| Deep brain stimulation | |
|---|---|
 |
Deep brain stimulation (DBS) is a surgical procedure that implants a neurostimulator and electrodes which sends electrical impulses to specified targets in the brain responsible for movement control. The treatment is designed for a range of movement disorders such as Parkinson's disease, essential tremor, and dystonia, as well as for certain neuropsychiatric conditions like obsessive-compulsive disorder (OCD) and epilepsy. The exact mechanisms of DBS are complex and not entirely clear, but it is known to modify brain activity in a structured way.
DBS has been approved by the Food and Drug Administration as a treatment for essential and Parkinsonian tremor and since 1997, and for Parkinson's disease (PD) since 2002. DBS was approved as humanitarian device excemptions for dystonia in 2003, obsessive–compulsive disorder (OCD) in 2009, and approved for epilepsy in 2018. DBS has been studied in clinical trials as a potential treatment for chronic pain, for various affective disorders, including major depression, for Alzheimer's Disease and drug addiction, among other brain disorders. It is one of few neurosurgical procedures that allow blinded studies.
As a first approximation, DBS is thought to mimic the clinical effects of lesioning, likely by attenuating (pathologically elevated) information flow through affected brain networks. Thus, DBS is thought to create an 'informational lesion', which can be switched off by turning off the DBS device, i.e. is largely reversible. This is a strong advantage compared to permanent brain lesions that are also applied to similar targets in similar conditions in the field of ablative stereotactic surgery.
Medical use


DBS is FDA approved or has FDA device exemptions for treatment of Parkinson's Disease, dystonia, Essential Tremor, obsessive-compulsive disorder and epilepsy. In Europe, beyond these indications, a CE mark exists for treatment of Alzheimer's Disease, and while there had been a device exemption for OCD, as well, this has not been renewed. All other indications are considered investigational, i.e. carried out within medical studies under IRB approval. The table below summarizes FDA approvals.
| Indication | Approval Date | Details | DBS Target | Evidence | Source |
|---|---|---|---|---|---|
| Essential Tremor (or Parkinsonian Tremor) | July 31, 1997 | The FDA approved DBS for the suppression of tremor in the upper extremity in patients with essential tremor. | Ventral intermediate nucleus of the thalamus (VIM) | The approval was based on clinical trials showing significant tremor reduction with thalamic DBS in patients with essential tremor, demonstrating long-term efficacy and safety. The key study is. | FDA |
| Parkinson's Disease | January 14, 2002 | Approved for advanced Parkinson’s disease symptoms not adequately controlled by medications. | Subthalamic nucleus (STN) or internal globus pallidus (GPi) | The key trial that led to approval is. Further large-scale randomized controlled trials such as, demonstrated the superiority of DBS in the subthalamic nucleus compared to best medical therapy, improving motor function and quality of life. | FDA |
| Dystonia | April 15, 2003 | Granted under a Humanitarian Device Exemption (HDE) for the treatment of chronic, intractable primary dystonia, including generalized and segmental dystonia, hemidystonia, and cervical dystonia in patients seven years of age or above. | Internal globus pallidus (GPi) | The key evidence came from smaller clinical trials under the Humanitarian Device Exemption, where DBS significantly improved motor function in patients with primary dystonia. Prominent trials include. | FDA |
| Obsessive-Compulsive Disorder | February 19, 2009 | Approved under HDE for adjunctive treatment of severe, treatment-resistant OCD. | Nucleus Accumbens (NAc) | Initial approval came under HDE based on evidence from smaller, open-label trials, such as, showing reductions in OCD symptoms in severe cases. | FDA |
| Epilepsy | April 27, 2018 | Approved for bilateral stimulation of the anterior nucleus of the thalamus (ANT) as an adjunctive therapy to reduce the frequency of seizures in adults with partial-onset seizures. | Anterior nucleus of the thalamus (ANT) | The key evidence came from the SANTE trial, demonstrating a significant reduction in seizure frequency in patients receiving DBS. | FDA |
Parkinson's disease
DBS is used to manage some of the symptoms of Parkinson's disease that cannot be adequately controlled with medications. PD is treated by applying high-frequency (> 100 Hz) stimulation to target structures in the depth of the brain. Frequently used targets include the subthalamic nucleus (STN), internal pallidum (GPi) and ventrointermediate nucleus of the thalamus (VIM). The pedunculopontine nucleus has been used as an investigational target to treat freezing of gait.
