| Nonsteroidal anti-inflammatory drug | |
|---|---|
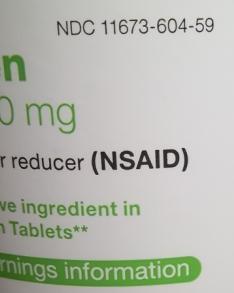
 Coated 200 mg tablets of generic ibuprofen, a common NSAID | |
| Class identifiers | |
| Pronunciation | /ˈɛnsɛd/ EN-sed |
| Synonyms | Cyclooxygenase inhibitor, Cyclooxygenase enzyme inhibitor, Nonsteroidal anti-inflammatory agents/analgesics (NSAIAs), Nonsteroidal anti-inflammatory medicines (NSAIMs) |
| Use | Pain, fever, Inflammation, Antithrombosis |
| ATC code | M01A |
| Mechanism of action | Enzyme inhibitor |
| Biological target | COX-1 and COX-2 |
Nonsteroidal anti-inflammatory drugs (NSAIDs) are members of a drug class that reduces pain, decreases fever, prevents blood clots, and in higher doses, decreases inflammation. Side effects depend on the specific drug but largely include an increased risk of gastrointestinal ulcers and bleeds, heart attack, and kidney disease.
The term nonsteroidal distinguishes these drugs from steroids, which while having a similar eicosanoid-depressing, anti-inflammatory action, have a broad range of other effects. First used in 1960, the term served to distance these medications from steroids, which were particularly stigmatised at the time due to the connotations with anabolic steroid abuse.
NSAIDs work by inhibiting the activity of cyclooxygenase enzymes (COX-1 or COX-2). In cells, these enzymes are involved in the synthesis of key biological mediators, namely prostaglandins, which are involved in inflammation, and thromboxanes, which are involved in blood clotting.
There are two types of NSAIDs available: non-selective and COX-2 selective. Most NSAIDs are non-selective and inhibit the activity of both COX-1 and COX-2. These NSAIDs, while reducing inflammation, also inhibit platelet aggregation (especially aspirin) and increase the risk of gastrointestinal ulcers/bleeds. COX-2 selective inhibitors have less gastrointestinal side effects but promote thrombosis and some of these agents substantially increase the risk of heart attack. As a result, certain older COX-2 selective inhibitors are no longer used due to the high risk of undiagnosed vascular disease. These differential effects are due to the different roles and tissue localisations of each COX isoenzyme. By inhibiting physiological COX activity, all NSAIDs increase the risk of kidney disease and through a related mechanism, heart attack. In addition, NSAIDs can blunt the production of erythropoietin resulting in anaemia, since haemoglobin needs this hormone to be produced. Prolonged use is dangerous and case studies have shown the health risk with celecoxib.
The most prominent NSAIDs are aspirin, ibuprofen, and naproxen, all available over the counter (OTC) in most countries. Paracetamol (acetaminophen) is generally not considered an NSAID because it has only minor anti-inflammatory activity. Acetaminophen treats pain mainly by blocking COX-2 and inhibiting endocannabinoid reuptake almost exclusively within the brain, but not much in the rest of the body.
Medical uses
NSAIDs are usually used for the treatment of acute or chronic conditions where pain and inflammation are present.
NSAIDs are generally used for the symptomatic relief of the following conditions:
- Osteoarthritis
- Rheumatoid arthritis
- Mild-to-moderate pain due to inflammation and tissue injury
- Low back pain
- Inflammatory arthropathies (e.g., ankylosing spondylitis, psoriatic arthritis, reactive arthritis)
- Tennis elbow
- Headache
- Migraine
- Acute gout
- Dysmenorrhea (menstrual pain)
- Metastatic bone pain
- Postoperative pain
- Muscle stiffness and pain due to Parkinson's disease
- Pyrexia (fever)
- Ileus
- Renal colic
- Macular edema
- Traumatic Injury
Aspirin, the only NSAID able to irreversibly inhibit COX-1, is also indicated for antithrombosis through inhibition of platelet aggregation. This is useful for the management of arterial thrombosis and prevention of adverse cardiovascular events like heart attacks. Aspirin inhibits platelet aggregation by inhibiting the action of thromboxane A2.
