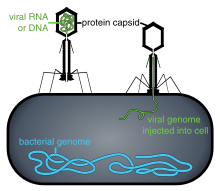
Phage therapy, viral phage therapy, or phagotherapy is the therapeutic use of bacteriophages to treat pathogenic bacterial infections. Bacteriophages, known as phages, are a form of virus. Phages attach to bacterial cells, and inject a viral genome into the cell. The viral genome effectively replaces the bacterial genome, halting the bacterial infection. The bacterial cell causing the infection is unable to reproduce, and instead produces additional phages. Phages are very selective in the strains of bacteria they are effective against. Advantages include reduced side-effects and reduced risk of the bacterium's developing resistance. Disadvantages include the difficulty of finding an effective phage for a particular infection. However, virulent phages can be isolated much more easily than other compounds and natural products. In addition to this, development of standardized manufacturing processes would make lab to clinic delivery of phages much quicker.
Phages are often compared to antibiotics. Phages tend to be more successful than antibiotics where there is a biofilm covered by a polysaccharide layer, which antibiotics typically cannot penetrate. Bacteriophages are much more specific than antibiotics. They are typically harmless not only to the host organism but also to other beneficial bacteria, such as the gut microbiota, reducing the chances of opportunistic infections. They have a high therapeutic index, that is, phage therapy would be expected to give rise to few side effects, even at higher-than-therapeutic levels. Because phages replicate in vivo (in cells of living organism), a smaller effective dose can be used.
This specificity is also a disadvantage: a phage will kill a bacterium only if it matches the specific strain. Consequently, phage mixtures ("cocktails") are often used to improve the chances of success. Alternatively, samples taken from recovering patients sometimes contain appropriate phages that can be grown to cure other patients infected with the same strain.
Phages are currently being used therapeutically to treat bacterial infections that do not respond to conventional antibiotics, particularly in Russia and Georgia. There is also a phage therapy unit in Wrocław, Poland, established in 2005, which continues several decades long research of the Institute of Immunology and Experimental Therapy of the Polish Academy of Sciences, the only such centre in a European Union country. Phages are the subject of renewed clinical attention in western countries, such as the United States. In 2019, the United States Food and Drug Administration approved the first US clinical trial for intravenous phage therapy.
Phage therapy has many potential applications in human medicine as well as dentistry, veterinary science, and agriculture. If the target host of a phage therapy treatment is not an animal, the term "biocontrol" (as in phage-mediated biocontrol of bacteria) is usually employed, rather than "phage therapy".
History
The discovery of bacteriophages was reported by British bacteriologist Frederick Twort in 1915, and by French-Canadian microbiologist Felix d'Hérelle in 1917. D'Hérelle said that the phages always appeared in the stools of Shigella dysentery patients shortly before they began to recover. He "quickly learned that bacteriophages are found wherever bacteria thrive: in sewers, in rivers that catch waste runoff from pipes, and in the stools of convalescent patients". Phage therapy was immediately recognized by many to be a key way forward for the eradication of pathogenic bacterial infections. A Georgian, George Eliava, was making similar discoveries. He travelled to the Pasteur Institute in Paris where he met d'Hérelle, and in 1923 he founded the Eliava Institute in Tbilisi, Georgia, devoted to the development of phage therapy. Phage therapy is used in Russia, Georgia and Poland, and was used prophylactically for a time in the Soviet army.
In Russia, extensive research and development soon began in this field. In the United States during the 1940s commercialization of phage therapy was undertaken by Eli Lilly and Company.
While knowledge was being accumulated regarding the biology of phages and how to use phage cocktails correctly, early uses of phage therapy were often unreliable. Since the early 20th century, research into the development of viable therapeutic antibiotics had also been underway, and by 1942 the antibiotic penicillin G had been successfully purified and saw use during the Second World War. The drug proved to be extraordinarily effective in the treatment of injured Allied soldiers whose wounds had become infected. By 1944, large-scale production of Penicillin had been made possible, and in 1945 it became publicly available in pharmacies. Due to the drug's success, it was marketed widely in the U.S. and Europe, leading Western scientists to mostly lose interest in further use and study of phage therapy for some time.