DBS is recommended for people who have PD with motor fluctuations and tremors inadequately controlled by medication, or to those who are intolerant to medication, as long as they do not have severe neuropsychiatric problems. Four areas of the brain have been treated with neural stimulators in PD. Most DBS surgeries in routine practice target either the GPi or the STN, which, in prospective trials have been equally efficient in reducing motor symptoms, likely due to a shared network being stimulated with either target. General differences between targets are not easy to summarize, but often include the following:
- DBS of the GPi has been shown to reduce uncontrollable movements called dyskinesias. This may sometimes allow a patient to take adequate (additional) quantities of medications (especially levodopa), thus leading to better control of symptoms.
- DBS of the subthalamic nucleus has a more sudden effect on tremor (while effect on tremor in GPi is sometimes delayed). Also, studies associated STN-DBS with reductions in dopaminergic medication.
- DBS of the VIM is mainly used to reduce shaking movements (tremor), and hence is, if at all, used in tremor-dominant variants of PD (and also to treat Essential Tremor).
- Some studies suggested efficacy for DBS of the PPN in reducing freezing of gait, but results have been mixed and the target is not routinely used.
Selection of the correct DBS target is a complicated process. Multiple clinical characteristics are used to select the target including – identifying the most troublesome symptoms, the dose of levodopa that the patient is currently taking, the effects and side-effects of current medications and concurrent problems. Decisions are often made in multidisciplinary teams at specialized institutions.
Essential Tremor
ET is a neurological condition characterized by involuntary and rhythmic shaking and the most common movement disorder. ET was the first indication to be approved for DBS (alongside Parkinsonian tremor) and before DBS had a long history of being treated with ablative brain lesioning. Already in the first publication on the matter by the team of Alim Louis Benabid, it could be shown that frequencies above 100 Hz are most effective for cessation of tremor, while lower frequencies have less effect. In clinical practice, frequencies between 80 and 180 Hz are typically applied. DBS electrodes commonly target the ventrointermediate nucleus of the thalamus (VIM) or ventrally adjacent areas that have been referred to as parts of the zona incerta, or posterior thalamic area. Recent metaanalytical evidence suggests that multiple targets along the circuitry of the cerebellothalamic pathway (also referred to as the dentatorubrothalamic or dentatothalamic tract) are similarly effective, i.e. modulating the cerebellar inflows into the thalamus may be key for therapeutic efficacy, for a review see. Despite its success, DBS for ET is not without side effects, which can include speech difficulties and paresthesia. Similar if not the same surgical targets have been applied to treat ET using surgical lesioning in both historical but also modern context, for instance using MR-guided Focused Ultrasound, Gamma-Knife Radiosurgery or conventional radiofrequency lesioning. For instance, the annual volume of MRgFUS thalamotomies has recently overtaken the volume of DBS cases to treat ET.
Dystonia
DBS is also an established therapeutic option for individuals with dystonia, a movement disorder characterized by sustained or repetitive muscle contractions, resulting in abnormal postures and involuntary movements. DBS is effective in treating primary generalized dystonia, and also used for focal dystonias such as cervical dystonia and task-specific dystonias (e.g., writer’s cramp). In dystonia, marked effects can be reached by targeting the GPi using high frequency DBS, with large randomized trials demonstrating improvements of ~45% and significant improvements in quality of life within the first six months of treatment. Similar effects have been reported in open label trials that targeted the STN (but this target is investigational for dystonia). In contrast to some symptoms in Parkinson's Disease or Essential Tremor, improvements in dystonia are often described to appear over weeks to months. This delayed response is thought to reflect the complexity of motor circuits involved in dystonia and the long-term plastic changes required for symptom relief. Despite the slower onset, many patients experience lasting and meaningful reductions in dystonia-related disability. DBS for dystonia is generally considered safe, but like all neuromodulation therapies, it comes with potential risks, including infection, hardware complications, or stimulation-related side effects such as speech difficulties. Ongoing research aims to optimize DBS targeting and stimulation settings to enhance outcomes for individuals with different types of dystonia. Recent large-scale mapping efforts have suggested slightly different optimal target sites for various forms of dystonia, such as generalized vs. cervical or appendicular vs. axial phenotypes of the disorder, potentially due to differing parts of the motor system being involved in different forms. In an attempt to develop physiomarkers that could guide adaptive forms of deep brain stimulation, researchers have identified elevated synchrony in the theta band to be associated with symptom severity, which was found maximally expressed at optimal stimulation sites within the GPi.
