| |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˈfoʊlɪk, |
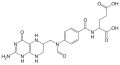
| Synonyms | FA, N-(4-{[(2-amino-4-oxo-1,4-dihydropteridin-6-yl)methyl]amino}benzoyl)-L-glutamic acid, pteroyl-L-glutamic acid, vitamin B9, vitamin Bc, vitamin M, folacin, pteroyl-L-glutamate |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682591 |
| Pregnancy category |
|
| Routes of administration | By mouth, IM, IV, sub-Q |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 50–100% |
| Metabolism | Liver |
| Excretion | Urine |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.381 |
| Chemical and physical data | |
| Formula | C19H19N7O6 |
| Molar mass | 441.404 g·mol−1 |
| Density | 1.6±0.1 g/cm3 |
| Melting point | 250 °C (482 °F) (decomposition) |
| Solubility in water | 1.6 mg/L (25 °C) mg/mL (20 °C) |
Folate, distinct forms of which are known as folic acid, folacin, and vitamin B9, is one of the B vitamins. It may be taken by mouth or by injection. The recommended adult daily intake of folate in the U.S. is 400 micrograms from foods or dietary supplements. Folate in the form of folic acid is used to treat anemia caused by folate deficiency. Folic acid is also used as a supplement by women during pregnancy to reduce the risk of neural tube defects (NTDs) in the baby. Low levels in early pregnancy are believed to be the cause of more than half of babies born with NTDs. More than 80 countries use fortification of certain foods with folic acid as a measure to decrease the rate of NTDs. Long-term supplementation is also associated with small reductions in the risk of stroke and cardiovascular disease.
No common side effects are known. There are concerns that large amounts of folic acid might hide vitamin B12 deficiency. Folate is essential for the body to make DNA, RNA, and metabolise amino acids, which are required for cell division. As humans cannot make folate, it is required from the diet, making it an essential vitamin.
Not consuming enough folate can lead to folate deficiency. This may result in a type of anemia in which low numbers of large red blood cells occur. Symptoms may include feeling tired, heart palpitations, shortness of breath, open sores on the tongue, and changes in the color of the skin or hair. Folate deficiency in children may develop within a month of poor dietary intake. In adults, normal total body folate is between 10 and 30 mg with blood levels of greater than 7 nmol/L (3 ng/mL).
Folic acid was discovered between 1931 and 1943. It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system. The wholesale cost of supplements in the developing world is between US$0.001 and 0.005 per dose as of 2014. The term "folic" is from the Latin word folium (which means leaf) because it was found in dark-green leafy vegetables. Folates occur naturally in many foods. In 2016, it was the 96th most prescribed medication in the United States, with more than 8 million prescriptions.
Definition
"Folate" is the term used to name the many forms of the vitamin—namely folic acid and its congeners, including tetrahydrofolic acid (the activated form of the vitamin), methyltetrahydrofolate (the primary form found in the serum), methenyltetrahydrofolate, folinic acid, and folacin. Other names include vitamin B9, vitamin Bc, vitamin M, and pteroyl-L-glutamate.
Health effects
Folate is necessary for the production and maintenance of new cells, for DNA synthesis and RNA synthesis through methylation, and for preventing changes to DNA.
It is especially important during periods of frequent cell division and
growth, such as infancy and pregnancy. Folate deficiency hinders DNA
synthesis and cell division, affecting hematopoietic cells and neoplasms
the most because of their greater frequency of cell division. RNA
transcription and subsequent protein synthesis are less affected by
folate deficiency, as the mRNA can be recycled and used again (as
opposed to DNA synthesis, where a new genomic copy must be created).
Since folate deficiency limits cell division, erythropoiesis (production of red blood cells) is hindered. This leads to megaloblastic anemia,
which is characterized by large, immature red blood cells. This
pathology results from persistently thwarted attempts at normal DNA
replication, DNA repair, and cell division, and produces abnormally
large red cells called megaloblasts (and hypersegmented neutrophils)
with abundant cytoplasm capable of RNA and protein synthesis, but with
clumping and fragmentation of nuclear chromatin. Some of these large
cells, although immature (reticulocytes), are released early from the
marrow in an attempt to compensate for the anemia. Both adults and children need folate to make normal red and white blood cells and prevent anemia.