In a more specific application, the reduction in prostaglandins is used to close a patent ductus arteriosus in neonates if it has not done so physiologically after 24 hours.
NSAIDs are useful in the management of post-operative dental pain following invasive dental procedures such as dental extraction. When not contra-indicated they are favoured over the use of paracetamol alone due to the anti-inflammatory effect they provide. When used in combination with paracetamol the analgesic effect has been proven to be improved. There is weak evidence suggesting that taking pre-operative analgesia can reduce the length of post operative pain associated with placing orthodontic spacers under local anaesthetic. Combination of NSAIDs with pregabalin as preemptive analgesia has shown promising results for decreasing post operative pain intensity.
The effectiveness of NSAIDs for treating non-cancer chronic pain and cancer-related pain in children and adolescents is not clear. There have not been sufficient numbers of high-quality randomized controlled trials conducted.
Inflammation
Differences in anti-inflammatory activity between NSAIDs are small, but there is considerable variation in individual response and tolerance to these drugs. About 60% of patients will respond to any NSAID; of the others, those who do not respond to one may well respond to another. Pain relief starts soon after taking the first dose and a full analgesic effect should normally be obtained within a week, whereas an anti-inflammatory effect may not be achieved (or may not be clinically assessable) for up to 3 weeks. If appropriate responses are not obtained within these times, another NSAID should be tried.
Contraindications
NSAIDs may be used with caution by people with the following conditions:
- Irritable bowel syndrome
- Persons who are over age 50, and who have a family history of GI (gastrointestinal) problems
- Persons who have had past GI problems from NSAID use
NSAIDs should usually be avoided by people with the following conditions:
- Peptic ulcer or stomach bleeding
- Uncontrolled hypertension
- Kidney disease
- People that suffer with inflammatory bowel disease (Crohn's disease or ulcerative colitis)
- Past transient ischemic attack (excluding aspirin)
- Past stroke (excluding aspirin)
- Past myocardial infarction (excluding aspirin)
- Coronary artery disease (excluding aspirin)
- Undergoing coronary artery bypass surgery
- Congestive heart failure (excluding low-dose aspirin)
- In third trimester of pregnancy
- Persons who have undergone gastric bypass surgery
- Persons who have a history of allergic or allergic-type NSAID hypersensitivity reactions, e.g. aspirin-induced asthma
Adverse effects
The widespread use of NSAIDs has meant that the adverse effects of these drugs have become increasingly common. Use of NSAIDs increases risk of a range of gastrointestinal (GI) problems, kidney disease and adverse cardiovascular events. As commonly used for post-operative pain, there is evidence of increased risk of kidney complications. Their use following gastrointestinal surgery remains controversial, given mixed evidence of increased risk of leakage from any bowel anastomosis created.
An estimated 10–20% of people taking NSAIDs experience indigestion. In the 1990s high doses of prescription NSAIDs were associated with serious upper gastrointestinal adverse events, including bleeding. Over the past decade, deaths associated with gastric bleeding have declined.
NSAIDs, like all medications, may interact with other medications. For example, concurrent use of NSAIDs and quinolone antibiotics may increase the risk of quinolones' adverse central nervous system effects, including seizure.
There is an argument over the benefits and risks of NSAIDs for treating chronic musculoskeletal pain. Each drug has a benefit-risk profile and balancing the risk of no treatment with the competing potential risks of various therapies should be considered. For people over the age of 65 years old, the balance between the benefits of pain-relief medications such as NSAIDS and the potential for adverse effects has not been well determined.
In October 2020, the U.S. Food and Drug Administration (FDA) required the drug label to be updated for all nonsteroidal anti-inflammatory medications to describe the risk of kidney problems in unborn babies that result in low amniotic fluid. They are recommending avoiding NSAIDs in pregnant women at 20 weeks or later in pregnancy.
Combinational risk
If a COX-2 inhibitor is taken, a traditional NSAID (prescription or over-the-counter) should not be taken at the same time. In addition, people on daily aspirin therapy (e.g., for reducing cardiovascular risk) must be careful if they also use other NSAIDs, as these may inhibit the cardioprotective effects of aspirin.
