Medicinal plants, also called medicinal herbs, have been discovered and used in traditional medicine practices since prehistoric times. Plants synthesise hundreds of chemical compounds for functions including defence against insects, fungi, diseases, and herbivorous mammals. Numerous phytochemicals with potential or established biological activity have been identified. However, since a single plant contains widely diverse phytochemicals, the effects of using a whole plant as medicine are uncertain. Further, the phytochemical content and pharmacological actions, if any, of many plants having medicinal potential remain unassessed by rigorous scientific research to define efficacy and safety.
The earliest historical records of herbs are found from the Sumerian civilisation, where hundreds of medicinal plants including opium are listed on clay tablets. The Ebers Papyrus from ancient Egypt, c. 1550 BC, describes over 850 plant medicines. The Greek physician Dioscorides, who worked in the Roman army, documented over 1000 recipes for medicines using over 600 medicinal plants in De materia medica, c. 60 AD; this formed the basis of pharmacopoeias for some 1500 years. Drug research makes use of ethnobotany to search for pharmacologically active substances in nature, and has in this way discovered hundreds of useful compounds. These include the common drugs aspirin, digoxin, quinine, and opium. The compounds found in plants are of many kinds, but most are in four major biochemical classes: alkaloids, glycosides, polyphenols, and terpenes.
Medicinal plants are widely used in non-industrialized societies, mainly because they are readily available and cheaper than modern medicines. The annual global export value of the thousands of types of plants with suspected medicinal properties was estimated to be US$2.2 billion in 2012. In 2017, the potential global market for botanical extracts and medicines was estimated at several hundred billion dollars. In many countries, there is little regulation of traditional medicine, but the World Health Organization coordinates a network to encourage safe and rational usage. Medicinal plants face both general threats, such as climate change and habitat destruction, and the specific threat of over-collection to meet market demand.
History
Prehistoric times
Plants, including many now used as culinary herbs and spices, have been used as medicines, not necessarily effectively, from prehistoric times. Spices have been used partly to counter food spoilage bacteria, especially in hot climates, and especially in meat dishes which spoil more readily. Angiosperms (flowering plants) were the original source of most plant medicines. Human settlements are often surrounded by weeds used as herbal medicines, such as nettle, dandelion and chickweed. Humans were not alone in using herbs as medicines: some animals such as non-human primates, monarch butterflies and sheep ingest medicinal plants when they are ill. Plant samples from prehistoric burial sites are among the lines of evidence that Paleolithic peoples had knowledge of herbal medicine. For instance, a 60 000-year-old Neanderthal burial site, "Shanidar IV", in northern Iraq has yielded large amounts of pollen from eight plant species, seven of which are used now as herbal remedies. A mushroom was found in the personal effects of Ötzi the Iceman, whose body was frozen in the Ötztal Alps for more than 5,000 years. The mushroom was probably used against whipworm.
Ancient times
In ancient Sumeria, hundreds of medicinal plants including myrrh and opium are listed on clay tablets. The ancient Egyptian Ebers Papyrus lists over 800 plant medicines such as aloe, cannabis, castor bean, garlic, juniper, and mandrake. From ancient times to the present, Ayurvedic medicine as documented in the Atharva Veda, the Rig Veda and the Sushruta Samhita has used hundreds of pharmacologically active herbs and spices such as turmeric, which contains curcumin. The Chinese pharmacopoeia, the Shennong Ben Cao Jing records plant medicines such as chaulmoogra for leprosy, ephedra, and hemp. This was expanded in the Tang Dynasty Yaoxing Lun. In the fourth century BC, Aristotle's pupil Theophrastus wrote the first systematic botany text, Historia plantarum. In around 60 AD, the Greek physician Pedanius Dioscorides, working for the Roman army, documented over 1000 recipes for medicines using over 600 medicinal plants in De materia medica. The book remained the authoritative reference on herbalism for over 1500 years, into the seventeenth century.
