| |

| |
| Names | |
|---|---|
| IUPAC name
2-Amino-4-sulfanylbutanoic acid
| |
| Identifiers | |
3D model (JSmol)
|
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| ECHA InfoCard | 100.006.567 |
| EC Number |
|
| KEGG | |
PubChem CID
|
|
| UNII |
|
| Properties | |
| C4H9NO2S | |
| Molar mass | 135.18 g/mol |
| Appearance | White crystalline powder |
| Melting point | 234–235 °C (453–455 °F; 507–508 K)[2] (decomposes) |
| soluble | |
| log P | -2.56 [1] |
| Acidity (pKa) | 2.25 [1] |
| Hazards | |
| GHS pictograms | 
|
| GHS Signal word | Warning |
| H302 | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
Homocysteine /ˌhoʊmoʊˈsɪstiːn/ is a non-proteinogenic α-amino acid. It is a homologue of the amino acid cysteine, differing by an additional methylene bridge (-CH2-). It is biosynthesized from methionine by the removal of its terminal Cε methyl group. Homocysteine can be recycled into methionine or converted into cysteine with the aid of certain B-vitamins.
A high level of homocysteine in the blood (hyperhomocysteinemia) makes a person more prone to endothelial cell injury, which leads to inflammation in the blood vessels, which in turn may lead to atherogenesis, which can result in ischemic injury. Hyperhomocysteinemia is therefore a possible risk factor for coronary artery disease. Coronary artery disease occurs when an atherosclerotic plaque blocks blood flow to the coronary arteries, which supply the heart with oxygenated blood.
Hyperhomocysteinemia has been correlated with the occurrence of blood clots, heart attacks and strokes, though it is unclear whether hyperhomocysteinemia is an independent risk factor for these conditions. Hyperhomocysteinemia has also been associated with early pregnancy loss and with neural tube defects.
Structure
Zwitterionic form of (S)-homocysteine (left) and (R)-homocysteine (right)
Homocysteine exists at neutral pH values as a zwitterion.
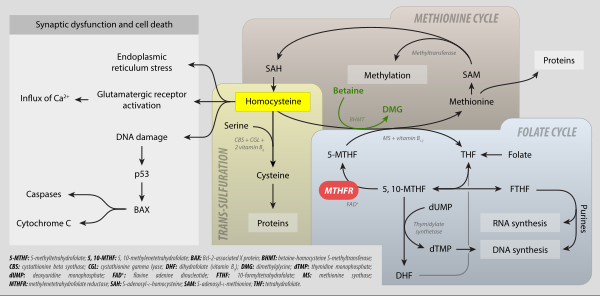
Biosynthesis and biochemical roles
Two
of homocysteine's main biochemical roles. (Homocysteine is seen in the
left middle of the image.) It can be synthesized from methionine and
then converted back to methionine via the SAM cycle or used to create
cysteine and alpha-ketobutyrate.
Homocysteine is not obtained from the diet. Instead, it is biosynthesized from methionine via a multi-step process. First, methionine receives an adenosine group from ATP, a reaction catalyzed by S-adenosyl-methionine synthetase, to give S-adenosyl methionine (SAM). SAM then transfers the methyl group to an acceptor molecule, (e.g., norepinephrine as an acceptor during epinephrine synthesis, DNA methyltransferase as an intermediate acceptor in the process of DNA methylation). The adenosine is then hydrolyzed to yield L-homocysteine. L-Homocysteine has two primary fates: conversion via tetrahydrofolate (THF) back into L-methionine or conversion to L-cysteine.
Biosynthesis of cysteine
Mammals biosynthesize the amino acid cysteine via homocysteine. Cystathionine β-synthase catalyses the condensation of homocysteine and serine to give cystathionine. This reaction uses pyridoxine (vitamin B6) as a cofactor. Cystathionine γ-lyase
then converts this double amino acid to cysteine, ammonia, and
α-ketobutyrate. Bacteria and plants rely on a different pathway to
produce cysteine, relying on O-acetylserine.
MTHFR metabolism: folate cycle, methionine cycle, trans-sulfuration and hyperhomocysteinemia. 5-MTHF: 5-methyltetrahydrofolate; 5,10-methyltetrahydrofolate; BAX: Bcl-2-associated X protein; BHMT: betaine-homocysteine S-methyltransferase; CBS: cystathionine beta synthase; CGL: cystathionine gamma-lyase; DHF: dihydrofolate (vitamin B9); DMG: dimethylglycine; dTMP: thymidine monophosphate; dUMP: deoxyuridine monophosphate; FAD+ flavine adenine dicucleotide; FTHF: 10-formyltetrahydrofolate; MS: methionine synthase; MTHFR: mehtylenetetrahydrofolate reductase; SAH: S-adenosyl-L-homocysteine; SAME: S-adenosyl-L-methionine; THF: tetrahydrofolate.
Methionine salvage
Homocysteine can be recycled into methionine. This process uses N5-methyl tetrahydrofolate as the methyl donor and cobalamin (vitamin B12)-related enzymes. More detail on these enzymes can be found in the article for methionine synthase.
Other reactions of biochemical significance
Homocysteine can cyclize to give homocysteine thiolactone, a five-membered heterocycle. Because of this "self-looping" reaction, homocysteine-containing peptides tend to cleave themselves by reactions generating oxidative stress.
Homocysteine also acts as an allosteric antagonist at Dopamine D2 receptors. It has been proposed that both homocysteine and its thiolactone may have played a significant role in the appearance of life on the early Earth.
Homocysteine levels
Total plasma homocysteine
Homocysteine levels are typically higher in men than women, and increase with age.
Common levels in Western populations are 10 to 12 μmol/L, and
levels of 20 μmol/L are found in populations with low B-vitamin intakes
or in the elderly (e.g., Rotterdam, Framingham).
It is decreased with methyl folate trapping, where it is
accompanied by decreased methylmalonic acid, increased folate and a
decrease in formiminoglutamic acid. This is the opposite of MTHFR C677T mutations, which result in an increase in homocysteine.
| Sex | Age | Lower limit |
Upper limit |
Unit | Elevated | Therapeutic target |
| Female | 12–19 years | 3.3 | 7.2 | μmol/L | > 10.4 μmol/L or > 140 μg/dl |
< 6.3 μmol/L or < 85 μg/dL |
| 45 | 100 | μg/dL | ||||
| >60 years | 4.9 | 11.6 | μmol/L | |||
| 66 | 160 | μg/dL | ||||
| Male | 12–19 years | 4.3 | 9.9 | μmol/L | > 11.4 μmol/L or > 150 μg/dL | |
| 60 | 130 | μg/dL | ||||
| >60 years | 5.9 | 15.3 | μmol/L | |||
| 80 | 210 | μg/dL |
The ranges above are provided as examples only; test results should
always be interpreted using the range provided by the laboratory that
produced the result.
Elevated homocysteine
Abnormally high levels of homocysteine in the serum, above 15 µmol/L, are a medical condition called hyperhomocysteinemia. This has been claimed to be a significant risk factor for the development of a wide range of diseases, including thrombosis, neuropsychiatric illness, and fractures.
It is also found to be associated with microalbuminuria which is a
strong indicator of the risk of future cardiovascular disease and renal
dysfunction. Vitamin B12 deficiency, when coupled with high serum folate levels, has been found to increase overall homocysteine concentrations as well.