Rofecoxib (Vioxx) was shown to produce significantly fewer gastrointestinal adverse drug reactions (ADRs) compared with naproxen. The study, the VIGOR trial, raised the issue of the cardiovascular safety of the coxibs. A statistically significant increase in the incidence of myocardial infarctions was observed in patients on rofecoxib. Further data, from the APPROVe trial, showed a statistically significant relative risk of cardiovascular events of 1.97 versus placebo—which caused a worldwide withdrawal of rofecoxib in October 2004.
Use of methotrexate together with NSAIDs in rheumatoid arthritis is safe, if adequate monitoring is done.
Cardiovascular
NSAIDs, aside from aspirin, increase the risk of myocardial infarction and stroke. This occurs at least within a week of use. They are not recommended in those who have had a previous heart attack as they increase the risk of death or recurrent MI. Evidence indicates that naproxen may be the least harmful out of these.
NSAIDs aside from (low-dose) aspirin are associated with a doubled risk of heart failure in people without a history of cardiac disease. In people with such a history, use of NSAIDs (aside from low-dose aspirin) was associated with a more than 10-fold increase in heart failure. If this link is proven causal, researchers estimate that NSAIDs would be responsible for up to 20 percent of hospital admissions for congestive heart failure. In people with heart failure, NSAIDs increase mortality risk (hazard ratio) by approximately 1.2–1.3 for naproxen and ibuprofen, 1.7 for rofecoxib and celecoxib, and 2.1 for diclofenac.
On 9 July 2015, the Food and Drug Administration (FDA) toughened warnings of increased heart attack and stroke risk associated with nonsteroidal anti-inflammatory drugs (NSAIDs) other than aspirin.
Possible erectile dysfunction risk
A 2005 Finnish survey study found an association between long term (over 3 months) use of NSAIDs and erectile dysfunction.
A 2011 publication in The Journal of Urology received widespread publicity. According to the study, men who used NSAIDs regularly were at significantly increased risk of erectile dysfunction. A link between NSAID use and erectile dysfunction still existed after controlling for several conditions. However, the study was observational and not controlled, with low original participation rate, potential participation bias, and other uncontrolled factors. The authors warned against drawing any conclusion regarding cause.
Gastrointestinal
The main adverse drug reactions (ADRs) associated with NSAID use relate to direct and indirect irritation of the gastrointestinal (GI) tract. NSAIDs cause a dual assault on the GI tract: the acidic molecules directly irritate the gastric mucosa, and inhibition of COX-1 and COX-2 reduces the levels of protective prostaglandins. Inhibition of prostaglandin synthesis in the GI tract causes increased gastric acid secretion, diminished bicarbonate secretion, diminished mucus secretion and diminished trophic effects on the epithelial mucosa.
Common gastrointestinal side effects include:
- Nausea or vomiting
- Indigestion
- Gastric ulceration or bleeding
- Diarrhea
Clinical NSAID ulcers are related to the systemic effects of NSAID administration. Such damage occurs irrespective of the route of administration of the NSAID (e.g., oral, rectal, or parenteral) and can occur even in people who have achlorhydria.
Ulceration risk increases with therapy duration, and with higher doses. To minimize GI side effects, it is prudent to use the lowest effective dose for the shortest period of time—a practice that studies show is often not followed. Over 50% of patients who take NSAIDs have sustained some mucosal damage to their small intestine.
The risk and rate of gastric adverse effects is different depending on the type of NSAID medication a person is taking. Indomethacin, ketoprofen, and piroxicam use appear to lead to the highest rate of gastric adverse effects, while ibuprofen (lower doses) and diclofenac appear to have lower rates.
Certain NSAIDs, such as aspirin, have been marketed in enteric-coated formulations that manufacturers claim reduce the incidence of gastrointestinal ADRs. Similarly, some believe that rectal formulations may reduce gastrointestinal ADRs. However, consistent with the systemic mechanism of such ADRs, and in clinical practice, these formulations have not demonstrated a reduced risk of GI ulceration.
Numerous "gastro-protective" drugs have been developed with the goal of preventing gastrointestinal toxicity in people who need to take NSAIDs on a regular basis. Gastric adverse effects may be reduced by taking medications that suppress acid production such as proton pump inhibitors (e.g.: omeprazole and esomeprazole), or by treatment with a drug that mimics prostaglandin in order to restore the lining of the GI tract (e.g.: a prostaglandin analog misoprostol). Diarrhea is a common side effect of misoprostol, however, higher doses of misoprostol have been shown to reduce the risk of a person having a complication related to a gastric ulcer while taking NSAIDs. While these techniques may be effective, they are expensive for maintenance therapy.