Deficiency of folate in pregnant women has been implicated in NTDs;
therefore, many developed countries have implemented mandatory folic
acid fortification in cereals, etc. NTDs occur early in pregnancy (first
month), therefore women must have abundant folate upon conception.
Folate is required to make red blood cells and white blood cells and
folate deficiency may lead to anemia, which causes fatigue, weakness,
and inability to concentrate.
Pregnancy
Folate
intake during pregnancy has been linked to a lessened risk of neural
tube defects (NTDs), and for this reason there is a recommendation that
any woman planning to become pregnant consume a folate-containing
dietary supplement before and during pregnancy.
Compliance with this recommendation is not complete, and many women
become pregnant without this being a planned pregnancy, or may not
realize that they are pregnant until well into the first trimester,
which is the critical period for reducing risk of NTDs. Countries have
implemented either mandatory or voluntary food fortification of wheat
flour and other grains, or else have no such program and depend on
public health and healthcare practitioner advice to women of
childbearing age. A meta-analysis of global birth prevalence of spina
bifida showed that when mandatory fortification was compared to
countries with voluntary fortification or no fortification program,
there was a 30% reduction in live births with spina bifida. The United States Preventive Services Task Force
recommends folic acid as the supplement or fortification ingredient, as
forms of folate other than folic acid have not been studied.
A meta-analysis of folate supplementation during pregnancy reported a 28% lower risk of newborn congenital heart defects. Prenatal supplementation with folic acid did not appear to reduce the risk of preterm births. One systematic review
indicated no effect of folic acid on mortality, growth, body
composition, respiratory, or cognitive outcomes of children from birth
to 9 years old. There was no correlation between maternal folic acid supplementation and an increased risk for childhood asthma.
Fertility
Folate is necessary for fertility in both men and women. It contributes to spermatogenesis. Therefore, receiving sufficient amounts through the diet is necessary to avoid low fertility.
Also, polymorphisms in genes of enzymes involved in folate metabolism
could be one reason for fertility complications in some women with unexplained infertility.
Heart disease
Taking folic acid over years reduced the risk of cardiovascular disease by 4%, where another study found it did not affect cardiovascular disease, even while reducing homocysteine levels.
Several studies provided preliminary evidence that folate-rich diets
were associated with reduced risk of cardiovascular diseases by lowering
blood levels of homocysteine.
Stroke
Long-term
supplementation with folic acid reduced the risk of stroke by 10%,
which may be due to the role folate plays in regulating homocysteine
concentration.
A meta-analysis indicated the risk of stroke appeared to be reduced
only in some individuals, so a definite recommendation regarding
supplementation beyond the current RDA has not been established.
Asian populations had greater protection against stroke with folate
supplementation than did European or North American subjects. Observed stroke reduction is consistent with the reduction in pulse pressure
produced by folate supplementation of 5 mg per day, since hypertension
is a key risk factor for stroke. Folic supplements are inexpensive and
relatively safe to use, which is why people who have had strokes or who
have hyperhomocysteinemia are encouraged to consume daily B vitamins including folic acid.
Cancer
Studies
on folic acid intake from food and folate supplementation with regards
to cancer risk are based on the adequacy of chronic intake. Chronically
insufficient intake of folate may increase the risk of colorectal,
breast, ovarian, pancreas, brain, lung, cervical, and prostate cancers.
Other studies showed that excessive dietary supplementation with folic
acid may modestly increase the risk of certain cancers, but only prostate cancer was significant. A subsequent meta-analysis found no relationship between taking folate supplements and cancer risk of any type.
Antifolate chemotherapy
Folate is important for cells and tissues that divide rapidly. Cancer cells divide rapidly, and drugs that interfere with folate metabolism are used to treat cancer. The antifolate drug methotrexate
is often used to treat cancer because it inhibits the production of the
active form of THF from the inactive dihydrofolate (DHF). However,
methotrexate can be toxic,
producing side effects, such as inflammation in the digestive tract
that make eating normally more difficult. Also, bone marrow depression
(inducing leukopenia and thrombocytopenia) and acute kidney and liver
failure have been reported.
Folinic acid, under the drug name leucovorin, a form of folate (formyl-THF), can help "rescue" or reverse the toxic effects of methotrexate. Folinic acid is not the same as folic acid. Folic acid supplements have little established role in cancer chemotherapy.