Middle Ages
In the Early Middle Ages, Benedictine monasteries preserved medical knowledge in Europe, translating and copying classical texts and maintaining herb gardens. Hildegard of Bingen wrote Causae et Curae ("Causes and Cures") on medicine. In the Islamic Golden Age, scholars translated many classical Greek texts including Dioscorides into Arabic, adding their own commentaries. Herbalism flourished in the Islamic world, particularly in Baghdad and in Al-Andalus. Among many works on medicinal plants, Abulcasis (936–1013) of Cordoba wrote The Book of Simples, and Ibn al-Baitar (1197–1248) recorded hundreds of medicinal herbs such as Aconitum, nux vomica, and tamarind in his Corpus of Simples. Avicenna included many plants in his 1025 The Canon of Medicine. Abu-Rayhan Biruni, Ibn Zuhr, Peter of Spain, and John of St Amand wrote further pharmacopoeias.
Early Modern
The Early Modern period saw the flourishing of illustrated herbals across Europe, starting with the 1526 Grete Herball. John Gerard wrote his famous The Herball or General History of Plants in 1597, based on Rembert Dodoens, and Nicholas Culpeper published his The English Physician Enlarged. Many new plant medicines arrived in Europe as products of Early Modern exploration and the resulting Columbian Exchange, in which livestock, crops and technologies were transferred between the Old World and the Americas in the 15th and 16th centuries. Medicinal herbs arriving in the Americas included garlic, ginger, and turmeric; coffee, tobacco and coca travelled in the other direction. In Mexico, the sixteenth century Badianus Manuscript described medicinal plants available in Central America.
19th and 20th centuries
The place of plants in medicine was radically altered in the 19th century by the application of chemical analysis. Alkaloids were isolated from a succession of medicinal plants, starting with morphine from the poppy in 1806, and soon followed by ipecacuanha and strychnos in 1817, quinine from the cinchona tree, and then many others. As chemistry progressed, additional classes of pharmacologically active substances were discovered in medicinal plants. Commercial extraction of purified alkaloids including morphine from medicinal plants began at Merck in 1826. Synthesis of a substance first discovered in a medicinal plant began with salicylic acid in 1853. Around the end of the 19th century, the mood of pharmacy turned against medicinal plants, as enzymes often modified the active ingredients when whole plants were dried, and alkaloids and glycosides purified from plant material started to be preferred. Drug discovery from plants continued to be important through the 20th century and into the 21st, with important anti-cancer drugs from yew and Madagascar periwinkle.
Context
Medicinal plants are used with the intention of maintaining health, to be administered for a specific condition, or both, whether in modern medicine or in traditional medicine. The Food and Agriculture Organization estimated in 2002 that over 50,000 medicinal plants are used across the world. The Royal Botanic Gardens, Kew more conservatively estimated in 2016 that 17,810 plant species have a medicinal use, out of some 30,000 plants for which a use of any kind is documented.
In modern medicine, around a quarter of the drugs prescribed to patients are derived from medicinal plants, and they are rigorously tested. In other systems of medicine, medicinal plants may constitute the majority of what are often informal attempted treatments, not tested scientifically. The World Health Organization estimates, without reliable data, that some 80 percent of the world's population depends mainly on traditional medicine (including but not limited to plants); perhaps some two billion people are largely reliant on medicinal plants. The use of plant-based materials including herbal or natural health products with supposed health benefits, is increasing in developed countries. This brings attendant risks of toxicity and other effects on human health, despite the safe image of herbal remedies. Herbal medicines have been in use since long before modern medicine existed; there was and often still is little or no knowledge of the pharmacological basis of their actions, if any, or of their safety. The World Health Organization formulated a policy on traditional medicine in 1991, and since then has published guidelines for them, with a series of monographs on widely used herbal medicines.
Medicinal plants may provide three main kinds of benefit: health benefits to the people who consume them as medicines; financial benefits to people who harvest, process, and distribute them for sale; and society-wide benefits, such as job opportunities, taxation income, and a healthier labour force. However, development of plants or extracts having potential medicinal uses is blunted by weak scientific evidence, poor practices in the process of drug development, and insufficient financing.