Obsessive-Compulsive-Disorder
DBS for OCD was first attempted by the team of Bart Nuttin in 1999. Curiously, the year 1999 marked three innovations all published in the Lancet: The first attempt to treat Tourette's Syndrome by the team of Veerle Visser-Vandewalle, the aforementioned trial by Nuttin and a trial reporting on bilateral stimulation of dystonia by Joachim Krauss and colleagues. Of these, the study by Visser-Vandewalle is considered the first modern-day indication of DBS in neuropsychiatric indication (Tourette's Syndrome), making the trial by Nuttin for OCD the second. DBS for OCD received a humanitarian device exemption from the FDA in 2009. In Europe, the CE Mark for Deep Brain Stimulation (DBS) for Obsessive-Compulsive Disorder (OCD) was active from 2009 to 2022 but not renewed thereafter, which was likely not motivated by a lack of evidence but by a lack of monetary interests, which has led to expert letters calling for a 'crisis of access' above and beyond Europe.
Beyond the original target in the anterior limb of the internal capsule (ALIC), multiple target sites have been probed, such as the nucleus accumbens (sometimes subsumized with the ALIC as the ventral capsule/ventral striatum or VC/VS target), the bed nucleus of stria terminalis, the inferior thalamic peduncle and the anteromedial portion of the STN. Within the ALIC region, large probabilistic mapping trials have identified two distinct sites of maximum efficacy, one likely corresponding to 'hyperdirect' pathway inputs to the subthalamic nucleus and other midbrain regions, the other potentially corresponding to 'indirect' pathway projections within the same basal ganglia thalamocortical loop. A potential circuit structure that seems to combine most effective targets in both the ALIC and STN region has been identified and termed the OCD response tract by the group of Andreas Horn. Modulating this fiber tract system, which has been described as projections from dorsal anterior cingulate and ventrolateral prefrontal cortices to the subthalamic nucleus (and potentially other midbrain structures), as well as reciprocal thalamic projections to the same sites, has been robustly associated with optimal treatment response across multiple studies from various groups. In an attempt to develop physiomarkers that could guide adaptive forms of deep brain stimulation, researchers have thus far identified mixed evidence, such as elevated delta activity to negatively correlate with OCD symptoms or elevated alpha activity to positively correlate with OCD symptoms. In 2024, Provenza et al. analyzed a larger cohort of 12 individuals implanted to the same target and confirmed and extended this latter finding: Elevated theta/alpha power (9 Hz) correlated with most symptomatic states. Curiously, they were expressed in a strong circadian pattern that allowed a high degree of predictability.
Epilepsy
As many as 36.3% of epilepsy patients are drug-resistant, i.e. may not be sufficiently treated with medication alone. These patients are at risk for significant morbidity and mortality including sudden unexpected death in epilepsy (SUDEP). If a seizure focus (i.e. seizure onset zone) can be determined (using MRI and/or invasive stereo-EEG recordings) resective brain surgery that involves removing brain tissue with the ictal focus is generally preferred, since this may potentially lead to a curative outcome (i.e. a state where no seizures happen anymore). In cases where resective surgery is not an option, other neurosurgical options such as responsive neurostimulation (RNS), DBS, or vagus nerve stimulation may be considered. While RNS is a method that includes brain sensing and brain stimulation, i.e. represents a form of adaptive deep brain stimulation, classical forms of DBS are also applied, typically at the standard 130 Hz frequency. The anterior nucleus of the thalamus (ANT) is the most commonly targeted area in DBS for epilepsy and the only FDA approved target site (see above). This multicenter, randomized, controlled SANTE trial (Stimulation of the Anterior Nucleus of the Thalamus for Epilepsy) demonstrated that DBS targeting the ANT significantly reduced seizure frequency in patients with medically refractory epilepsy. Over time, patients experienced sustained seizure reductions, with some achieving more than a 50% decrease in seizures. The SANTE trial has been a pivotal study, leading to the approval of ANT-DBS for epilepsy in many countries. This region plays a key role in the network of structures that propagate seizure activity.
Beyond the ANT, several other brain regions have been explored as potential DBS targets for epilepsy. These include:
- Centromedian nucleus (CM): Located in the thalamus, CM-DBS has been used in some cases of generalized epilepsy, including Lennox-Gastaut syndrome. It targets the thalamocortical networks involved in seizure propagation and has been reported to help reduce seizure severity and frequency.