Cases of severe adverse effects of accidental substitution of folic
acid for folinic acid have been reported in people receiving
methotrexate cancer chemotherapy. Anyone receiving methotrexate should
follow medical advice on the use of folic or folinic acid supplements.
The supplement of folinic acid in people undergoing methotrexate
treatment is to give cells dividing less rapidly enough folate to
maintain normal cell functions. The amount of folate given is depleted
by rapidly dividing cells (cancer) quickly, so does not negate the
effects of methotrexate.
Neurological
Some evidence links a shortage of folate with clinical depression. Limited evidence from randomized controlled trials showed using folic acid in addition to selective serotonin reuptake inhibitors (SSRIs) may have benefits. Research found a link between depression and low levels of folate. Folate may reduce homocysteine levels, which are associated with cognitive functions.
The exact mechanisms involved in the development of schizophrenia
and depression are not entirely clear, but the bioactive folate, methyltetrahydrofolate (5-MTHF), a direct target of methyl donors such as S-adenosyl methionine (SAMe), recycles the inactive dihydrobiopterin (BH2) into tetrahydrobiopterin (BH4), the necessary cofactor in various steps of monoamine synthesis, including that of dopamine. BH4
serves a regulatory role in monoamine neurotransmission and is required
to mediate the actions of most antidepressants. 5-MTHF also plays both
direct & indirect roles in DNA methylation, NO2 synthesis, and one-carbon metabolism.
A sub-study of the Women's Antioxidant and Folic Acid Cardiovascular Study published in 2009 reported use of a nutritional supplement containing folic acid at 2,500 μg/day, pyridoxine at 50 mg/day, and vitamin B12 at 1,000 μg/day decreased the risk of developing age-related macular degeneration
by 34.7%. The amount of folic acid used in this clinical trial – 2,500
μg/day – was higher than the tolerable upper intake level of 1,000 μg.
Folic acid, B12 and iron
A complex interaction occurs between folic acid, vitamin B12, and iron. A deficiency of one may be "masked" by excess of another, so the three must always be in balance.
Folate deficiency
Folate deficiency can be caused by unhealthy diets that do not
include enough vegetables and other folate-rich foods; diseases in which
folates are not well absorbed in the digestive system (such as Crohn's disease or celiac disease);
some genetic disorders that affect levels of folate; and certain
medicines (such as phenytoin, sulfasalazine, or
trimethoprim-sulfamethoxazole). Folate deficiency is accelerated by alcohol consumption, possibly by interference with folate transport.
Folate deficiency may lead to glossitis, diarrhea, depression, confusion, anemia, and fetal neural tube and brain defects. Other symptoms include fatigue, gray hair, mouth sores, poor growth, and swollen tongue. Folate deficiency is diagnosed by analyzing a Complete blood count (CBC) and plasma vitamin B12 and folate levels. A serum folate of 3 μg/L or lower indicates deficiency.
Serum folate level reflects folate status, but erythrocyte folate level
better reflects tissue stores after intake. An erythrocyte folate level
of 140 μg/L or lower indicates inadequate folate status. Serum folate
reacts more rapidly to folate intake than erythrocyte folate.
Increased homocysteine levels suggest tissue folate deficiency, but homocysteine is also affected by vitamin B12 and vitamin B6, renal function, and genetics. One way to differentiate between folate (vitamin B9) deficiency from vitamin B12 deficiency is by testing for methylmalonic acid (MMA) levels. Normal MMA levels indicate folate deficiency and elevated MMA levels indicate vitamin B12 deficiency.
Folate deficiency is treated with supplemental oral folic acid of 400
to 1000 μg per day. This treatment is very successful in replenishing
tissues, even if deficiency was caused by malabsorption. People with
megaloblastic anemia need to be tested for vitamin B12 deficiency before treatment with folic acid, because if the person has vitamin B12 deficiency, folic acid supplementation can remove the anemia, but can also worsen neurologic problems.
Cobalamin deficiency may lead to folate deficiency, which, in turn,
increases homocysteine levels and may result in the development of
cardiovascular disease or birth defects.
Malaria
Some studies show iron–folic acid supplementation in children under five may result in increased mortality due to malaria;
this has prompted the World Health Organization to alter their
iron–folic acid supplementation policies for children in malaria-prone
areas, such as India.
