain management in opioid-tolerant subjects. It uses a medication delivery technology called BEMA (BioErodible MucoAdhesive), a small dissolvable polymer film containing various fentanyl doses applied to the inner lining of the cheek.
Fentanyl has a US DEA ACSCN of 9801 and a 2013 annual aggregate manufacturing quota of 2,108.75 kg, unchanged from the prior year.
Society and culture
Legal status
In the UK, fentanyl is classified as a controlled Class A drug under the Misuse of Drugs Act 1971.
In the Netherlands, fentanyl is a List I substance of the Opium Law.
In the U.S., fentanyl is a Schedule II controlled substance per the Controlled Substance Act. Distributors of Abstral are required to implement an FDA-approved risk evaluation and mitigation strategy (REMS) program. In order to curb misuse, many health insurers have begun to require precertification and/or quantity limits for Actiq prescriptions.
In Canada, fentanyl is considered a Schedule I drug as listed in Canada's Controlled Drugs and Substances Act.
Estonia in known to have been home to the world's longest documented fentanyl epidemic, especially following the Taliban ban on opium poppy cultivation in Afghanistan.
A 2018 report by The Guardian indicated that many major drug suppliers on the dark web have voluntarily banned the trafficking of fentanyl.
Recreational use
Illicit use of pharmaceutical fentanyl and its analogues first appeared in the mid-1970s in the medical community and continues in the present. More than 12 different analogues of fentanyl, all unapproved and clandestinely produced, have been identified in the U.S. drug traffic. In February 2018, the U.S. Drug Enforcement Administration indicated that illicit fentanyl analogs have no medically valid use, and thus applied a "Schedule I" classification to them.
Fentanyl analogues may be hundreds of times more potent than heroin. Fentanyl is used orally, smoked, snorted, or injected. Fentanyl is sometimes sold as heroin or oxycodone, sometimes leading to overdoses. Many fentanyl overdoses are initially classified as heroin overdoses. The recreational use is not particularly widespread in the EU with the exception of Tallinn, Estonia, where it has largely replaced heroin. Estonia has the highest rate of 3-methylfentanyl overdose deaths in the EU, due to its high rate of recreational use.
Fentanyl is sometimes sold on the black market in the form of transdermal fentanyl patches such as Duragesic, diverted from legitimate medical supplies. The gel from inside the patches is sometimes ingested or injected.
Another form of fentanyl that has appeared on the streets is the Actiq lollipop formulation. The pharmacy retail price ranges from US$15 to US$50 per unit based on the strength of the lozenge, with the black market cost ranging from US$5 to US$25, depending on the dose. The attorneys general of Connecticut and Pennsylvania have launched investigations into its diversion from the legitimate pharmaceutical market, including Cephalon's "sales and promotional practices for Provigil, Actiq and Gabitril".
Non-medical use of fentanyl by individuals without opiate tolerance can be very dangerous and has resulted in numerous deaths. Even those with opiate tolerances are at high risk for overdoses. Like all opioids, the effects of fentanyl can be reversed with naloxone, or other opiate antagonists. Naloxone is increasingly available to the public. Long acting or sustained release opioids may require repeat dosage. Illicitly synthesized fentanyl powder has also appeared on the United States market. Because of the extremely high strength of pure fentanyl powder, it is very difficult to dilute appropriately, and often the resulting mixture may be far too strong and, therefore, very dangerous.
Some heroin dealers mix fentanyl powder with heroin to increase potency or compensate for low-quality heroin. In 2006, illegally manufactured, non-pharmaceutical fentanyl often mixed with cocaine or heroin caused an outbreak of overdose deaths in the United States and Canada, heavily concentrated in the cities of Dayton, Ohio; Chicago; Detroit; and Philadelphia.
Enforcement
Several large quantities of illicitly produced fentanyl have been seized by U.S. law enforcement agencies. In November 2016, the DEA uncovered an operation making counterfeit oxycodone and Xanax from a home in Cottonwood Heights, Utah. They found about 70,000 pills in the appearance of oxycodone and more than 25,000 in the appearance of Xanax. The DEA reported that millions of pills could have been distributed from this location over the course of time. The accused owned a tablet press and ordered fentanyl in powder form from China. A seizure of a record amount of fentanyl occurred on February 2, 2019, by U.S. Customs and Border Protection in Nogales, Arizona. The 254 pounds (115 kg) of fentanyl, which was estimated to be worth US$3.5M, was concealed in a compartment under a false floor of a truck transporting cucumbers. The "China White" form of fentanyl refers to any of a number of clandestinely produced analogues, especially α-methylfentanyl (AMF). One US Department of Justice publication lists "China White" as a synonym for a number of fentanyl analogues, including 3-methylfentanyl and α-methylfentanyl, which today are classified as Schedule I drugs in the United States. Part of the motivation for AMF is that, despite the extra difficulty from a synthetic standpoint, the resultant drug is more resistant to metabolic degradation. This results in a drug with an increased duration.
In June 2013, the United States Centers for Disease Control and Prevention (CDC) issued a health advisory to emergency departments alerting to 14 overdose deaths among intravenous drug users in Rhode Island associated with acetylfentanyl, a synthetic opioid analog of fentanyl that has never been licensed for medical use. In a separate study conducted by the CDC, 82% of fentanyl overdose deaths involved illegally manufactured fentanyl, while only 4% were suspected to originate from a prescription.