Isolated from Western advances in antibiotic production in the 1940s, Russian scientists continued to develop already successful phage therapy to treat the wounds of soldiers in field hospitals. During World War II, the Soviet Union used bacteriophages to treat many soldiers infected with various bacterial diseases e.g. dysentery and gangrene. Russian researchers continued to develop and to refine their treatments and to publish their research and results. However, due to the scientific barriers of the Cold War, this knowledge was not translated and did not proliferate across the world. A summary of these publications was published in English in 2009 in "A Literature Review of the Practical Application of Bacteriophage Research".
There is an extensive library and research center at the George Eliava Institute in Tbilisi, Georgia. Phage therapy is today a widespread form of treatment in that region.
As a result of the development of antibiotic resistance since the 1950s and an advancement of scientific knowledge, there has been renewed interest worldwide in the ability of phage therapy to eradicate bacterial infections and chronic polymicrobial biofilm (including in industrial situations).
Phages have been investigated as a potential means to eliminate pathogens like Campylobacter in raw food and Listeria in fresh food or to reduce food spoilage bacteria. In agricultural practice phages were used to fight pathogens like Campylobacter, Escherichia and Salmonella in farm animals, Lactococcus and Vibrio pathogens in fish from aquaculture and Erwinia, Xanthomonas, and others in plants of agricultural importance. The oldest use was, however, in human medicine. Phages have been used against diarrheal diseases caused by E. coli, Shigella or Vibrio and against wound infections caused by facultative pathogens of the skin like staphylococci and streptococci. Recently the phage therapy approach has been applied to systemic and even intracellular infections and the addition of non-replicating phage and isolated phage enzymes like lysins to the antimicrobial arsenal. However, actual proof for the efficacy of these phage approaches in the field or the hospital is not available.
Some of the interest in the West can be traced back to 1994, when Soothill demonstrated (in an animal model) that the use of phages could improve the success of skin grafts by reducing the underlying Pseudomonas aeruginosa infection. Recent studies have provided additional support for these findings in the model system.
Although not "phage therapy" in the original sense, the use of phages as delivery mechanisms for traditional antibiotics constitutes another possible therapeutic use. The use of phages to deliver antitumor agents has also been described in preliminary in vitro experiments for cells in tissue culture.
In June 2015 the European Medicines Agency hosted a one-day workshop on the therapeutic use of bacteriophages and in July 2015 the National Institutes of Health (US) hosted a two-day workshop "Bacteriophage Therapy: An Alternative Strategy to Combat Drug Resistance".
In January 2016, Phages were used successfully at Yale University by Benjamin Chan to treat a chronic Pseudomonas aeruginosa infection in ophthalmologist Ali Asghar Khodadoust. This successful treatment of a life threatening infection sparked a resurgence of interest in phage therapy in the United States.
In 2017, a pair of genetically engineered phages along with one naturally occurring (so-called "phage Muddy") each from among those catalogued by Science Education Alliance-Phages Hunters Advancing Genomics and Evolutionary Science (SEA-PHAGES) at the Howard Hughes Medical Institute by Graham Hatfull and colleagues, was used by microbiologist James Soothill at Great Ormond Street Hospital for Children in London to treat an antibiotic-resistant bacterial (Mycobacterium abscessus) infection in a young woman with cystic fibrosis.
Potential benefits
Bacteriophage treatment offers a possible alternative to conventional antibiotic treatments for bacterial infection. It is conceivable that, although bacteria can develop resistance to phages, the resistance might be easier to overcome than resistance to antibiotics. Just as bacteria can evolve resistance, viruses can evolve to overcome resistance.
Bacteriophages are very specific, targeting only one or a few strains of bacteria. Traditional antibiotics have a more wide-ranging effect, killing both harmful bacteria and useful bacteria such as those facilitating food digestion. The species and strain specificity of bacteriophages makes it unlikely that harmless or useful bacteria will be killed when fighting an infection.
A few research groups in the West are engineering a broader spectrum phage, and also a variety of forms of MRSA treatments, including impregnated wound dressings, preventative treatment for burn victims, phage-impregnated sutures. Enzybiotics are a new development at Rockefeller University that create enzymes from phage. Purified recombinant phage enzymes can be used as separate antibacterial agents in their own right.
Phage therapy also has the potential of preventing or treating infectious diseases of corals. This could assist with decline of coral around the world.
