| Anticonvulsant | |
|---|---|
| Drug class | |
| Class identifiers | |
| Synonyms | Antiepileptic drugs, antiseizure drugs |
| Use | Epilepsy |
| Biological target | Brain |
Anticonvulsants (also commonly known as antiepileptic drugs or as antiseizure drugs) are a diverse group of pharmacological agents used in the treatment of epileptic seizures. Anticonvulsants are also increasingly being used in the treatment of bipolar disorder and borderline personality disorder, since many seem to act as mood stabilizers, and for the treatment of neuropathic pain. Anticonvulsants suppress the excessive rapid firing of neurons during seizures. Anticonvulsants also prevent the spread of the seizure within the brain.
Conventional antiepileptic drugs may block sodium channels or enhance γ-aminobutyric acid (GABA) function. Several antiepileptic drugs have multiple or uncertain mechanisms of action. Next to the voltage-gated sodium channels and components of the GABA system, their targets include GABAA receptors, the GAT-1 GABA transporter, and GABA transaminase. Additional targets include voltage-gated calcium channels, SV2A, and α2δ. By blocking sodium or calcium channels, antiepileptic drugs reduce the release of excitatory glutamate, whose release is considered to be elevated in epilepsy, but also that of GABA. This is probably a side effect or even the actual mechanism of action for some antiepileptic drugs, since GABA can itself, directly or indirectly, act proconvulsively. Another potential target of antiepileptic drugs is the peroxisome proliferator-activated receptor alpha. The drug class was the 5th-best-selling in the US in 2007.
Some anticonvulsants have shown antiepileptogenic effects in animal models of epilepsy. That is, they either prevent the development of epilepsy or can halt or reverse the progression of epilepsy. However, no drug has been shown in human trials to prevent epileptogenesis (the development of epilepsy in an individual at risk, such as after a head injury).
Terminology
Approval
The usual method of achieving approval for a drug is to show it is effective when compared against placebo, or that it is more effective than an existing drug. In monotherapy (where only one drug is taken) it is considered unethical by most to conduct a trial with placebo on a new drug of uncertain efficacy. This is because untreated epilepsy leaves the patient at significant risk of death. Therefore, almost all new epilepsy drugs are initially approved only as adjunctive (add-on) therapies. Patients whose epilepsy is currently uncontrolled by their medication (i.e., it is refractory to treatment) are selected to see if supplementing the medication with the new drug leads to an improvement in seizure control. Any reduction in the frequency of seizures is compared against a placebo. The lack of superiority over existing treatment, combined with lacking placebo-controlled trials, means that few modern drugs have earned FDA approval as initial monotherapy. In contrast, Europe only requires equivalence to existing treatments, and has approved many more. Despite their lack of FDA approval, the American Academy of Neurology and the American Epilepsy Society still recommend a number of these new drugs as initial monotherapy.Drugs
In the following list, the dates in parentheses are the earliest approved use of the drug.Aldehydes
- Paraldehyde (1882). One of the earliest anticonvulsants. It is still used to treat status epilepticus, particularly where there are no resuscitation facilities.
Aromatic allylic alcohols
- Stiripentol (2001 – limited availability). Indicated for the treatment of Dravet syndrome.
Barbiturates
Barbiturates are drugs that act as central nervous system (CNS) depressants, and by virtue of this they produce a wide spectrum of effects, from mild sedation to anesthesia. The following are classified as anticonvulsants:- Phenobarbital (1912). See also the related drug primidone.
- Methylphenobarbital (1935). Known as mephobarbital in the US. No longer marketed in the UK
- Barbexaclone (1982). Only available in some European countries.
Benzodiazepines
The benzodiazepines are a class of drugs with hypnotic, anxiolytic, anticonvulsive, amnestic and muscle relaxant properties. Benzodiazepines act as a central nervous system depressant. The relative strength of each of these properties in any given benzodiazepine varies greatly and influences the indications for which it is prescribed. Long-term use can be problematic due to the development of tolerance to the anticonvulsant effects and dependency. Of the many drugs in this class, only a few are used to treat epilepsy:- Clobazam (1979). Notably used on a short-term basis around menstruation in women with catamenial epilepsy.
- Clonazepam (1974).
- Clorazepate (1972).
- Diazepam (1963). Can be given rectally by trained care-givers.