Hydrogen sulfide NSAID hybrids prevent the gastric ulceration/bleeding associated with taking the NSAIDs alone. Hydrogen sulfide is known to have a protective effect on the cardiovascular and gastrointestinal system.
Inflammatory bowel disease
NSAIDs should be used with caution in individuals with inflammatory bowel disease (e.g., Crohn's disease or ulcerative colitis) due to their tendency to cause gastric bleeding and form ulceration in the gastric lining.
Renal
NSAIDs are also associated with a fairly high incidence of adverse drug reactions (ADRs) on the kidney and over time can lead to chronic kidney disease. The mechanism of these kidney ADRs is due to changes in kidney blood flow. Prostaglandins normally dilate the afferent arterioles of the glomeruli. This helps maintain normal glomerular perfusion and glomerular filtration rate (GFR), an indicator of kidney function. This is particularly important in kidney failure where the kidney is trying to maintain renal perfusion pressure by elevated angiotensin II levels. At these elevated levels, angiotensin II also constricts the afferent arteriole into the glomerulus in addition to the efferent arteriole it normally constricts. Since NSAIDs block this prostaglandin-mediated effect of afferent arteriole dilation, particularly in kidney failure, NSAIDs cause unopposed constriction of the afferent arteriole and decreased RPF (renal perfusion flow) and GFR.
Common ADRs associated with altered kidney function include:
- Sodium and fluid retention
- Hypertension (high blood pressure)
These agents may also cause kidney impairment, especially in combination with other nephrotoxic agents. Kidney failure is especially a risk if the patient is also concomitantly taking an ACE inhibitor (which removes angiotensin II's vasoconstriction of the efferent arteriole) and a diuretic (which drops plasma volume, and thereby RPF)—the so-called "triple whammy" effect.
In rarer instances NSAIDs may also cause more severe kidney conditions:
- Interstitial nephritis
- Nephrotic syndrome
- Acute kidney injury
- Acute tubular necrosis
- Renal papillary necrosis
NSAIDs in combination with excessive use of phenacetin or paracetamol (acetaminophen) may lead to analgesic nephropathy.
Photosensitivity
Photosensitivity is a commonly overlooked adverse effect of many of the NSAIDs. The 2-arylpropionic acids are the most likely to produce photosensitivity reactions, but other NSAIDs have also been implicated including piroxicam, diclofenac, and benzydamine.
Benoxaprofen, since withdrawn due to its liver toxicity, was the most photoactive NSAID observed. The mechanism of photosensitivity, responsible for the high photoactivity of the 2-arylpropionic acids, is the ready decarboxylation of the carboxylic acid moiety. The specific absorbance characteristics of the different chromophoric 2-aryl substituents, affects the decarboxylation mechanism.
During pregnancy
NSAIDs are not recommended during pregnancy, particularly during the third trimester. While NSAIDs as a class are not direct teratogens, they may cause premature closure of the fetal ductus arteriosus and kidney ADRs in the fetus. Additionally, they are linked with premature birth and miscarriage. Aspirin, however, is used together with heparin in pregnant women with antiphospholipid syndrome. Additionally, indomethacin is used in pregnancy to treat polyhydramnios by reducing fetal urine production via inhibiting fetal kidney blood flow.
In contrast, paracetamol (acetaminophen) is regarded as being safe and well tolerated during pregnancy, but Leffers et al. released a study in 2010, indicating that there may be associated male infertility in the unborn. Doses should be taken as prescribed, due to risk of liver toxicity with overdoses.
In France, the country's health agency contraindicates the use of NSAIDs, including aspirin, after the sixth month of pregnancy.
In October 2020, the U.S. Food and Drug Administration (FDA) required the drug label to be updated for all nonsteroidal anti-inflammatory medications to describe the risk of kidney problems in unborn babies that result in low amniotic fluid. They are recommending avoiding NSAIDs in pregnant women at 20 weeks or later in pregnancy.