Dietary recommendations
Because
of the difference in bioavailability between supplemented folic acid
and the different forms of folate found in food, the dietary folate
equivalent (DFE) system was established. One DFE is defined as 1 μg of
dietary folate. One μg of folic acid supplement counts as 1.7 μg DFE.
The reason for the difference is that at least 85% of folic acid is
estimated to be bioavailable when taken with food, whereas only about
50% of folate naturally present in food is bioavailable.
| Age | Infants | Children and adults | Pregnant women | Lactating women | ||||
|---|---|---|---|---|---|---|---|---|
| (AI) | (UL) | (RDA) | (UL) | (RDA) | (UL) | (RDA) | (UL) | |
| 0–6 months | 65 | None set | – | – | – | – | – | – |
| 7–12 months | 80 | None set | – | – | – | – | – | – |
| 1–3 years | – | – | 150 | 300 | – | – | – | – |
| 4–8 years | – | – | 200 | 400 | – | – | – | – |
| 9–13 years | – | – | 300 | 600 | – | – | – | – |
| 14–18 | – | – | 400 | 800 | 600 | 800 | 500 | 800 |
| 19+ | – | – | 400 | 1000 | 600 | 1000 | 500 | 1000 |
The U.S. Institute of Medicine (IOM) updated Recommended Dietary Allowances (RDAs) and Tolerable upper intake levels (ULs) for folate in 2001. Collectively the EARs, RDAs, AIs, and ULs are referred to as Dietary Reference Intakes (DRIs). The European Food Safety Authority
(EFSA) refers to the collective set of information as Dietary Reference
Values, with Population Reference Intake (PRI) instead of RDA, and
Average Requirement instead of EAR. AI and UL defined the same as in
United States. For women and men over age 18 the PRI is set at 330
μg/day. PRI for pregnancy is 600 μg/day, for lactation 500 μg/day. For
children ages 1–17 years the PRIs increase with age from 120 to 270
μg/day. These values differ somewhat from the U.S. RDAs.
The United Kingdom's Dietary Reference Value for folate, set by the
Committee on Medical Aspects of Food and Nutrition Policy (COMA) in
1991, is 200 μg/day for adults.
Safety
The risk
of toxicity from folic acid is low, because folate is a water-soluble
vitamin and is regularly removed from the body through urine. One
potential issue associated with high doses of folic acid is that it has a
masking effect on the diagnosis of pernicious anaemia due to vitamin B12 deficiency. An additional concern raised was that low vitamin B12 status in combination with high folic acid intake appeared to increase the risk of cognitive impairment in the elderly.
The IOM sets ULs for vitamins and minerals when evidence is sufficient.
The adult UL of 1000 μg for folate (and lower for children) refers to
folic acid used as a supplement, as no health risks have been associated
with high intake of folate from food sources. The EFSA reviewed the
safety question and agreed with United States that the UL be set at 1000
μg. The Japan National Institute of Health and Nutrition set the adult UL at 1,300 or 1,400 μg depending on age.
Food labeling
For
U.S. food and dietary supplement labeling purposes the amount in a
serving is expressed as a percent of Daily Value (%DV). For folate
labeling purposes 100% of the Daily Value was 400 μg. As of the 27 May
2016 update, it was kept unchanged at 400 μg. A table of the old and new adult Daily Values is provided at Reference Daily Intake.
The original deadline to be in compliance was 28 July 2018, but on 29
September 2017 the FDA released a proposed rule that extended the
deadline to 1 January 2020 for large companies and 1 January 2021 for
small companies.
European Union regulations require that labels declare energy, protein,
fat, saturated fat, carbohydrates, sugars, and salt. Voluntary
nutrients may be shown if present in significant amounts. Instead of
Daily Values, amounts are shown as percent of Reference Intakes (RIs).
For folate, 100% RI was set at 200 μg in 2011.
Sources
The United States Department of Agriculture (USDA), Agricultural Research Service, maintains a food composition database from which folate content in hundreds of foods can be searched as shown in the table. The Food Fortification Initiative lists all countries in the world that conduct fortification programs,
and within each country, what nutrients are added to which foods, and
whether those programs are voluntary or mandatory. In the US, mandatory
fortification of enriched breads, cereals, flours, corn meal, pastas,
rice, and other grain products began in January 1998. As of December 21,
2018, 81 countries required food fortification with one or more
vitamins.