Application
Collection
The simplest method of phage treatment involves collecting local samples of water likely to contain high quantities of bacteria and bacteriophages, for example effluent outlets, sewage and other sources. The samples are taken and applied to the bacteria that are to be destroyed which have been cultured on growth medium.
If the bacteria die, as usually happens, the mixture is centrifuged; the phages collect on the top of the mixture and can be drawn off.
The phage solutions are then tested to see which ones show growth suppression effects (lysogeny) or destruction (lysis) of the target bacteria. The phage showing lysis is then amplified on cultures of the target bacteria, passed through a filter to remove all but the phages, then distributed.
Treatment
Phages are "bacterium-specific" and it is, therefore, necessary in many cases to take a swab from the patient and culture it prior to treatment. Occasionally, isolation of therapeutic phages can require a few months to complete, but clinics generally keep supplies of phage cocktails for the most common bacterial strains in a geographical area.
Phage cocktails are sold in pharmacies in eastern countries. The composition of bacteriophagic cocktails has been periodically modified to add phages effective against emerging pathogenic strains.
Phages in practice are applied orally, topically on infected wounds or spread onto surfaces, or used during surgical procedures. Injection is rarely used, avoiding any risks of trace chemical contaminants that may be present from the bacteria amplification stage, and recognizing that the immune system naturally fights against viruses introduced into the bloodstream or lymphatic system.
Individualised phage therapy was successfully used by Robert T. Schooley and others to treat a case of multi-drug-resistant Acinetobacter baumannii in the U.S. in 2015. Reviews of phage therapy indicate that more clinical and microbiological research is needed to meet current standards.
Clinical trials
Funding for phage therapy research and clinical trials is generally insufficient and difficult to obtain, since it is a lengthy and complex process to patent bacteriophage products. Scientists comment that 'the biggest hurdle is regulatory', whereas an official view is that individual phages would need proof individually because it would be too complicated to do as a combination, with many variables. Due to the specificity of phages, phage therapy would be most effective with a cocktail injection, which is generally rejected by the U.S. Food and Drug Administration (FDA). Researchers and observers predict that for phage therapy to be successful the FDA must change its regulatory stance on combination drug cocktails. Public awareness and education about phage therapy are generally limited to scientific or independent research rather than mainstream media.
In 2007 a Phase 1/2 clinical trial was completed at the Royal National Throat, Nose and Ear Hospital, London, for Pseudomonas aeruginosa infections (otitis). Documentation of the Phase-1/Phase-2 study was published in August 2009 in the journal Clinical Otolaryngology. Phase 1 clinical trials have now been completed in the Southwest Regional Wound Care Center, Lubbock, Texas for an approved cocktail of phages against bacteria, including P. aeruginosa, Staphylococcus aureus and Escherichia coli (E. coli). The cocktail of phages for the clinical trials was developed and supplied by Intralytix. PhagoBurn, a phase 1/2 trial of phage therapy against P. aeruginosa wound infection in France and Belgium in 2015–17, was terminated early because the phage therapy was not effective.
In July 2020, the FDA approved the first clinical trial of nebulized phage therapy in the United States. This double blind, placebo controlled study at Yale University will be focused on treating Pseudomonas aeruginosa infections in those with Cystic Fibrosis.
Locus Biosciences created a cocktail of three CRISPR modified phages. The study in 2019 of 30 patients will look at the reduction of E. coli in their urinary tracts. Twenty patients will get a phage cocktail, and 10 will get a placebo.
In February 2019, the FDA approved the first clinical trial of intravenously administered phage therapy in the United States.
Administration
Phages can usually be freeze-dried and turned into pills without materially reducing efficiency. Temperature stability up to 55 °C and shelf lives of 14 months have been shown for some types of phages in pill form.
Application in liquid form is possible, stored preferably in refrigerated vials.
Oral administration works better when an antacid is included, as this increases the number of phages surviving passage through the stomach.
Topical administration often involves application to gauzes that are laid on the area to be treated.
Phages were used successfully at Yale University by Benjamin Chan to treat a Pseudomonas infection in 2016.
IV phage drip therapy was successfully used to treat a patient with MDR Acinetobacter baumannii in Thornton Hospital at UC San Diego in 2017.
Nebulized phage therapy has been used successfully to treat numerous patients with Cystic fibrosis and Multidrug-resistant bacteria at Yale University as part of their compassionate use program.