Beginning in 2015, Canada has seen a number of fentanyl overdoses. Authorities suspected that the drug was being imported from Asia to the western coast by organized crime groups in powder form and being pressed into pseudo-OxyContin tablets. Traces of the drug have also been found in other recreational drugs including cocaine, MDMA, and heroin. The drug has been implicated in multiple deaths from the homeless to young professionals, including multiple teens and young parents. Because of the rising deaths across the country, especially in British Columbia where the deaths for 2016 is 668 and deaths for 2017 (January to October) is 999, Health Canada is putting a rush on a review of the prescription-only status of naloxone in an effort to combat overdoses of the drug.
Fentanyl has been discovered for sale in illicit markets in Australia in 2017 and in New Zealand in 2018. In response, New Zealand experts called for wider availability of naloxone.
Recalls
In February 2004, a leading fentanyl supplier, Janssen Pharmaceutica Products, L.P., recalled one lot, and later, additional lots of fentanyl (brand name: Duragesic) patches because of seal breaches which might have allowed the medication to leak from the patch. A series of Class II recalls was initiated in March 2004, and in February 2008 ALZA Corporation recalled their 25 µg/h Duragesic patches due to a concern that small cuts in the gel reservoir could result in accidental exposure of patients or health care providers to the fentanyl gel.
Brand names
Brand names include Sublimaze, Actiq, Durogesic, Duragesic, Fentora, Matrifen, Haldid, Onsolis, Instanyl, Abstral, Lazanda and others.
Cost
In the US, the 800 mcg tablet was 6.75 times more expensive as of 2020 than the lozenge.
Storage and disposal
The fentanyl patch is one of a few medications that may be especially harmful, and in some cases fatal, with just one dose, if used by someone other than the person for whom the medication was prescribed. Unused fentanyl patches should be kept in a secure location out of children's sight and reach, such as a locked cabinet.
In British Columbia, Canada where there are environmental concerns about toilet flushing or garbage disposal, pharmacists recommend that unused patches be sealed in a child-proof container which is then returned to a pharmacy. In the United States where patches cannot always be returned through a medication take-back program, flushing is recommended for fentanyl patches because it is the fastest and surest way to remove them from the home to prevent them from ingestion by children, pets or others not intended to use them.
Notable deaths
- Medical examiners concluded that musician Prince died on April 21, 2016, from an accidental fentanyl overdose. Fentanyl was among many substances identified in counterfeit pills recovered from his home, especially some that were mislabeled as Watson 385, a combination of hydrocodone and paracetamol.
- Author & journalist Michelle McNamara died on April 21, 2016, from an accidental overdose; medical examiners determined fentanyl was a contributing factor.
- American rapper Lil Peep died of an accidental fentanyl overdose on November 15, 2017.
- On January 19, 2018, the medical examiner-coroner for the county of Los Angeles said musician Tom Petty died from an accidental drug overdose as a result of mixing medications that included fentanyl, acetyl fentanyl and despropionyl fentanyl (among others). He was reportedly treating "many serious ailments" that included a broken hip.
- In 2018, American rapper Mac Miller died from an accidental overdose of fentanyl, cocaine and alcohol.
- On August 20, 2020, Justin Townes Earle died from an accidental overdose caused by cocaine laced with fentanyl.
State use
In August 2018, the United States used fentanyl for the first time to execute a prisoner. Carey Dean Moore, at the time one of the United States' longest-serving death row inmates, was executed at the Nebraska State Penitentiary. Moore received a lethal injection, administered as an intravenous series of four drugs that included fentanyl citrate to inhibit breathing and render the subject unconscious. The other drugs included diazepam as a tranquilizer, cisatracurium besylate as a muscle relaxant, and potassium chloride to stop the heart. The use of fentanyl in execution caused concern among death penalty experts because it was part of a previously untested drug cocktail. The execution was also protested by anti-death penalty advocates at the prison during the execution and later at the Nebraska capitol building.
Russian Spetsnaz security forces used a fentanyl analogue or derivative to incapacitate people rapidly in the Moscow theater hostage crisis in 2002. The siege was ended, but about 130 of the 850 hostages died from the gas. The Russian Health Minister later stated that the gas was based on fentanyl, but the exact chemical agent has not been identified.
Veterinary use
Fentanyl in injectable formulation is commonly used for analgesia and as a component of balanced sedation and general anesthesia in small animal patients. Its potency and short duration of action make it particularly useful in critically ill patients. In addition, it tends to cause less vomiting and regurgitation than other pure-opiate (codeine, morphine) and synthetic pure-opioid agonists (oxycodone, hydromorphone) when given as a continuous post-operative infusion. As with other pure-opioid agonists, fentanyl can be associated with dysphoria in both dogs and cats.
Transdermal fentanyl has also been used for many years in dogs and cats for post-operative analgesia. This is usually done with off-label fentanyl patches manufactured for humans with chronic pain. In 2012 a highly concentrated (50 mg/mL) transdermal solution, trade name Recuvyra, has become commercially available for dogs only. It is FDA approved to provide four days of analgesia after a single application prior to surgery. It is not approved for multiple doses or other species. The drug is also approved in Europe.