Allergy and allergy-like hypersensitivity reactions
A variety of allergic or allergic-like NSAID hypersensitivity reactions follow the ingestion of NSAIDs. These hypersensitivity reactions differ from the other adverse reactions listed here which are toxicity reactions, i.e. unwanted reactions that result from the pharmacological action of a drug, are dose-related, and can occur in any treated individual; hypersensitivity reactions are idiosyncratic reactions to a drug. Some NSAID hypersensitivity reactions are truly allergic in origin: 1) repetitive IgE-mediated urticarial skin eruptions, angioedema, and anaphylaxis following immediately to hours after ingesting one structural type of NSAID but not after ingesting structurally unrelated NSAIDs; and 2) Comparatively mild to moderately severe T cell-mediated delayed onset (usually more than 24 hour), skin reactions such as maculopapular rash, fixed drug eruptions, photosensitivity reactions, delayed urticaria, and contact dermatitis; or 3) far more severe and potentially life-threatening t-cell-mediated delayed systemic reactions such as the DRESS syndrome, acute generalized exanthematous pustulosis, the Stevens–Johnson syndrome, and toxic epidermal necrolysis. Other NSAID hypersensitivity reactions are allergy-like symptoms but do not involve true allergic mechanisms; rather, they appear due to the ability of NSAIDs to alter the metabolism of arachidonic acid in favor of forming metabolites that promote allergic symptoms. Afflicted individuals may be abnormally sensitive to these provocative metabolites or overproduce them and typically are susceptible to a wide range of structurally dissimilar NSAIDs, particularly those that inhibit COX1. Symptoms, which develop immediately to hours after ingesting any of various NSAIDs that inhibit COX-1, are: 1) exacerbations of asthmatic and rhinitis (see aspirin-induced asthma) symptoms in individuals with a history of asthma or rhinitis and 2) exacerbation or first-time development of wheals or angioedema in individuals with or without a history of chronic urticarial lesions or angioedema.
Possible effects on bone and soft tissue healing
It has been hypothesized that NSAIDs may delay healing from bone and soft-tissue injuries by inhibiting inflammation. On the other hand, it has also been hypothesized that NSAIDs might speed recovery from soft tissue injuries by preventing inflammatory processes from damaging adjacent, non-injured muscles.
There is moderate evidence that they delay bone healing. Their overall effect on soft-tissue healing is unclear.
Other
The use of NSAIDs for analgesia following gastrointestinal surgery remains controversial, given mixed evidence of an increased risk of leakage from any bowel anastomosis created. This risk may vary according to the class of NSAID prescribed.
Common adverse drug reactions (ADR), other than listed above, include: raised liver enzymes, headache, dizziness. Uncommon ADRs include an abnormally high level of potassium in the blood, confusion, spasm of the airways, and rash. Ibuprofen may also rarely cause irritable bowel syndrome symptoms. NSAIDs are also implicated in some cases of Stevens–Johnson syndrome.
Most NSAIDs penetrate poorly into the central nervous system (CNS). However, the COX enzymes are expressed constitutively in some areas of the CNS, meaning that even limited penetration may cause adverse effects such as somnolence and dizziness.
NSAIDs may increase the risk of bleeding in patients with Dengue fever For this reason, NSAIDs are only available with a prescription in India.
In very rare cases, ibuprofen can cause aseptic meningitis.
As with other drugs, allergies to NSAIDs might exist. While many allergies are specific to one NSAID, up to 1 in 5 people may have unpredictable cross-reactive allergic responses to other NSAIDs as well.
Drug interactions
NSAIDs reduce kidney blood flow and thereby decrease the efficacy of diuretics, and inhibit the elimination of lithium and methotrexate.
NSAIDs cause decreased ability to form blood clots, which can increase the risk of bleeding when combined with other drugs that also decrease blood clotting, such as warfarin.
NSAIDs may aggravate hypertension (high blood pressure) and thereby antagonize the effect of antihypertensives, such as ACE inhibitors.
NSAIDs may interfere and reduce efficiency of SSRI antidepressants. NSAIDs, when used in combination with SSRIs, increases the risk of adverse gastrointestinal effects. NSAIDs, when used in combination with SSRIs, increases the risk of internal bleeding and brain hemorrhages.