The most commonly fortified vitamin – as used in 62 countries – is
folate; the most commonly fortified food is wheat flour, followed by
maize flour and rice. From country to country, added folic acid amounts
range from 0.4 to 5.1 μg/100 g, but the great majority are in a more
narrow range of 1.5 to 2.5 μg/100 g.
Folate naturally found in food is susceptible to destruction from high
heat cooking, especially in the presence of acidic foods and sauces. It
is soluble in water, and so may be lost from foods boiled in water. For foods that are normally consumed cooked, values in the table are for folate naturally occurring in cooked foods.
| Plant sources | Amount as Folate (μg / 100g) |
|---|---|
| Peanuts | 246 |
| Sunflower seed kernels | 238 |
| Lentils | 181 |
| Chickpeas | 172 |
| Asparagus | 149 |
| Spinach | 146 |
| Lettuce | 136 |
| Peanuts (oil-roasted) | 125 |
| Soy beans | 111 |
| Broccoli | 108 |
| Walnuts | 98 |
| Plant sources | Amount as Folate (μg / 100g) |
|---|---|
| Peanut butter | 92 |
| Hazelnuts | 88 |
| Avocados | 81 |
| Beets | 80 |
| Kale | 65 |
| Bread (not fortified) | 65 |
| Cabbage | 46 |
| Red bell peppers | 46 |
| Cauliflower | 44 |
| Tofu | 29 |
| Potatoes | 28 |
| Animal sources | Amount as Folate (μg / 100g) |
|---|---|
| Chicken liver | 578 |
| Calf liver | 331 |
| Cheese | 20-60 |
| Chicken eggs | 44 |
| Salmon | 35 |
| Chicken | 12 |
| Beef | 12 |
| Pork | 8 |
| Yogurt | 8-11 |
| Milk, whole | 5 |
| Butter, salted | 3 |
Biological roles
The formation of tetrahydrofolate (FH4, also THF) begins when folic acid (F) is reduced to dihydrofolate (DHF) (FH2), which is then reduced to THF. Dihydrofolate reductase catalyses the last step. Vitamin B3 in the form of NADPH is a cofactor for both steps. Thus, hydride is transferred from NADPH to the C6 position of the pteridine ring.
C1-derivatives of folate
Folate is a carrier of C1 groups (methyl, methylene, formyl). Methylene-THF (CH2FH4) is formed from THF by the addition of a methylene bridge from one of three carbon donors: formate, serine, or glycine. For example, serine hydroxymethyltransferase catalyzes the conversion of THF to CH2-THF, extracting the C1 unit from L-serine giving glycine. This reaction provides the largest part of the one-carbon units available to the cell. Methyl tetrahydrofolate (CH3-THF,
or methyl-THF) forms by reduction of methylene-THF by NADPH. Also,
histidine can donate a single carbon to THF to form methenyl-THF. 10-Formyl-THF forms from two pathways. It results from oxidation of methylene-THF. It also forms from formate donating formyl group to THF.
DNA production
Folate
derivatives participate in the biosynthesis of both purines and
pyrimidines. Formyl folate is required for two of the steps in the
biosynthesis of inosine monophosphate, the precursor to GMP and AMP. Methylenetetrahydrofolate donates the C1 center required for the biosynthesis of dTMP (2′-deoxythymidine-5′-phosphate) from dUMP (2′-deoxyuridine-5′-phosphate). The conversion is catalyzed by thymidylate synthase.
Metabolism of folic acid to recycle homocysteine into methionine
Amino acid processing
Methyl-THF converts vitamin B12 to methyl-B12 (methylcobalamin). Methyl-B12 converts homocysteine, in a reaction catalyzed by homocysteine methyltransferase, to methionine. A defect in homocysteine methyltransferase or a deficiency of B12 may lead to a so-called "methyl-trap" of THF, in which THF converts to methyl-THF, causing a deficiency in folate. Thus, a deficiency in B12 can cause accumulation of methyl-THF, mimicking folate deficiency. Methionyl-tRNA formyltransferase catalyzes the conversion of L-methionyl-tRNAfMet into N-formylmethionyl-tRNAfMet.