- Hippocampus: Particularly in patients with temporal lobe epilepsy, hippocampal DBS has been investigated as an option due to its role in seizure propagation and memory function. Studies have generally shown promising results, particularly for temporal lobe seizures.
- Subthalamic nucleus (STN): Commonly used in Parkinson’s disease, the STN has also been explored as a target for epilepsy due to its involvement in motor control and seizure modulation. Initial studies have shown seizure reduction, especially in patients with focal epilepsy.
- Cerebellum: DBS of the cerebellum has been studied as a way to influence the modulation of neural circuits involved in epilepsy, although its use remains experimental.
Tourette syndrome
As mentioned above, the first DBS application for Tourette's Syndrome has been carried out by the team of Veerle Visser-Vandewalle in 1999. Building upon the ablative lesion cases carried out by Rolf Hassler and colleagues, Visser-Vandewalle chose the intersection between the centromedian, parafascicular and ventrooralis internus nuclei of the thalamus as her DBS target. Authors reported that, after surgery, tics disappeared and "a change in the patient’s character occurred in that he had become much more kind-hearted." DBS has been used experimentally in treating adults with severe Tourette syndrome who do not respond to conventional treatment. Despite widely publicized early successes, DBS remains a highly experimental procedure for treating Tourette's, and more study is needed to determine whether long-term benefits outweigh the risks. The procedure is well tolerated, but complications include "short battery life, abrupt symptom worsening upon cessation of stimulation, hypomanic or manic conversion, and the significant time and effort involved in optimizing stimulation parameters".
The procedure is invasive and expensive and requires long-term expert care. Benefits for severe Tourette's are inconclusive, considering the less robust effects of this surgery seen in the Netherlands. Tourette's is more common in pediatric populations, tending to remit in adulthood, so, in general, this would not be a recommended procedure for use on children. It may not always be obvious how to utilize DBS for a particular person because the diagnosis of Tourette's is based on a history of symptoms rather than an examination of neurological activity. Due to concern over the use of DBS in Tourette syndrome treatment, the Tourette Association of America convened a group of experts to develop recommendations guiding the use and potential clinical trials of DBS for TS.
Robertson reported that DBS had been used on 55 adults by 2011, remained an experimental treatment at that time, and recommended that the procedure "should only be conducted by experienced functional neurosurgeons operating in centres which also have a dedicated Tourette syndrome clinic". According to Malone et al. (2006), "Only patients with severe, debilitating, and treatment-refractory illness should be considered; while those with severe personality disorders and substance-abuse problems should be excluded." Du et al. (2010) say, "As an invasive therapy, DBS is currently only advisable for severely affected, treatment-refractory TS adults". Singer (2011) says, "pending determination of patient selection criteria and the outcome of carefully controlled clinical trials, a cautious approach is recommended". Viswanathan et al. (2012) say DBS should be used for people with "severe functional impairment that cannot be managed medically".
Major Depression
DBS has also been under investigational use for patients with treatment-resistant major depressive disorder (TRD), a condition in which individuals do not adequately respond to conventional therapies such as medication or psychotherapy. Following early endeavors of electrical brain stimulation starting in the 1950ies, the era of modern DBS for TRD started with the seminal study by Helen Mayberg and Andres Lozano which applied DBS to the subcallosal cingulate region (SCC, also referred to as Brodman Area 25). BA 25 is involved in the regulation of mood and implicated in the pathophysiology of depression. Initial and recent open-label studies showed promising results, with significant improvements in depressive symptoms for many patients.
Randomized controlled trials, such as those targeting the SCC and the ventral capsule/ventral striatum (VC/VS), have shown mixed outcomes, highlighting the complexity of DBS as a treatment for depression. Use of advanced imaging modalities such as diffusion-weighted imaging based tractography has led to the discovery of the so-called 'depression switch', the intersection of four bundles that allowed more deliberate targeting of DBS in the SCC area and improved results in additional open-label studies. More recently, it became possible to sense brain signals from the SCC region that allowed inferring states of depression which could potentially lead to adaptive deep brain stimulation for depression.