Various widely used nonsteroidal anti-inflammatory drugs (NSAIDs) enhance endocannabinoid signaling by blocking the anandamide-degrading membrane enzyme fatty acid amide hydrolase (FAAH).
NSAIDs may reduce the effectiveness of antibiotics. Tests on cultured bacteria found that antibiotic effectiveness was reduced by 18-30% on average compared to tests which did not include NSAIDs.
Immune response
Although small doses generally have little to no effect on the immune system, large doses of NSAIDs significantly suppress the production of immune cells. As NSAIDs affect prostaglandins, they affect the production of most fast growing cells. This includes immune cells. Unlike corticosteroids, they do not directly suppress the immune system and so their effect on the immune system is not immediately obvious. They suppress the production of new immune cells, but leave existing immune cells functional. Large doses slowly reduce the immune response as the immune cells are renewed at a much lower rate. Causing a gradual reduction of the immune system, much slower and less noticeable than the immediate effect of Corticosteroids. The effect significantly increases with dosage, in a nearly exponential rate. Doubling of dose reduced cells by nearly four times. Increasing dose by five times reduced cell counts to only a few percent of normal levels. This is likely why the effect was not immediately obvious in low dose trials, as the effect is not apparent until much higher dosages are tested.
Mechanism of action
Most NSAIDs act as nonselective inhibitors of the cyclooxygenase (COX) enzymes, inhibiting both the cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2) isoenzymes. This inhibition is competitively reversible (albeit at varying degrees of reversibility), as opposed to the mechanism of aspirin, which is irreversible inhibition. COX catalyzes the formation of prostaglandins and thromboxane from arachidonic acid (itself derived from the cellular phospholipid bilayer by phospholipase A2). Prostaglandins act (among other things) as messenger molecules in the process of inflammation. This mechanism of action was elucidated in 1970 by John Vane (1927–2004), who received a Nobel Prize for his work.
COX-1 is a constitutively expressed enzyme with a "house-keeping" role in regulating many normal physiological processes. One of these is in the stomach lining, where prostaglandins serve a protective role, preventing the stomach mucosa from being eroded by its own acid. COX-2 is an enzyme facultatively expressed in inflammation, and it is inhibition of COX-2 that produces the desirable effects of NSAIDs.
When nonselective COX-1/COX-2 inhibitors (such as aspirin, ibuprofen, and naproxen) lower stomach prostaglandin levels, ulcers of the stomach or duodenum and internal bleeding can result.
NSAIDs have been studied in various assays to understand how they affect each of these enzymes. While the assays reveal differences, unfortunately, different assays provide differing ratios.
The discovery of COX-2 led to research to the development of selective COX-2 inhibiting drugs that do not cause gastric problems characteristic of older NSAIDs.
Paracetamol (acetaminophen) is not considered an NSAID because it has little anti-inflammatory activity. It treats pain mainly by blocking COX-2 mostly in the central nervous system, but not much in the rest of the body.
However, many aspects of the mechanism of action of NSAIDs remain unexplained, and for this reason, further COX pathways are hypothesized. The COX-3 pathway was believed to fill some of this gap but recent findings make it appear unlikely that it plays any significant role in humans and alternative explanation models are proposed.
NSAIDs interact with the endocannabinoid system and its endocannabinoids, as COX2 have been shown to utilize endocannabinoids as substrates, and may have a key role in both the therapeutic effects and adverse effects of NSAIDs, as well as in NSAID-induced placebo responses.
NSAIDs are also used in the acute pain caused by gout because they inhibit urate crystal phagocytosis besides inhibition of prostaglandin synthase.
Antipyretic activity
NSAIDs have antipyretic activity and can be used to treat fever. Fever is caused by elevated levels of prostaglandin E2, which alters the firing rate of neurons within the hypothalamus that control thermoregulation. Antipyretics work by inhibiting the enzyme COX, which causes the general inhibition of prostanoid biosynthesis (PGE2) within the hypothalamus. PGE2 signals to the hypothalamus to increase the body's thermal setpoint. Ibuprofen has been shown more effective as an antipyretic than paracetamol (acetaminophen). Arachidonic acid is the precursor substrate for cyclooxygenase leading to the production of prostaglandins F, D, and E.