Phytochemical basis
All plants produce chemical compounds which give them an evolutionary advantage, such as defending against herbivores or, in the example of salicylic acid, as a hormone in plant defenses. These phytochemicals have potential for use as drugs, and the content and known pharmacological activity of these substances in medicinal plants is the scientific basis for their use in modern medicine, if scientifically confirmed. For instance, daffodils (Narcissus) contain nine groups of alkaloids including galantamine, licensed for use against Alzheimer's disease. The alkaloids are bitter-tasting and toxic, and concentrated in the parts of the plant such as the stem most likely to be eaten by herbivores; they may also protect against parasites.
Modern knowledge of medicinal plants is being systematised in the Medicinal Plant Transcriptomics Database, which by 2011 provided a sequence reference for the transcriptome of some thirty species. The major classes of pharmacologically active phytochemicals are described below, with examples of medicinal plants that contain them.
Alkaloids
Alkaloids are bitter-tasting chemicals, very widespread in nature, and often toxic, found in many medicinal plants. There are several classes with different modes of action as drugs, both recreational and pharmaceutical. Medicines of different classes include atropine, scopolamine, and hyoscyamine (all from nightshade), the traditional medicine berberine (from plants such as Berberis and Mahonia), caffeine (Coffea), cocaine (Coca), ephedrine (Ephedra), morphine (opium poppy), nicotine (tobacco), reserpine (Rauvolfia serpentina), quinidine and quinine (Cinchona), vincamine (Vinca minor), and vincristine (Catharanthus roseus).
The opium poppy Papaver somniferum is the source of the alkaloids morphine and codeine.
The alkaloid nicotine from tobacco binds directly to the body's Nicotinic acetylcholine receptors, accounting for its pharmacological effects.
Deadly nightshade, Atropa belladonna, yields tropane alkaloids including atropine, scopolamine and hyoscyamine.
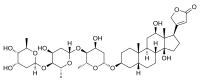
Glycosides
Anthraquinone glycosides are found in medicinal plants such as rhubarb, cascara, and Alexandrian senna. Plant-based laxatives made from such plants include senna, rhubarb and Aloe.
The cardiac glycosides are powerful drugs from medicinal plants including foxglove and lily of the valley. They include digoxin and digitoxin which support the beating of the heart, and act as diuretics.
Senna alexandrina, containing anthraquinone glycosides, has been used as a laxative for millennia.
The foxglove, Digitalis purpurea, contains digoxin, a cardiac glycoside. The plant was used on heart conditions long before the glycoside was identified.
Digoxin is used to treat atrial fibrillation, atrial flutter and sometimes heart failure.
Polyphenols
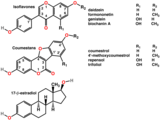
Polyphenols of several classes are widespread in plants, having diverse roles in defenses against plant diseases and predators. They include hormone-mimicking phytoestrogens and astringent tannins. Plants containing phytoestrogens have been administered for centuries for gynecological disorders, such as fertility, menstrual, and menopausal problems. Among these plants are Pueraria mirifica, kudzu, angelica, fennel, and anise.
Many polyphenolic extracts, such as from grape seeds, olives or maritime pine bark, are sold as dietary supplements and cosmetics without proof or legal health claims for beneficial health effects. In Ayurveda, the astringent rind of the pomegranate, containing polyphenols called punicalagins, is used as a medicine.
Angelica, containing phytoestrogens, has long been used for gynaecological disorders.
Polyphenols include phytoestrogens (top and middle), mimics of animal estrogen (bottom).
Terpenes
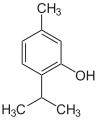
Terpenes and terpenoids of many kinds are found in a variety of medicinal plants, and in resinous plants such as the conifers. They are strongly aromatic and serve to repel herbivores. Their scent makes them useful in essential oils, whether for perfumes such as rose and lavender, or for aromatherapy. Some have medicinal uses: for example, thymol is an antiseptic and was once used as a vermifuge (anti-worm medicine).