- Midazolam (N/A). Increasingly being used as an alternative to diazepam. This water-soluble drug is squirted into the side of the mouth but not swallowed. It is rapidly absorbed by the buccal mucosa.
- Lorazepam (1972). Given by injection in hospital.
Bromides
- Potassium bromide (1857). The earliest effective treatment for epilepsy. There would not be a better drug until phenobarbital in 1912. It is still used as an anticonvulsant for dogs and cats.
Carbamates
- Felbamate (1993). This effective anticonvulsant has had its usage severely restricted due to rare but life-threatening side effects.
Carboxamides
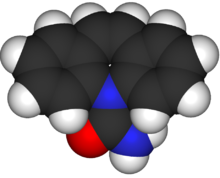
Carbamazepine
The following are carboxamides:
- Carbamazepine (1963). A popular anticonvulsant that is available in generic formulations.
- Oxcarbazepine (1990). A derivative of carbamazepine that has similar efficacy but is better tolerated and is also available generically.
- Eslicarbazepine acetate (2009)
Fatty acids
The following are fatty-acids:- The valproates — valproic acid, sodium valproate, and divalproex sodium (1967).
- Vigabatrin (1989).
- Progabide (1987)
- Tiagabine (1996).
Fructose derivatives
- Topiramate (1995).
GABA analogs
- Gabapentin (1993).
- Pregabalin (2004).
- Vigabatrin (1989).
- Progabide (1987).
Hydantoins
The following are hydantoins:- Ethotoin (1957).
- Phenytoin (1938).
- Mephenytoin
- Fosphenytoin (1996).
Oxazolidinediones
The following are oxazolidinediones:- Paramethadione
- Trimethadione (1946).
- Ethadione
Propionates
Pyrimidinediones
- Primidone (1952).
Pyrrolidines
Succinimides
The following are succinimides:- Ethosuximide (1955).
- Phensuximide
- Mesuximide
Sulfonamides
- Acetazolamide (1953).
- Sultiame
- Methazolamide
- Zonisamide (2000).
Triazines
- Lamotrigine (1990).
Ureas
Valproylamides
Other
- Perampanel
- Stiripentol
- Pyridoxine (1939)
Non-pharmaceutical anticonvulsants
Sometimes, ketogenic diet or vagus nerve stimulation are described as "anticonvulsant" therapies as well. However they do not work as well as the anticonvulsant drugsTreatment guidelines
According to guidelines by the American Academy of Neurology and American Epilepsy Society, mainly based on a major article review in 2004, patients with newly diagnosed epilepsy who require treatment can be initiated on standard anticonvulsants such as carbamazepine, phenytoin, valproic acid/valproate semisodium, phenobarbital, or on the newer anticonvulsants gabapentin, lamotrigine, oxcarbazepine or topiramate. The choice of anticonvulsants depends on individual patient characteristics. Both newer and older drugs are generally equally effective in new onset epilepsy. The newer drugs tend to have fewer side effects. For newly diagnosed partial or mixed seizures, there is evidence for using gabapentin, lamotrigine, oxcarbazepine or topiramate as monotherapy. Lamotrigine can be included in the options for children with newly diagnosed absence seizures.History
The first anticonvulsant was bromide, suggested in 1857 by the British gynecologist Charles Locock who used it to treat women with "hysterical epilepsy" (probably catamenial epilepsy). Bromides are effective against epilepsy, and also cause impotence, which is not related to its anti-epileptic effects. Bromide also suffered from the way it affected behaviour, introducing the idea of the 'epileptic personality' which was actually a result of medication. Phenobarbital was first used in 1912 for both its sedative and antiepileptic properties. By the 1930s, the development of animal models in epilepsy research led to the development of phenytoin by Tracy Putnam and H. Houston Merritt, which had the distinct advantage of treating epileptic seizures with less sedation.[35] By the 1970s, a National Institutes of Health initiative, the Anticonvulsant Screening Program, headed by J. Kiffin Penry, served as a mechanism for drawing the interest and abilities of pharmaceutical companies in the development of new anticonvulsant medications.Marketing approval history