In 2019, a Brownsville, MN man with a long-standing bacterial infection in his knee received a phage treatment at the Mayo Clinic which successfully killed the bacteria and avoided planned amputation of his lower leg.
Obstacles
The high bacterial strain specificity of phage therapy may make it necessary for clinics to make different cocktails for treatment of the same infection or disease because the bacterial components of such diseases may differ from region to region or even person to person. In addition, this means that "banks" containing many different phages must be kept and regularly updated with new phages.
Further, bacteria can evolve different receptors either before or during treatment. This can prevent phages from completely eradicating bacteria.
The need for banks of phages makes regulatory testing for safety harder and more expensive under current rules in most countries. Such a process would make the large-scale use of phage therapy difficult. Additionally, patent issues (specifically on living organisms) may complicate distribution for pharmaceutical companies wishing to have exclusive rights over their "invention", which would discourage a commercial corporation from investing capital in this.
As has been known for at least thirty years, mycobacteria such as Mycobacterium tuberculosis have specific bacteriophages. No lytic phage has yet been discovered for Clostridium difficile, which is responsible for many nosocomial diseases, but some temperate phages (integrated in the genome, also called lysogenic) are known for this species; this opens encouraging avenues but with additional risks as discussed below.
The negative public perception of viruses may also play a role in the reluctance to embrace phage therapy.
Legislation
Approval of phage therapy for use in humans has not been given in Western countries with a few exceptions. In the United States, Washington and Oregon law allows naturopathic physicians to use any therapy that is legal any place in the world on an experimental basis, and in Texas phages are considered natural substances and can be used in addition to (but not as a replacement for) traditional therapy (they have been used routinely in a wound care clinic in Lubbock, TX, since 2006).
In 2013, "the 20th biennial Evergreen International Phage Meeting ... conference drew 170 participants from 35 countries, including leaders of companies and institutes involved with human phage therapies from France, Australia, Georgia, Poland and the United States."
Safety
Much of the difficulty in obtaining regulatory approval is proving to be the risks of using a self-replicating entity which has the capability to evolve.
As with antibiotic therapy and other methods of countering bacterial infections, endotoxins are released by the bacteria as they are destroyed within the patient (Jarisch–Herxheimer reaction). This can cause symptoms of fever; in extreme cases toxic shock (a problem also seen with antibiotics) is possible. Janakiraman Ramachandran argues that this complication can be avoided in those types of infection where this reaction is likely to occur by using genetically engineered bacteriophages which have had their gene responsible for producing endolysin removed. Without this gene, the host bacterium still dies but remains intact because the lysis is disabled. On the other hand, this modification stops the exponential growth of phages, so one administered phage means one dead bacterial cell. Eventually these dead cells are consumed by the normal house-cleaning duties of the phagocytes, which utilize enzymes to break down the whole bacterium and its contents into harmless proteins, polysaccharides and lipids.
Temperate (or Lysogenic) bacteriophages are not generally used therapeutically, as this group can act as a way for bacteria to exchange DNA; this can help spread antibiotic resistance or even, theoretically, make the bacteria pathogenic (see Cholera). Carl Merril claimed that harmless strains of corynebacterium may have been converted into C. diphtheriae that "probably killed a third of all Europeans who came to North America in the seventeenth century". Fortunately, many phages seem to be lytic only with negligible probability of becoming lysogenic.
Other animals
Brigham Young University has been researching the use of phage therapy to treat American foulbrood in honeybees. Phage therapy is also being investigated for potential applications in aquaculture.
Cultural impact
The 1925 novel and 1926 Pulitzer prize winner Arrowsmith used phage therapy as a plot point.
Greg Bear's 2002 novel Vitals features phage therapy, based on Soviet research, used to transfer genetic material.
The 2012 collection of military history essays about the changing role of women in warfare, "Women in War – from home front to front line" includes a chapter featuring phage therapy: "Chapter 17: Women who thawed the Cold War".
Steffanie A. Strathdee's 2019 book The Perfect Predator: An Epidemiologist’s Journey to Save Her Husband from a Deadly Superbug, co-written with her husband Thomas Patterson, was published by Hachette Book Group in 2019. It describes Dr Strathdee's ultimately successful attempt to introduce phage therapy as a life-saving treatment for her husband, critically ill with a completely antibiotic-resistant Acinetobacter baumannii infection following severe pancreatitis.