The essential oil of common thyme (Thymus vulgaris), contains the monoterpene thymol, an antiseptic and antifungal.
Thymol is one of many terpenes found in plants.
In practice
Cultivation
Medicinal plants demand intensive management. Different species each require their own distinct conditions of cultivation. The World Health Organization recommends the use of rotation to minimise problems with pests and plant diseases. Cultivation may be traditional or may make use of conservation agriculture practices to maintain organic matter in the soil and to conserve water, for example with no-till farming systems. In many medicinal and aromatic plants, plant characteristics vary widely with soil type and cropping strategy, so care is required to obtain satisfactory yields.
Preparation
Medicinal plants are often tough and fibrous, requiring some form of preparation to make them convenient to administer. According to the Institute for Traditional Medicine, common methods for the preparation of herbal medicines include decoction, powdering, and extraction with alcohol, in each case yielding a mixture of substances. Decoction involves crushing and then boiling the plant material in water to produce a liquid extract that can be taken orally or applied topically. Powdering involves drying the plant material and then crushing it to yield a powder that can be compressed into tablets. Alcohol extraction involves soaking the plant material in cold wine or distilled spirit to form a tincture.
Traditional poultices were made by boiling medicinal plants, wrapping them in a cloth, and applying the resulting parcel externally to the affected part of the body.
When modern medicine has identified a drug in a medicinal plant, commercial quantities of the drug may either be synthesised or extracted from plant material, yielding a pure chemical. Extraction can be practical when the compound in question is complex.
Usage
Plant medicines are in wide use around the world. In most of the developing world, especially in rural areas, local traditional medicine, including herbalism, is the only source of health care for people, while in the developed world, alternative medicine including use of dietary supplements is marketed aggressively using the claims of traditional medicine. As of 2015, most products made from medicinal plants had not been tested for their safety and efficacy, and products that were marketed in developed economies and provided in the undeveloped world by traditional healers were of uneven quality, sometimes containing dangerous contaminants. Traditional Chinese medicine makes use of a wide variety of plants, among other materials and techniques. Researchers from Kew Gardens found 104 species used for diabetes in Central America, of which seven had been identified in at least three separate studies. The Yanomami of the Brazilian Amazon, assisted by researchers, have described 101 plant species used for traditional medicines.
Drugs derived from plants including opiates, cocaine and cannabis have both medical and recreational uses. Different countries have at various times made use of illegal drugs, partly on the basis of the risks involved in taking psychoactive drugs.
Effectiveness
Plant medicines have often not been tested systematically, but have come into use informally over the centuries. By 2007, clinical trials had demonstrated potentially useful activity in nearly 16% of herbal medicines; there was limited in vitro or in vivo evidence for roughly half the medicines; there was only phytochemical evidence for around 20%; 0.5% were allergenic or toxic; and some 12% had basically never been studied scientifically. Cancer Research UK caution that there is no reliable evidence for the effectiveness of herbal remedies for cancer.
A 2012 phylogenetic study built a family tree down to genus level using 20,000 species to compare the medicinal plants of three regions, Nepal, New Zealand and the South African Cape. It discovered that the species used traditionally to treat the same types of condition belonged to the same groups of plants in all three regions, giving a "strong phylogenetic signal". Since many plants that yield pharmaceutical drugs belong to just these groups, and the groups were independently used in three different world regions, the results were taken to mean 1) that these plant groups do have potential for medicinal efficacy, 2) that undefined pharmacological activity is associated with use in traditional medicine, and 3) that the use of a phylogenetic groups for medicines in one region may predict their use in the other regions.
Regulation
The World Health Organization (WHO) has been coordinating a network called the International Regulatory Cooperation for Herbal Medicines to try to improve the quality of medical products made from medicinal plants and the claims made for them. In 2015, only around 20% of countries had well-functioning regulatory agencies, while 30% had none, and around half had limited regulatory capacity. In India, where Ayurveda has been practised for centuries, herbal remedies are the responsibility of a government department, AYUSH, under the Ministry of Health & Family Welfare.