Folate metabolism
Formiminoglutamic acid is an intermediate in the conversion of histidine to glutamic acid, catalyzed by THF.
Conversion to biologically active derivatives
All the biological functions of folic acid are performed by tetrahydrofolate and other derivatives. Their biological availability to the body depends upon dihydrofolate reductase
action in the liver. This action is unusually slow in humans, being
less than 2% of that in rats (and with an almost-5-fold variation in
enzymatic activity), leading to the accumulation of unmetabolized folic
acid.
It has been suggested this low activity limits the conversion of folic
acid into its biologically active forms "when folic acid is consumed at
levels higher than the Tolerable Upper Intake Level (1 mg/d for
adults)."
Drugs that interfere with folate reactions
A number of drugs interfere with the biosynthesis of folic acid and THF. Among them are the dihydrofolate reductase inhibitors such as trimethoprim, pyrimethamine, and methotrexate; the sulfonamides (competitive inhibitors of 4-aminobenzoic acid in the reactions of dihydropteroate synthetase). Valproic acid,
one of the most commonly prescribed anticonvulsants that is also used
to treat certain psychological conditions, is a known inhibitor of folic
acid, and as such, has been shown to cause neural tube defects and cases of spina bifida
and cognitive impairment in the newborn. Because of this considerable
risk, those mothers who must continue to use valproic acid or its
derivatives during pregnancy to control their condition (as opposed to
stopping the drug or switching to another drug or to a lesser dose)
should take folic acid supplements under the direction and guidance of
their health care providers.
Food fortification
Folic acid fortification is a process where folic acid is
added to flour with the intention of promoting public health through
increasing blood folate levels in the populace. In the U.S., food is
fortified with folic acid, only one of the many naturally occurring
forms of folate, and a substance contributing only a minor amount to the
folates in natural foods. After the discovery of the link between insufficient folic acid and neural tube defects, governments and health organizations worldwide made recommendations concerning folic acid supplementation
for women intending to become pregnant. Because the neural tube closes
in the first four weeks of gestation, often before many women even know
they are pregnant, many countries in time decided to implement mandatory
food fortification programs. A meta-analysis of global birth prevalence
of spina bifida showed that when mandatory fortification was compared
to countries with voluntary fortification or no fortification program,
there was a 30% reduction in live births with spina bifida. Folic acid is added to grain products in more than 80 countries, and these fortified products make up a significant source of the population's folate intake. Fortification is controversial, with issues having been raised concerning individual liberty, as well as the health concerns described in the Toxicity
section. In the U.S., there is concern that the federal government
mandates fortification but does not provide monitoring of potential
undesirable effects of fortification. The Food Fortification Initiative lists all countries in the world that conduct fortification programs,
and within each country, what nutrients are added to which foods. As
of December 21, 2018, 81 countries required food fortification with one
or more vitamins. The most commonly fortified vitamin – as used in 62 countries – is folate; the most commonly fortified food is wheat flour.
Australia and New Zealand
Australia and New Zealand jointly agreed to wheat flour fortification through the Food Standards Australia New Zealand in 2007. The requirement was set at 135 µg of folate per 100 g of bread. Australia implemented the program in 2009.
New Zealand was also planning to fortify bread (excluding organic and
unleavened varieties) starting in 2009, but then opted to wait until
more research was done. The Association of Bakers and the Green Party had opposed mandatory fortification, describing it as "mass medication." Food Safety Minister Kate Wilkinson
reviewed the decision to fortify in July 2009, citing as reasons to
oppose claims for links between over consumption of folate with
increased risk of cancer.
In 2012 the delayed mandatory fortification program was revoked and
replaced by a voluntary program, with the hope of achieving a 50% bread
fortification target.
Canada
According
to a Canadian survey, 58% of women said they took a folic acid
containing multivitamin or a folic acid supplement as early as three
months before becoming pregnant. Women in higher income households and
with more years of school education were more likely to use folic acid
supplements before pregnancy, as were women with planned pregnancies and
those over the age of 25. Canadian public health efforts focused on
promoting awareness of the importance of folic acid supplementation for
all women of childbearing age and decreasing socio-economic inequalities
by providing practical folic acid support to vulnerable groups of
women. Folic acid food fortification became mandatory in 1998, with the fortification of 150 µg of folic acid per 100 grams of enriched flour and uncooked cereal grains. The results of folic acid fortification on the rate of neural tube defects in Canada
have been positive, showing a 46% reduction in prevalence of NTDs; the
magnitude of reduction was proportional to the prefortification rate of
NTDs, essentially removing geographical variations in rates of NTDs seen
in Canada before fortification.