The following table lists anticonvulsant drugs together with the date their marketing was approved in the US, UK and France. Data for the UK and France are incomplete. In recent years, the European Medicines Agency has approved drugs throughout the European Union. Some of the drugs are no longer marketed.| Drug | Brand | US | UK | France |
|---|---|---|---|---|
| acetazolamide | Diamox | 27 July 1953 | 1988 |
|
| carbamazepine | Tegretol | 15 July 1974 | 1965 | 1963 |
| clobazam | Frisium |
| 1979 |
|
| clonazepam | Klonopin/Rivotril | 4 June 1975 | 1974 |
|
| diazepam | Valium | 15 November 1963 |
|
|
| divalproex sodium | Depakote | 10 March 1983 |
|
|
| eslicarbazepine |
|
Data needed |
|
|
| ethosuximide | Zarontin | 2 November 1960 | 1955 | 1962 |
| ethotoin | Peganone | 22 April 1957 |
|
|
| felbamate | Felbatol | 29 July 1993 |
|
|
| fosphenytoin | Cerebyx | 5 August 1996 |
|
|
| gabapentin | Neurontin | 30 December 1993 | May 1993 | October 1994 |
| lamotrigine | Lamictal | 27 December 1994 | October 1991 | May 1995 |
| lacosamide | Vimpat | 28 October 2008 |
|
|
| levetiracetam | Keppra | 30 November 1999 | 29 September 2000 | 29 September 2000 |
| mephenytoin | Mesantoin | 23 October 1946 |
|
|
| metharbital | Gemonil | 1952 |
|
|
| methsuximide | Celontin | 8 February 1957 |
|
|
| methazolamide | Neptazane | 26 January 1959 |
|
|
| oxcarbazepine | Trileptal | 14 January 2000 | 2000 |
|
| phenobarbital |
|
|
1912 | 1920 |
| phenytoin | Dilantin/Epanutin | 1938 | 1938 | 1941 |
| phensuximide | Milontin | 1953 |
|
|
| pregabalin | Lyrica | 30 December 2004 | 6 July 2004 | 6 July 2004 |
| primidone | Mysoline | 8 March 1954 | 1952 | 1953 |
| sodium valproate | Epilim |
|
December 1977 | June 1967 |
| stiripentol | Diacomit |
|
5 December 2001 | 5 December 2001 |
| tiagabine | Gabitril | 30 September 1997 | 1998 | November 1997 |
| topiramate | Topamax | 24 December 1996 | 1995 |
|
| trimethadione | Tridione | 25 January 1946 |
|
|
| valproic acid | Depakene/Convulex | 28 February 1978 | 1993 |
|
| vigabatrin | Sabril | 21 August 2009 | 1989 |
|
| zonisamide | Zonegran | 27 March 2000 | 10 March 2005 | 10 March 2005 |
Pregnancy
During pregnancy, the metabolism of several anticonvulsants is affected. There may be an increase in the clearance and resultant decrease in the blood concentration of lamotrigine, phenytoin, and to a lesser extent carbamazepine, and possibly decreases the level of levetiracetam and the active oxcarbazepine metabolite, the monohydroxy derivative. Therefore, these drugs should be monitored during use in pregnancy.Many of the common used medications, such as valproate, phenytoin, carbamazepine, phenobarbitol, gabapentin have been reported to cause increased risk of birth defects. Among anticonvulsants, levetiracetam and lamotrigine seem to carry the lowest risk of causing birth defects. The risk of untreated epilepsy is believed to be greater than the risk of adverse effects caused by these medications, necessitating continuation of antiepileptic treatment.
Valproic acid, and its derivatives such as sodium valproate and divalproex sodium, causes cognitive deficit in the child, with an increased dose causing decreased intelligence quotient. On the other hand, evidence is conflicting for carbamazepine regarding any increased risk of congenital physical anomalies or neurodevelopmental disorders by intrauterine exposure. Similarly, children exposed lamotrigine or phenytoin in the womb do not seem to differ in their skills compared to those who were exposed to carbamazepine.
There is inadequate evidence to determine if newborns of women with epilepsy taking anticonvulsants have a substantially increased risk of hemorrhagic disease of the newborn.
Regarding breastfeeding, some anticonvulsants probably pass into breast milk in clinically significant amounts, including primidone and levetiracetam. On the other hand, valproate, phenobarbital, phenytoin, and carbamazepine probably are not transferred into breast milk in clinically important amounts.
In animal models, several anticonvulsant drugs have been demonstrated to induce neuronal apoptosis in the developing brain.