WHO has set out a strategy for traditional medicines with four objectives: to integrate them as policy into national healthcare systems; to provide knowledge and guidance on their safety, efficacy, and quality; to increase their availability and affordability; and to promote their rational, therapeutically sound usage. WHO notes in the strategy that countries are experiencing seven challenges to such implementation, namely in developing and enforcing policy; in integration; in safety and quality, especially in assessment of products and qualification of practitioners; in controlling advertising; in research and development; in education and training; and in the sharing of information.
Drug discovery
The pharmaceutical industry has roots in the apothecary shops of Europe in the 1800s, where pharmacists provided local traditional medicines to customers, which included extracts like morphine, quinine, and strychnine. Therapeutically important drugs like camptothecin (from Camptotheca acuminata, used in traditional Chinese medicine) and taxol (from the Pacific yew, Taxus brevifolia) were derived from medicinal plants. The Vinca alkaloids vincristine and vinblastine, used as anti-cancer drugs, were discovered in the 1950s from the Madagascar periwinkle, Catharanthus roseus.
Hundreds of compounds have been identified using ethnobotany, investigating plants used by indigenous peoples for possible medical applications. Some important phytochemicals, including curcumin, epigallocatechin gallate, genistein and resveratrol are pan-assay interference compounds, meaning that in vitro studies of their activity often provide unreliable data. As a result, phytochemicals have frequently proven unsuitable as lead compounds in drug discovery. In the United States over the period 1999 to 2012, despite several hundred applications for new drug status, only two botanical drug candidates had sufficient evidence of medicinal value to be approved by the Food and Drug Administration.
The pharmaceutical industry has remained interested in mining traditional uses of medicinal plants in its drug discovery efforts. Of the 1073 small-molecule drugs approved in the period 1981 to 2010, over half were either directly derived from or inspired by natural substances. Among cancer treatments, of 185 small-molecule drugs approved in the period from 1981 to 2019, 65% were derived from or inspired by natural substances.
Safety
Plant medicines can cause adverse effects and even death, whether by side-effects of their active substances, by adulteration or contamination, by overdose, or by inappropriate prescription. Many such effects are known, while others remain to be explored scientifically. There is no reason to presume that because a product comes from nature it must be safe: the existence of powerful natural poisons like atropine and nicotine shows this to be untrue. Further, the high standards applied to conventional medicines do not always apply to plant medicines, and dose can vary widely depending on the growth conditions of plants: older plants may be much more toxic than young ones, for instance.
Pharmacologically active plant extracts can interact with conventional drugs, both because they may provide an increased dose of similar compounds, and because some phytochemicals interfere with the body's systems that metabolise drugs in the liver including the cytochrome P450 system, making the drugs last longer in the body and have a more powerful cumulative effect. Plant medicines can be dangerous during pregnancy. Since plants may contain many different substances, plant extracts may have complex effects on the human body.
Quality, advertising, and labelling
Herbal medicine and dietary supplement products have been criticized as not having sufficient standards or scientific evidence to confirm their contents, safety, and presumed efficacy. A 2013 study found that one-third of herbal products sampled contained no trace of the herb listed on the label, and other products were adulterated with unlisted fillers including potential allergens.
Threats
Where medicinal plants are harvested from the wild rather than cultivated, they are subject to both general and specific threats. General threats include climate change and habitat loss to development and agriculture. A specific threat is over-collection to meet rising demand for medicines. A case in point was the pressure on wild populations of the Pacific yew soon after news of taxol's effectiveness became public. The threat from over-collection could be addressed by cultivation of some medicinal plants, or by a system of certification to make wild harvesting sustainable. A report in 2020 by the Royal Botanic Gardens, Kew identifies 723 medicinal plants as being at risk of extinction, caused partly by over-collection.
See also