United Kingdom
While the Food Standards Agency recommended folic acid fortification, and wheat flour is fortified with iron,
folic acid fortification of wheat flour is allowed voluntarily rather
than required. A 2018 review by authors based in the United Kingdom
strongly recommended that mandatory fortification be reconsidered as a
means of reducing the risk of neural tube defects.
United States
In the United States many grain products are fortified with folic acid.
In 1996, the United States Food and Drug Administration
(FDA) published regulations requiring the addition of folic acid to
enriched breads, cereals, flours, corn meals, pastas, rice, and other
grain products.
This ruling took effect on 1 January 1998, and was specifically targeted
to reduce the risk of neural tube birth defects in newborns. There were concerns expressed that the amount of folate added was insufficient.
The fortification program was expected to raise a person's folic acid intake level by 70–130 µg/day; however, an increase of almost double that amount was actually observed. This could be from the fact that many foods are over-fortified by 160–175% over the required amount. Much of the elder population take supplements
that add 400 µg to their daily folic acid intake. This is a concern
because 70–80% of the population have detectable levels of unmetabolized
folic acid in their blood,
a consequence of folic acid supplementation and fortification, and high
intakes are thought to accelerate the growth of preneoplastic lesions
that could lead to cancer.
The U.S. National Center for Health Statistics conducts biannual
National Health and Nutrition Examination Survey (NHANES) to assess the
health and nutritional status of adults and children in the United
States. Some results are reported as What We Eat In America. The
2013–2014 survey reported that for adults ages 20 years and older, men
consumed on average of 249 μg/d folate from food plus 207/d μg of folic
acid from consumption of fortified foods, for a combined total of 601
μg/d of dietary folate equivalents (DFEs; because each microgram of
folic acid counts as 1.7 μg of food folate). For women, the values are
199, 153 and 459 μg/d, respectively. This means that fortification led
to a bigger increase in folic acid intake than first projected, and that
more than half the adults are consuming more than the RDA of 400 μg (as
DFEs). Even so, fewer than half of pregnant women are exceeding the
pregnancy RDA of 600 μg/d.
The Centers for Disease Control and Prevention in Atlanta, Georgia
used data from 23 birth defect registries covering about half of United
States births, and extrapolated their findings to the rest of the
country. These data indicate that since the addition of folic acid in
grain-based foods as mandated by the FDA, the rate of neural tube
defects dropped by 25% in the United States.
Before folic acid fortification, about 4,100 pregnancies were affected
by a neural tube defect each year in the United States. After
fortification, this number declined to around 3,000.
History
In the 1920s, scientists believed folate deficiency and anemia were the same condition. In 1931, researcher Lucy Wills made a key observation that led to the identification of folate as the nutrient required to prevent anemia during pregnancy. Wills demonstrated that anemia could be reversed with brewer's yeast.
In the late 1930s, folate was identified as the corrective substance in
brewer's yeast. It was first isolated via extraction from spinach leaves by Herschel K. Mitchell, Esmond E. Snell, and Roger J. Williams in 1941.
Bob Stokstad isolated the pure crystalline form in 1943, and was able
to determine its chemical structure while working at the Lederle
Laboratories of the American Cyanamid Company.
This historical research project, of obtaining folic acid in a pure
crystalline form in 1945, was done by the team called the "folic acid
boys," under the supervision and guidance of Director of Research Dr. Yellapragada Subbarow, at the Lederle Lab, Pearl River, NY.
This research subsequently led to the synthesis of the antifolate aminopterin, the first-ever anticancer drug, the clinical efficacy was proven by Sidney Farber in 1948. In the 1950s and 1960s, scientists began to discover the biochemical mechanisms of action for folate. In 1960, experts first linked folate deficiency to neural tube defects.
In the late 1990s, U.S. scientists realized, despite the availability
of folate in foods and in supplements, there was still a challenge for
people to meet their daily folate requirements, which is when the US
implemented the folate fortification program.