Despite these successes, mixed results in randomized trials has led to the exploration of alternative routes on how to personalize DBS therapy through better understanding of the brain networks involved in individual cases of depression. Based on personalization strategies established in surgical treatment of epilepsy (see above), research has begun to incorporate sEEG and intracranial recordings to map depression-relevant brain circuits and optimize stimulation parameters. Most notably, the studies by Scangos et al. (2020) and Sheth et al. (2022) explored personalized approaches to deep brain stimulation for TRD by utilizing intracranial recordings to tailor stimulation parameters. Scangos et al. demonstrated the effectiveness of mapping emotional and clinical responses to multi-site brain stimulation, revealing state-dependent and reproducible effects that offer proof of concept for circuit-specific neuromodulation. Sheth et al. also applied sEEG to map brain networks and optimize DBS settings in a 37-year-old patient, targeting the subcallosal cingulate and VC/VS area. This individualized approach led to the remission of depressive symptoms, showcasing the potential of sEEG-informed DBS as a platform for precise neuromodulation in psychiatric disorders.
Beyond the SCC and VC/VS, a third target includes the so-called 'superolateral branch' of the medial forebrain bundle (MFB). It is critical to mention that, as acknowledged by the original authors, the anatomical description of this bundle rather matches the one of the anterior limb of the internal capsule (see above) and takes a course within the capsule, rather than following a trans-hypothalamic route as known for the MFB proper. This target site was discovered serendipitously when a patient with Parkinson's Disease developed hypomania under subthalamic nucleus DBS. While this is not an uncommon side-effect of STN-DBS and alternative pathomechanisms have been suggested, the original investigators attributed the occurrence of hypomania to stimulation of a hitherto undescribed 'superolateral' branch of the MFB, which supposedly only exists in humans. While anatomical descriptions as well as supposed mechanisms for this target site have been debated, clinical effects of this DBS target in patients with TRD have been very promising and at times with sudden onset of symptom improvements in open-label studies.
Chronic pain
Stimulation of the periaqueductal gray and periventricular gray for nociceptive pain, and the internal capsule, ventral posterolateral nucleus, and ventral posteromedial nucleus for neuropathic pain has produced impressive results with some people, but results vary. One study of 17 people with intractable cancer pain found that 13 were virtually pain-free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life. DBS has also been applied for phantom limb pain.
Other clinical applications
Results of DBS in people with dystonia, where positive effects often appear gradually over a period of weeks to months, indicate a role of functional reorganization in at least some cases. The procedure has been tested for effectiveness in people with epilepsy that is resistant to medication. DBS may reduce or eliminate epileptic seizures with programmed or responsive stimulation.
DBS of the septal areas of persons with schizophrenia has resulted in enhanced alertness, cooperation, and euphoria. Persons with narcolepsy and complex-partial seizures also reported euphoria and sexual thoughts from self-elicited DBS of the septal nuclei.
Orgasmic ecstasy was reported with the electrical stimulation of the brain with depth electrodes in the left hippocampus at 3mA, and the right hippocampus at 1 mA.
In 2015, a group of Brazilian researchers led by neurosurgeon Erich Fonoff described a new technique that allows for simultaneous implants of electrodes called bilateral stereotactic procedure for DBS. The main benefits are less time spent on the procedure and greater accuracy.
In 2016, DBS was found to improve learning and memory in a mouse model of Rett syndrome. More recent (2018) work showed, that forniceal DBS upregulates genes involved in synaptic function, cell survival, and neurogenesis, making some first steps at explaining the restoration of hippocampal circuit function.
Adaptive Deep Brain Stimulation
Adaptive of Closed Loop Deep Brain Stimulation is a technique in which a steering signal influences when, with which amplitude or at which electrode contacts the DBS system is activated. This steering signal can be a physiological sensing signal, which is typically either recorded from the same implanted electrode or a cortical electrode/ECoG strip/grid. Alternatively, signals from wearables, that e.g. detect symptoms such as tremor, may be used to guide stimulation across time. The concept of adaptive deep brain stimulation is as old as the concept of electrical stimulation of the brain, itself, i.e. originates in the 1950ies-1960ies and was implemented by early pioneers such as Carl-Wilhelm Sem-Jacobsen, Natalia Bechtereva, José Delgado or Robert Heath. The reason these scientists came up with the concept so early was out of necessity: At the time, chronic stimulation as carried out in open-loop (conventional) DBS applications was not technically possible using fully implanted devices, since the battery technology at the time was not ready to do so. With the advent of 'modern' DBS as implemented by the team of Alim Louis Benabid, for decades, chronic, open-loop DBS became the dominant application. Here, pulses are emitted to the brain tissue in a fixed frequency (often 130 Hz) without sensing brain signals or other forms of a steering signal.It took until the 2010s, after a demonstration of efficacy of aDBS in the macaque by the team of Hagai Bergman in 2011, the first in-human application of aDBS was carried out by the team of Peter Brown in 2013, followed by the team of Alberto Priori in the same year. Since then, several companies, including Medtronic and Newronika have begun developing commercial applications of closed-loop DBS.
Adverse effects
DBS carries the risks of major surgery, with a complication rate related to the experience of the surgical team. The major complications include hemorrhage (1–2%) and infection (3–5%).
The potential exists for neuropsychiatric side effects after DBS, including apathy, hallucinations, hypersexuality, cognitive dysfunction, depression, and euphoria. However, these effects may be temporary and related to (1) incorrect placement of electrodes, (2) open-loop VS closed-loop stimulation, meaning a constant stimulation or an A.I. monitoring delivery system and (3) calibration of the stimulator, so these side effects are potentially reversible.
Because the brain can shift slightly during surgery, the electrodes can become displaced or dislodged from the specific location. This may cause more profound complications such as personality changes, but electrode misplacement is relatively easy to identify using CT scan. Also, surgery complications may occur, such as bleeding within the brain. After surgery, swelling of the brain tissue, mild disorientation, and sleepiness are normal. After 2–4 weeks, a follow-up visit is used to remove sutures, turn on the neurostimulator, and program it.
Impaired swimming skills surfaced as an unexpected risk of the procedure; several Parkinson's disease patients lost their ability to swim after receiving deep brain stimulation.
Mechanisms
The exact mechanism of action of DBS is not known. A variety of hypotheses try to explain the mechanisms of DBS:
- Depolarization blockade: Electrical currents block the neuronal output at or near the electrode site.
- Synaptic inhibition: This causes an indirect regulation of the neuronal output by activating axon terminals with synaptic connections to neurons near the stimulating electrode.
- Desynchronization of abnormal oscillatory activity of neurons
- Antidromic activation either activating/blockading distant neurons or blockading slow axons
DBS represents an advance on previous treatments which involved pallidotomy (i.e., surgical ablation of the globus pallidus) or thalamotomy (i.e., surgical ablation of the thalamus). Instead, a thin lead with multiple electrodes is implanted in the globus pallidus, nucleus ventralis intermedius thalami, or subthalamic nucleus, and electric pulses are used therapeutically. The lead from the implant is extended to the neurostimulator under the skin in the chest area.
Its direct effect on the physiology of brain cells and neurotransmitters is currently debated, but by sending high-frequency electrical impulses into specific areas of the brain, it can mitigate symptoms and directly diminish the side effects induced by PD medications, allowing a decrease in medications, or making a medication regimen more tolerable.
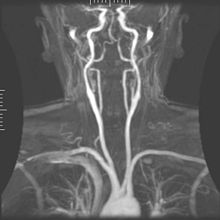
Components and placement
The DBS system consists of three components: the implanted pulse generator (IPG), the lead, and an extension. The IPG is a battery-powered neurostimulator encased in a titanium housing, which sends electrical pulses to the brain that interfere with neural activity at the target site. The lead is a coiled wire insulated in polyurethane with four platinum-iridium electrodes and is placed in one or two different nuclei of the brain. The lead is connected to the IPG by an extension, an insulated wire that runs below the skin, from the head, down the side of the neck, behind the ear, to the IPG, which is placed subcutaneously below the clavicle, or in some cases, the abdomen.[19] The IPG can be calibrated by a neurologist, nurse, or trained technician to optimize symptom suppression and control side effects.
DBS leads are placed in the brain according to the type of symptoms to be addressed. For non-Parkinsonian essential tremor, the lead is placed in either the ventrointermediate nucleus of the thalamus or the zona incerta; for dystonia and symptoms associated with PD (rigidity, bradykinesia/akinesia, and tremor), the lead may be placed in either the globus pallidus internus or the subthalamic nucleus; for OCD and depression to the nucleus accumbens; for incessant pain to the posterior thalamic region or periaqueductal gray; and for epilepsy treatment to the anterior thalamic nucleus.
All three components are surgically implanted inside the body. Lead implantation may take place under local anesthesia or under general anesthesia ("asleep DBS"), such as for dystonia. A hole about 14 mm in diameter is drilled in the skull and the probe electrode is inserted stereotactically, using either frame-based or frameless stereotaxis. During the awake procedure with local anesthesia, feedback from the person is used to determine the optimal placement of the permanent electrode. During the asleep procedure, intraoperative MRI guidance is used for direct visualization of brain tissue and device. The installation of the IPG and extension leads occurs under general anesthesia. The right side of the brain is stimulated to address symptoms on the left side of the body and vice versa.